For decades, doctors have taught that high blood pressure—also known as hypertension—starts in the kidneys and blood vessels. The kidneys regulate fluid balance, and blood vessels respond by tightening or relaxing, which sets the stage for blood pressure levels. But now, a groundbreaking study led by McGill University’s Masha Prager-Khoutorsky suggests another, often overlooked culprit: the brain.
This new research shows that eating too much salt doesn’t just affect the kidneys—it can spark inflammation in the brain itself, which in turn drives blood pressure higher. The findings, published in the journal Neuron, are rewriting the story of hypertension and pointing scientists toward brand-new ways of treating it.
“High blood pressure can originate in the brain,” says Prager-Khoutorsky, an associate professor in McGill’s Department of Physiology. “This opens the door to treatments that act on the brain rather than just the kidneys or blood vessels.”
The Silent Killer Affecting Millions
Hypertension has been called the “silent killer” for a reason. Often symptomless, it slowly wears down the body, increasing the risk of heart disease, strokes, kidney damage, and even dementia. Globally, it contributes to around 10 million deaths each year.
The condition is especially common in older adults: nearly two out of three people over the age of 60 live with hypertension. While medications exist to control it, about one in three patients don’t respond well to standard treatments. These are often the most difficult cases, where even lifestyle changes and multiple drugs fail to bring blood pressure under control. For them, the brain may hold the missing piece of the puzzle.
Salt, the Brain, and a Surprising Reaction
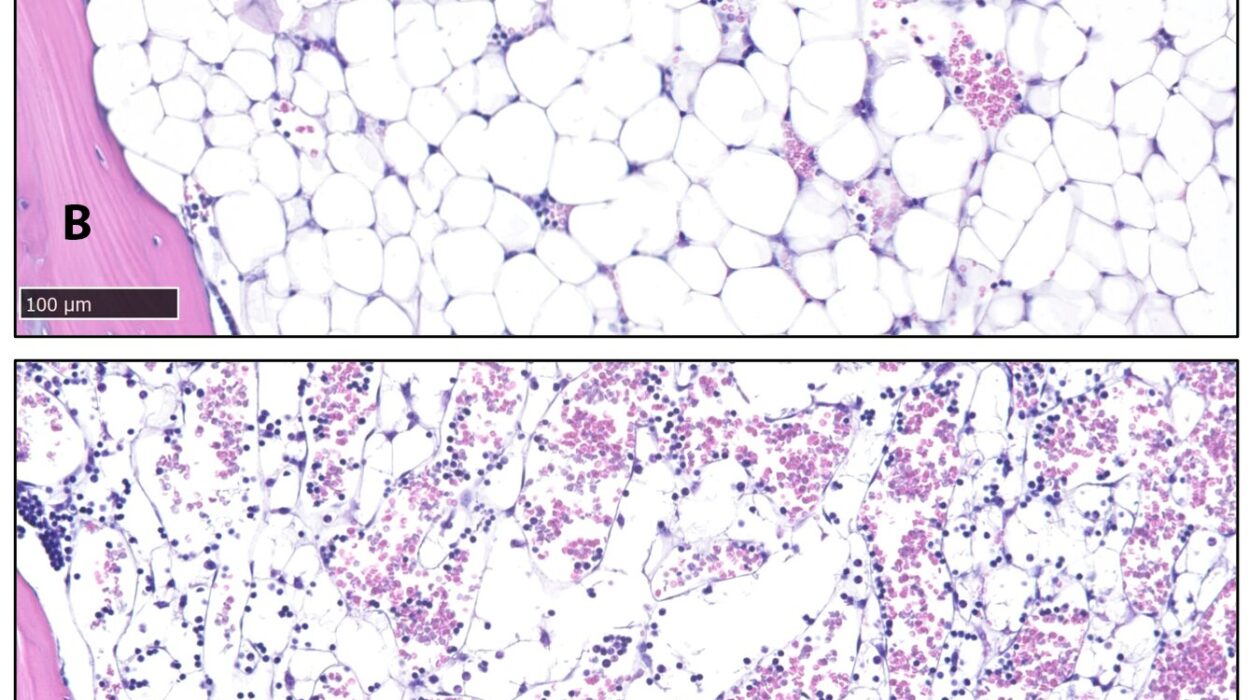
To study the effects of salt on the body, researchers turned to lab rats—animals that, unlike mice, regulate salt and water in a way that closely resembles humans. The rats were given water with 2% salt, a level comparable to what a person might consume from a diet heavy in fast food, instant noodles, processed meats, or cheese.
What the scientists discovered was striking. The salty diet triggered immune cells in a small but crucial region of the brain. These activated cells caused inflammation, which set off a surge of vasopressin—a hormone that signals the body to hold onto water and constrict blood vessels. The end result: a sharp rise in blood pressure.
This chain reaction shows that the brain is not just passively responding to changes in blood pressure—it can actively drive the process, especially when challenged by excess salt.
New Tools to See the Invisible
One reason this brain connection has been overlooked for so long is that the brain is notoriously difficult to study. Unlike blood pressure in the arm or kidney function in a lab test, inflammation inside tiny brain circuits is invisible without advanced tools.
But thanks to new imaging technologies and molecular techniques, scientists can now track these changes in real time. “With new techniques, we’re able to see these changes in action,” says Prager-Khoutorsky. This shift is giving researchers unprecedented access to the hidden processes that shape blood pressure from inside the brain.
Why This Matters for Patients
The discovery has enormous implications. If the brain plays a central role in hypertension, particularly in treatment-resistant cases, then future therapies may target brain pathways rather than just focusing on the kidneys and blood vessels. This could provide hope for millions of patients who currently struggle to keep their blood pressure under control.
It also reinforces public health warnings about high-salt diets. While many people think of salt only in terms of bloating or thirst, this research reveals deeper consequences: salty meals may be quietly fueling inflammation in the brain, nudging blood pressure upward in ways we never imagined before.
What Comes Next
The McGill team is now investigating whether similar brain-driven processes occur in other forms of hypertension, including those not directly linked to salt. If they do, it could mark a turning point in how we understand and treat this condition.
For now, the takeaway is both sobering and empowering. Hypertension is not just a matter of blood vessels tightening or kidneys retaining fluid. It is also a story written inside the brain. And that means what we choose to eat—especially when it comes to salty foods—may shape not just our waistlines but also our brain’s control over one of the most vital measures of health: blood pressure.
More information: Ning Gu et al, Microglia regulate neuronal activity via structural remodeling of astrocytes, Neuron (2025). DOI: 10.1016/j.neuron.2025.07.024