In the early days of medicine, diagnosis relied almost entirely on observation, intuition, and trial and error. Ancient healers would study a patient’s pulse, examine their eyes, ask about dreams or superstitions, and sometimes even rely on rituals or celestial readings. As centuries passed, the practice of medicine grew increasingly empirical and systematic—gaining clarity through dissection, data, and the scientific method.
Now, in the 21st century, we find ourselves on the brink of yet another transformation. A technological revolution is unfolding, and at the center of it is artificial intelligence (AI). What once belonged in the realm of science fiction—computers diagnosing cancer, algorithms predicting heart attacks, machines reading medical images with superhuman accuracy—is now rapidly becoming reality.
AI is not just a tool in modern healthcare; it’s poised to become an indispensable partner in diagnosis. The very act of identifying disease is undergoing a metamorphosis, and with it, the future of medicine itself.
What Is AI in the Context of Healthcare?
Before diving into the role of AI in diagnosing diseases, it’s important to define what we mean by AI in this context. Artificial intelligence, in its broadest sense, refers to the ability of machines to perform tasks that typically require human intelligence. This includes learning from data, recognizing patterns, making decisions, and adapting over time.
In healthcare, AI takes many forms. It powers natural language processing systems that can read clinical notes, machine learning algorithms that detect anomalies in medical images, chatbots that help triage symptoms, and predictive models that forecast disease outbreaks or patient deterioration.
Crucially, when we talk about AI diagnosing diseases, we’re usually referring to machine learning (ML) and deep learning (DL)—subsets of AI that involve training algorithms on large datasets so they can learn to recognize complex patterns. Just as a doctor learns to distinguish between a benign mole and a malignant melanoma through experience, an AI system learns by being shown thousands or millions of examples.
The difference? AI never forgets. It doesn’t get tired. It doesn’t bring bias or mood into the clinic. And it can process in seconds what might take a human hours—or years—to learn.
Diagnosing with Data: The Foundation of AI’s Power
Every diagnosis begins with data: a symptom described by a patient, a blood test result, an X-ray image, a genetic sequence. Modern medicine is awash in data, more than any single doctor could hope to digest.
Enter AI.
The strength of AI lies in its ability to sift through colossal volumes of medical information—far beyond the capacity of the human brain—and find patterns, correlations, and anomalies. It’s like having a doctor with perfect memory, instant access to every medical paper ever written, and the ability to read and compare thousands of patient records simultaneously.
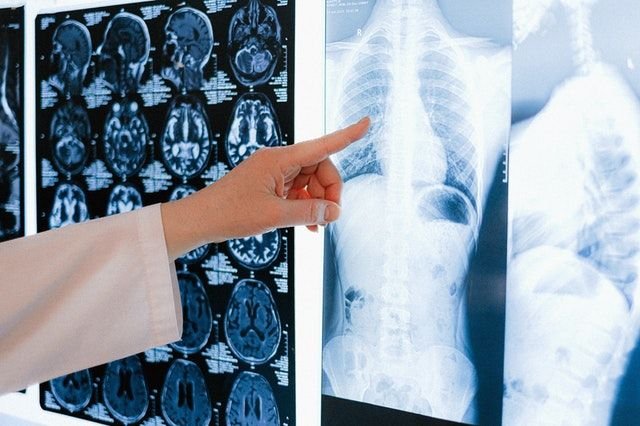
For example, in imaging-heavy specialties like radiology and pathology, AI has shown remarkable accuracy in detecting early-stage cancers, fractures, and brain lesions. It can scan CT scans, MRIs, or digital pathology slides with such precision that it often matches or even exceeds the performance of experienced specialists.
And this isn’t limited to images. AI can analyze electronic health records (EHRs), genomic data, lab test results, and even spoken language to make diagnostic suggestions. It turns raw data into actionable insights—and does so in real time.
AI and Radiology: Seeing What Humans Might Miss
One of the earliest and most successful applications of AI in disease diagnosis has been in radiology. Every day, radiologists interpret hundreds of images—chest X-rays, mammograms, CT scans, MRIs—looking for signs of disease that may be subtle, complex, or easily overlooked.
AI, especially through deep learning, has become a powerful ally in this domain. By training on massive image datasets, AI models can learn to detect everything from lung nodules to brain tumors with exceptional accuracy.
For instance, algorithms have been developed that can spot early signs of breast cancer in mammograms better than many seasoned radiologists. Others can detect intracranial hemorrhages, classify types of pneumonia, or identify musculoskeletal injuries.
But AI doesn’t just aim to replace the radiologist. Instead, it acts as a second set of eyes—helping flag images for review, prioritizing urgent cases, and reducing diagnostic errors. In many clinical settings, AI now acts as a triage assistant, ensuring that the most critical cases are reviewed first.
Pathology and Pattern Recognition
Like radiologists, pathologists spend their days examining samples under microscopes—searching for patterns that suggest disease. Whether it’s a cancerous cell in a tissue biopsy or an abnormal blood smear, diagnosis often depends on keen observation.
AI thrives in this pattern-rich environment. Trained on thousands of digitized pathology slides, AI can learn to distinguish between healthy and diseased cells with incredible nuance. Some systems are already capable of grading tumors, predicting genetic mutations based on visual features, and even forecasting patient outcomes.
The implications are profound. In low-resource settings where pathologists are scarce, AI could bring expert-level diagnosis to places where it was previously out of reach. And even in world-class hospitals, it can increase speed, consistency, and accuracy.
Dermatology: Diagnosing Through Photos
One of the most visually driven specialties, dermatology is another field where AI has made significant strides.
Using deep convolutional neural networks (CNNs), researchers have built models that can analyze skin lesions from photographs and diagnose conditions like melanoma, basal cell carcinoma, or psoriasis. In several studies, these models have matched or surpassed the diagnostic performance of dermatologists.
