In the modern age of digital calendars, contraceptive pills, and instant health apps, it’s easy to forget that the most intricate and intelligent fertility tracker has always been within us. Long before the invention of hormonal birth control, women relied on deep knowledge of their bodies to understand when conception was most likely—or least likely—to occur. This knowledge was passed quietly between mothers, daughters, and midwives, wrapped in tradition but often lacking scientific clarity.
Today, that tradition has been reborn in a new form: fertility awareness methods (FAMs), backed by decades of research in reproductive biology. These are not mystical guesses or folklore remedies, but systems rooted in measurable physiological changes—changes that can be learned, tracked, and understood by anyone willing to observe their own patterns.
Natural family planning, in its modern scientific form, stands at the crossroads of empowerment and responsibility. It invites individuals to work with their biology rather than override it. Whether the goal is to avoid pregnancy, achieve it, or simply understand one’s reproductive health more deeply, fertility awareness offers a path built on trust—trust in one’s own observations, in the science of the menstrual cycle, and in the body’s ability to communicate its rhythms.
The Menstrual Cycle: Nature’s Intricate Symphony
The foundation of fertility awareness is the menstrual cycle—an exquisite interplay of hormones, organs, and timing that orchestrates the possibility of new life. The average cycle spans about twenty-eight days, though “average” is a statistical midpoint; healthy cycles may be shorter or longer.
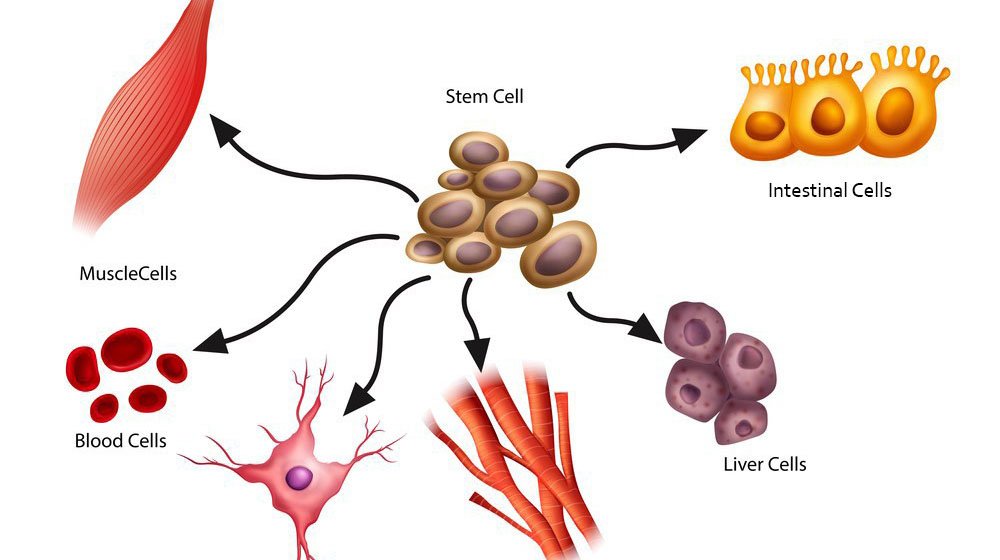
The cycle begins with menstruation, the visible shedding of the uterine lining. Beneath the surface, the ovaries are already preparing for the next potential ovulation. Follicle-stimulating hormone (FSH) encourages the growth of several ovarian follicles, each containing an immature egg. Estrogen levels begin to rise, thickening the endometrium and signaling the body that fertility is on the horizon.
Around the midpoint of the cycle, a surge in luteinizing hormone (LH) triggers ovulation—the release of a mature egg into the fallopian tube. This is the moment of peak fertility. The egg itself lives for only about twenty-four hours, but sperm can survive in the female reproductive tract for up to five days, creating a fertile window that extends beyond the day of ovulation itself.
If the egg meets sperm and is fertilized, the body shifts into the luteal phase, producing progesterone to prepare the uterus for implantation. If no fertilization occurs, hormone levels drop, the uterine lining breaks down, and the cycle begins again.
This dance of hormones creates observable changes in the body—changes in basal body temperature, cervical mucus, and even subtle sensations—that fertility awareness methods use as reliable signposts.
