Mental health disorders have always carried an air of mystery. Conditions like depression, schizophrenia, and bipolar disorder can reshape lives in profound ways, yet their origins often remain elusive. While environment and life experiences undeniably play a role, scientists have long known that genetics exerts a powerful influence on who develops these disorders and how they manifest. The question has always been: how do our genes translate into changes in the brain that shape vulnerability to psychiatric conditions?
A new study, led by researchers at the University of Pennsylvania, the Children’s Hospital of Philadelphia, and several partner institutions, takes a bold step toward answering this question. Published in Nature Mental Health, the work reveals specific genetic footprints that simultaneously shape the structure of the brain’s cortex and increase the risk of psychiatric disorders. By tracing these connections, the study illuminates the hidden biological pathways that may underlie some of the most challenging mental health conditions of our time.
The Brain’s Blueprint in Our DNA
The human cortex—the outer layer of the brain responsible for higher-order functions like reasoning, memory, and emotion—is not uniform. Its shape, thickness, and surface area vary subtly from person to person. Some of these differences are harmless quirks of individuality, but others may mark a higher likelihood of developing mental health challenges.
What makes this new research so groundbreaking is that it links these structural brain differences back to precise locations in human DNA. The researchers examined vast genetic datasets from major projects such as the European Genomics Consortium, the UK Biobank, and the Adolescent Brain Cognitive Development (ABCD) study. These datasets contained not just DNA samples but also brain imaging data, allowing scientists to look for overlapping patterns.
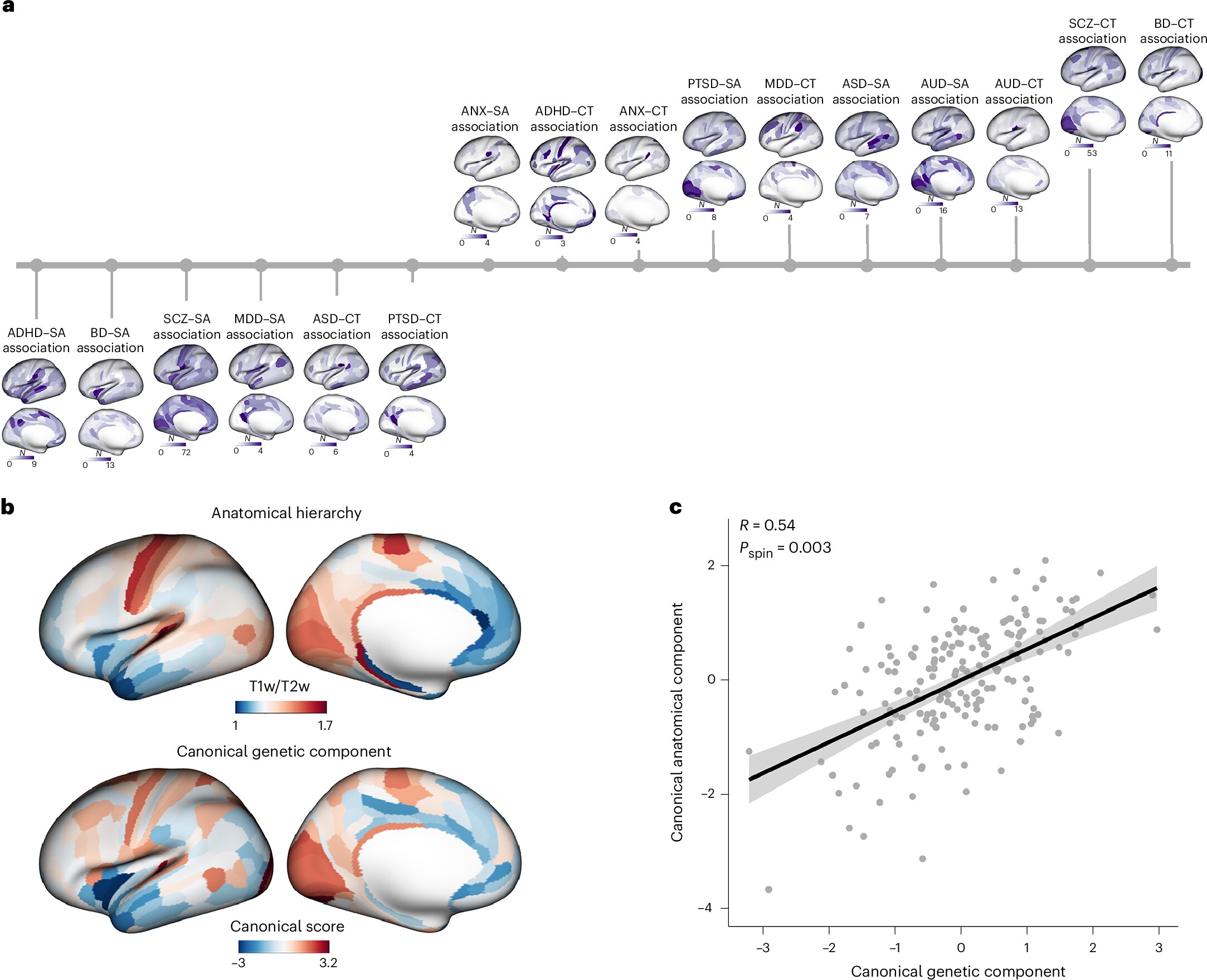
Using advanced statistical tools, the team identified dozens of genetic loci—specific positions on chromosomes—that influence both brain structure and psychiatric risk. In other words, the same genetic variants that increase the likelihood of a psychiatric disorder can also leave measurable imprints on the shape and architecture of the cortex.