Imagine a patient in a remote village with a smartphone. They snap a photo of a mole and upload it to an app powered by AI. Within moments, they get a risk assessment: likely benign, or needs biopsy. This kind of tool doesn’t just democratize healthcare—it has the potential to save lives.
Of course, these tools are not without limitations. Lighting, skin tone variability, and image quality can affect accuracy. But with each iteration and each new dataset, these systems improve, becoming more robust and inclusive.
Cardiology: Listening to the Heart with Machines
Cardiovascular disease remains the leading cause of death worldwide. Diagnosing heart conditions can be complex, requiring interpretation of ECGs, echocardiograms, blood tests, and patient history.
AI is now being trained to read ECGs with extraordinary precision—detecting arrhythmias, predicting sudden cardiac death, or identifying early signs of heart failure that even expert cardiologists might miss.
In echocardiography, AI can assist in image acquisition, automatically measure heart function, and flag abnormalities in real time. Some models have been trained to identify subtle cardiac features that correlate with outcomes like stroke risk or heart attack probability.
The future may see wearable devices, powered by AI, that constantly monitor heart rhythms and alert users or doctors to any anomalies long before symptoms appear.
Ophthalmology: AI with Vision
Eye diseases such as diabetic retinopathy, macular degeneration, and glaucoma can be devastating but are often preventable with early detection.
AI is already being used to analyze retinal scans and flag early warning signs. In fact, the first FDA-approved AI diagnostic tool for autonomous use in medicine was IDx-DR—a system that detects diabetic retinopathy from retinal images without needing a doctor to interpret the result.
These tools are especially impactful in areas lacking ophthalmologists, bringing expert-level screening to primary care offices or mobile clinics. The role of AI here is not to replace eye doctors but to extend their reach, catching disease before vision is lost.
Predictive Diagnostics: Seeing the Future Before It Happens
One of the most exciting—and potentially disruptive—roles of AI in medicine is predictive diagnostics.
By analyzing large datasets from EHRs, lab tests, genomics, lifestyle data, and even social determinants of health, AI can predict who is likely to get sick before symptoms appear.
Imagine knowing that a patient is at high risk of sepsis six hours before their vitals change—or predicting which patients with mild COVID-19 will deteriorate and need ICU care. These early warnings can prompt preemptive action, saving lives and reducing the burden on healthcare systems.
Predictive models are being developed for diabetes, cancer recurrence, mental health crises, and even suicide risk. Some hospitals already use AI to identify high-risk patients upon admission, guiding resource allocation and care strategies.
Genetic and Molecular Diagnosis
Genomics has revolutionized our understanding of disease. AI is now being used to interpret complex genomic data—identifying mutations that drive cancer, predicting responses to targeted therapies, and uncovering rare genetic disorders.
These systems can process vast amounts of sequence data, cross-reference it with medical literature, and suggest diagnoses or treatments personalized to the patient’s DNA.
In the near future, whole-genome sequencing at birth could be analyzed by AI to predict health risks, tailor preventative care, and guide lifelong medical decisions.
AI and Mental Health: Listening Between the Lines
Diagnosing mental health conditions is notoriously subjective. There are no blood tests for depression or brain scans that diagnose anxiety. But AI is beginning to help fill this gap.
Natural language processing models can analyze speech, writing, social media posts, or voice patterns to detect linguistic markers of mood disorders. AI systems have been trained to recognize depression, PTSD, and even early signs of schizophrenia by listening to how people talk—long before a crisis point is reached.
Mobile apps and virtual therapists are also incorporating AI to track user behavior, provide support, and escalate care when needed. While human connection remains central to mental health, AI can offer scalable, round-the-clock support in a world with rising mental health needs and not enough providers.
Ethical Challenges: Trust, Bias, and Responsibility
As promising as AI is, it comes with serious ethical concerns.
One of the most pressing is bias. AI learns from data, and if that data reflects historical inequities, the AI will reproduce them. For instance, if a diagnostic model is trained mostly on white male patients, it may perform poorly for women or people of color. This can lead to misdiagnosis, underdiagnosis, or lack of access to care.
Transparency is another challenge. Many AI systems operate as “black boxes”—we know what decision they made but not why. In medicine, where accountability and explanation are essential, this can be problematic.
There are also questions of consent, privacy, and data ownership. Who controls the medical data used to train these systems? Who is responsible if the AI makes a mistake?
AI in medicine must be held to high ethical and regulatory standards—not only to ensure safety but to build trust among patients and providers.
The Human-AI Partnership: A New Model of Care
Despite the hype, AI will not replace doctors. Rather, it will empower them.
AI can handle the data deluge, flag abnormalities, prioritize tasks, and suggest diagnoses—but human physicians bring empathy, intuition, and holistic judgment. They consider context, values, and patient preferences in a way no machine can replicate.
The future of diagnosis will be human-AI collaboration: doctors making faster, smarter, more personalized decisions with the help of intelligent tools. This partnership could reduce burnout, increase access, improve outcomes, and transform healthcare delivery across the globe.
Conclusion: The Algorithm Will See You Now
Artificial intelligence is reshaping how we diagnose disease—not just in academic labs or elite hospitals, but in real-world clinics, mobile apps, and global health programs. From reading X-rays to predicting cardiac events, from analyzing speech patterns to detecting tumors, AI is proving to be a powerful diagnostic ally.
Yet, the heart of medicine remains human. AI may read a scan or highlight a risk, but it’s the doctor who will explain the result, guide the patient, and walk with them through fear, hope, and healing.
The question is not whether AI will be a part of diagnosing disease—it already is. The question is how we will harness its power ethically, wisely, and inclusively.
Because the best medicine isn’t man or machine.
It’s both.