Understanding the Fertile Window
Fertility awareness hinges on one principle: pregnancy can occur only when live sperm meet a viable egg. This seems straightforward, but the challenge lies in identifying the narrow window when this can happen.
Because sperm can survive for several days and the egg only for one, the fertile window typically spans about six days: the five days before ovulation and the day of ovulation itself. Outside of this window, conception is biologically impossible.
The difficulty is that ovulation does not occur on the same calendar date every cycle. Stress, illness, changes in routine, and natural biological variation can shift ovulation earlier or later. Fertility awareness methods work by detecting the body’s own early warning signs of fertility, allowing individuals to adjust their understanding in real time rather than relying on fixed predictions.
The Science of Cervical Mucus
One of the most reliable indicators of fertility is cervical mucus, a substance whose texture and appearance shift in response to hormonal changes. Under the influence of estrogen in the days before ovulation, cervical glands produce mucus that is clear, slippery, and stretchy—often compared to raw egg whites. This fertile-type mucus is a biological masterpiece, designed to protect and nourish sperm, guiding them toward the egg.
After ovulation, progesterone transforms the mucus into a thicker, stickier substance that acts as a barrier, blocking sperm from entering the uterus. By observing and recording the daily changes in mucus, an individual can identify when fertility begins and when it ends in each cycle.
Learning to read these signs takes practice. At first, patterns may seem confusing, especially for those who have spent years ignoring or suppressing these natural changes. But over time, the patterns become as clear as the seasons—predictable not in their exact timing, but in their recurring nature.
Tracking Basal Body Temperature
Another key tool in fertility awareness is the measurement of basal body temperature (BBT)—the body’s lowest resting temperature, taken immediately upon waking. After ovulation, the hormone progesterone causes a slight but measurable increase in BBT, usually about 0.3 to 0.6 degrees Celsius.
This temperature rise confirms that ovulation has already occurred, allowing individuals to identify the end of the fertile window. While BBT tracking cannot predict ovulation ahead of time, it is invaluable for confirming its occurrence, especially when combined with cervical mucus observations.
Accurate tracking requires consistency: the temperature should be taken at the same time each morning before getting out of bed, using a thermometer sensitive enough to detect small changes. Over several cycles, the BBT pattern becomes an unmistakable signature of the body’s rhythm.
The Hormonal Blueprint of Awareness
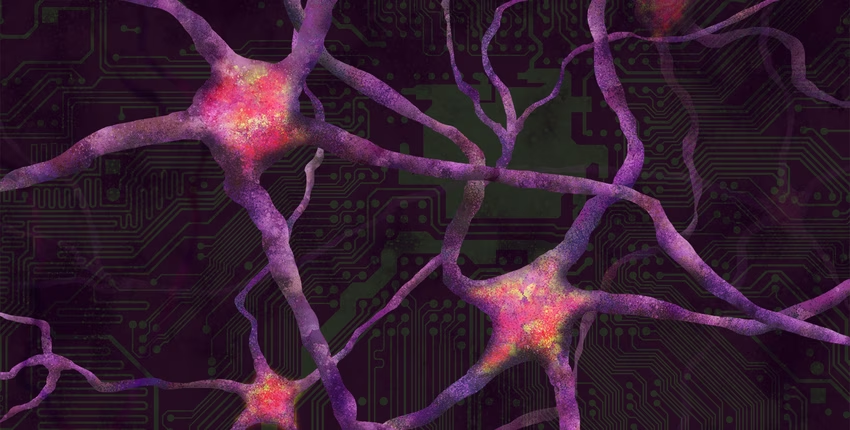
Beyond mucus and temperature, modern fertility awareness can also incorporate other biological markers. Some methods use ovulation predictor kits (OPKs) to detect the LH surge, providing an additional layer of confirmation. Others observe secondary signs such as changes in cervical position, breast tenderness, or even shifts in mood and energy levels—all of which reflect the hormonal tides of the cycle.
These methods are not based on vague intuition; they are grounded in endocrinology and physiology. Estrogen, progesterone, LH, and FSH are not abstract concepts but chemical messengers whose effects can be observed in real time. By mapping these effects, fertility awareness transforms invisible hormonal changes into tangible data.