A Complex and Surprising Genetic Map
The study uncovered 55 genetic regions that affect the brain’s surface area and 29 that influence cortical thickness. These numbers are more than statistics—they represent hidden levers within the genome that tug on the brain in different ways.
What surprised the researchers most was the direction of these genetic effects. In some cases, a variant might enlarge one region of the cortex while simultaneously shrinking another. This suggests that psychiatric vulnerability is not the result of simple, uniform changes but of a delicate, sometimes contradictory balance in brain development.
As Zhiqiang Sha, the study’s first author, explained: “Remarkably, these genetic variants can drive brain regions to grow larger or smaller in opposite directions, highlighting complex, not always intuitive, genetic effects.”
This complexity also reveals why traditional genetic studies sometimes miss key connections. Looking at the brain as a whole may smooth over these regional variations, but by zooming in with unprecedented precision, Sha and his colleagues could map out the subtle ways in which DNA sculpts the cortex and shapes mental health.
From Discovery to Prevention and Treatment
The implications of these findings are profound. By understanding the genetic and structural underpinnings of psychiatric disorders, scientists move closer to predicting risk earlier in life—possibly even before symptoms appear. For example, if a young person carries genetic variants known to alter the structure of certain brain regions, clinicians might one day monitor their development more closely, offering preventive interventions or early support.
This approach could transform mental health care. Instead of waiting for illness to fully manifest, doctors could anticipate vulnerability and act preemptively, much like we monitor cholesterol levels to prevent heart disease.
Moreover, the genetic loci identified in this study may point toward biological pathways that could be targeted by new therapies. If certain genes influence both cortical structure and psychiatric risk, then drugs or interventions that modulate these pathways might alleviate symptoms or slow the progression of disorders.
Building a Bigger Picture of the Brain
The researchers are not stopping here. Future work will focus on how these genetic effects unfold across development—from childhood through adulthood—and how they interact with other layers of biology. Gene expression patterns, brain connectivity, and environmental factors like stress and trauma will all need to be integrated into a larger framework.
“We are also interested in testing whether these genetic effects can help predict early vulnerability to psychiatric disorders before clinical symptoms appear,” Sha noted. This is a crucial step, as psychiatric conditions often emerge during adolescence or early adulthood, years after the genetic and structural groundwork may have been laid.
By building this layered, multidimensional picture, scientists hope to move from broad associations to actionable insights—insights that could guide more precise, individualized treatment strategies.
The Human Story Behind the Science
Beyond the data and statistical models, this research carries a deeply human dimension. Every genetic variant identified is a clue that may help ease the suffering of millions of people worldwide living with psychiatric disorders. For patients and families, the hope is not simply for explanation but for tangible improvements in care.
The study reminds us that psychiatric disorders are not signs of weakness or moral failing—they are conditions rooted in biology, shaped by invisible forces written into our DNA and expressed in the structure of our brains. By uncovering these hidden patterns, science takes one more step toward compassion, understanding, and healing.
Conclusion: A New Era in Mental Health Research
The study from the University of Pennsylvania and its collaborators represents more than a technical achievement—it marks a new era in the study of mental health. By connecting the dots between genetics, brain structure, and psychiatric disorders, researchers are beginning to decipher the complex code that links our DNA to our mental well-being.
Though many mysteries remain, the path forward is clearer than ever. Genetics will not determine destiny, but it will provide a map—a guide to understanding risk, protecting health, and tailoring treatment. As this map becomes more detailed, the hope is that society will move toward a future where psychiatric disorders are not only better understood but also more effectively prevented and treated.
In this sense, the brain’s hidden genetic blueprint is not just a story of science but of possibility—a reminder that even in the most complex corners of the mind, discovery holds the power to change lives.
More information: Zhiqiang Sha et al, The overlapping genetic architecture of psychiatric disorders and cortical brain structure, Nature Mental Health (2025). DOI: 10.1038/s44220-025-00475-7.