Effectiveness and Responsibility
One of the most common misconceptions about fertility awareness is that it is inherently unreliable. This misunderstanding often arises from confusing it with the outdated “calendar method,” which predicts fertile days solely based on past cycle lengths.
In reality, when practiced correctly and consistently, modern fertility awareness methods can be highly effective. Studies have shown that some methods, when taught and applied precisely, can rival the effectiveness of hormonal contraceptives in preventing pregnancy.
However, the key word is “correctly.” FAMs require daily observation, accurate record-keeping, and disciplined decision-making. They are not a passive form of birth control; they demand engagement and responsibility. For some, this is a drawback. For others, it is a source of empowerment, fostering a deeper connection to one’s body and reproductive choices.
Beyond Contraception: Achieving Pregnancy
While much of the conversation around fertility awareness focuses on avoiding pregnancy, the same methods can be used to increase the likelihood of conception. For couples struggling with infertility, learning to identify the fertile window with precision can make the difference between months of disappointment and a positive test.
By pinpointing ovulation, FAMs allow couples to time intercourse for the days when conception is most likely. This is particularly valuable for those with irregular cycles, where ovulation can be unpredictable. In this way, fertility awareness becomes not only a method of family planning but also a tool for fertility support.
Emotional and Cultural Dimensions
Fertility awareness is not purely a biological practice; it is also deeply personal and, for some, spiritual. In a world where reproductive health is often medicalized, FAMs offer a way to reclaim agency over one’s fertility without external intervention.
For many, this fosters a profound sense of bodily autonomy and trust. The daily practice of observation becomes a form of mindfulness, attuning the individual to subtle changes in sensation, energy, and mood. Couples practicing together may experience a new level of communication and cooperation, as decisions about intimacy are made jointly in light of the fertile window.
However, this intimacy with one’s fertility can also bring challenges. For those avoiding pregnancy, the fertile phase may mean refraining from sex or choosing non-penetrative intimacy—choices that require negotiation, patience, and mutual understanding. These emotional dynamics are as much a part of the practice as the physical observations.
Fertility Awareness in the Digital Age
In the 21st century, fertility awareness has been transformed by technology. Smartphone apps, wearable temperature sensors, and digital fertility monitors promise to simplify tracking, automate charting, and even predict fertile days.
While these tools can be helpful, they are only as accurate as the data entered—and no algorithm can replace direct awareness of the body’s own signs. Experts caution against outsourcing fertility entirely to an app without learning the underlying biology. The ideal approach blends technology with personal observation, using digital tools to support rather than replace human insight.
Medical Insights from Fertility Tracking
An often-overlooked benefit of fertility awareness is its role in overall health monitoring. The menstrual cycle is a vital sign, reflecting the body’s hormonal balance, nutritional status, and stress levels. Changes in cycle length, mucus patterns, or luteal phase length can signal underlying health issues such as thyroid disorders, polycystic ovary syndrome (PCOS), or luteal phase defects.
For healthcare providers trained in fertility awareness, a patient’s charts can offer valuable diagnostic clues. This approach reframes the cycle not as an inconvenience to be suppressed, but as a window into overall wellness.
The Future of Natural Family Planning
As interest in holistic and body-centered health grows, fertility awareness methods are likely to become increasingly mainstream. Education is key: when people understand the science behind their cycles, they are better equipped to make informed reproductive choices.
In medical schools, midwifery programs, and public health initiatives, there is a renewed push to teach fertility literacy—not merely as a contraceptive option, but as a fundamental aspect of reproductive health. The future may see FAMs integrated alongside other methods in a truly informed-choice framework, where individuals can weigh the benefits and responsibilities of each.
A Lifelong Conversation with the Body
Fertility awareness is not a temporary skill but a lifelong conversation with the body. Even beyond the childbearing years, the patterns of the cycle offer insights into hormonal health, perimenopause, and overall well-being.
It is a practice rooted in observation, patience, and respect—qualities that extend far beyond reproduction. To engage in fertility awareness is to acknowledge that our bodies are not random or chaotic, but rhythmic, intelligent, and worthy of our attention.
In the end, the science behind natural family planning is more than data and charts; it is a meeting point between biology and self-knowledge. It asks us to slow down, to listen, and to trust that the body’s quiet signals are worth hearing.