It usually begins quietly. Maybe you’re sitting on the couch after the kids are in bed, or maybe it’s over coffee on a Saturday morning. The subject drifts—half casually, half seriously—to the idea of being done with having children. Your partner might say, “We’ve built our family. Maybe it’s time to think about something permanent.”
In that moment, the concept of a vasectomy enters the room. For many men, it’s a strange mixture of relief, fear, and curiosity. Relief at the idea of freedom from unplanned pregnancies. Fear at the idea of anything surgical involving that part of the body. And curiosity about what it would actually mean for life, intimacy, and identity.
This is a conversation worth having in depth, because vasectomy is more than a quick medical procedure. It’s a personal decision that sits at the crossroads of health, relationships, and future plans. To understand it fully, we need to explore not just the medical facts, but the emotional landscape that surrounds it.
What Vasectomy Really Is
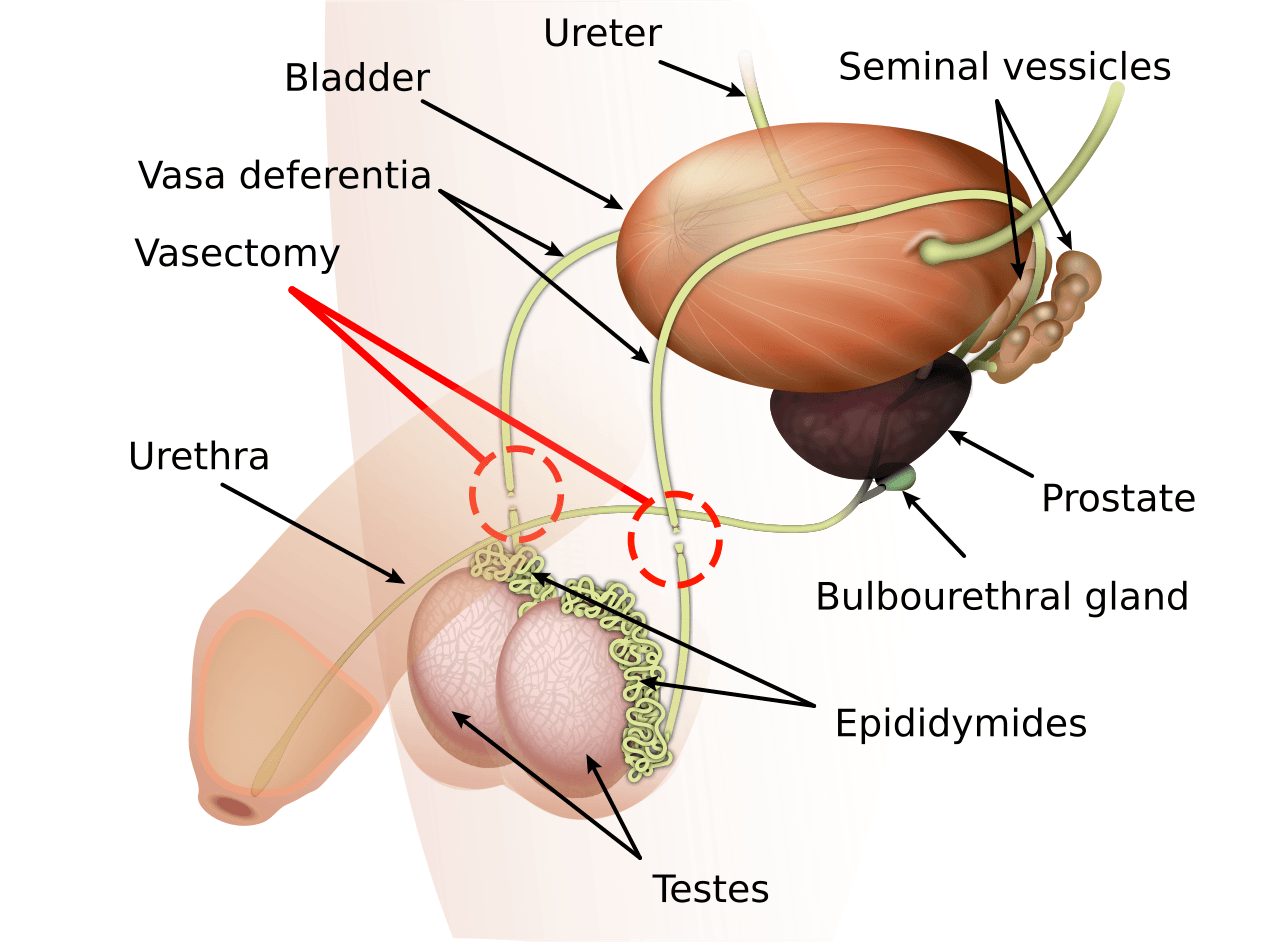
At its simplest, a vasectomy is a minor surgical procedure designed to permanently prevent sperm from reaching semen during ejaculation. The sperm are still produced in the testes, but after the procedure, they no longer travel through the vas deferens—the tubes that normally carry them to be mixed with seminal fluid.
Without sperm in the semen, fertilization cannot occur. The body naturally reabsorbs the unused sperm. Importantly, the production of testosterone—the hormone responsible for libido, muscle mass, and secondary male characteristics—continues as normal. Sexual function, erections, and orgasm are unaffected. In fact, most men find that the only difference in their sex life is a greatly reduced level of worry about pregnancy.
From a medical standpoint, it is one of the most effective methods of birth control available, with a success rate of more than 99%. But its power comes from the fact that it is meant to be permanent. While reversal is technically possible, it’s not guaranteed, and it can be costly and invasive. That permanence is both its strength and the reason it requires careful consideration.
The Decision Beyond the Clinic
Choosing a vasectomy isn’t just about personal anatomy—it’s about personal readiness. It demands a certain clarity about the future. Are you certain you don’t want more biological children? Have you and your partner talked through the possibility of future changes—divorce, new relationships, unexpected life events—that could alter how you feel about that choice?
These are not easy questions. A man in his late thirties, married with two children, might feel confident that his family is complete. But a man in his twenties, uncertain about his long-term relationship or future life path, may find the permanence more daunting. Doctors often encourage men to think long-term, because while vasectomy reversal exists, it’s never wise to count on it as a backup plan.
Emotionally, men can approach the decision from different angles. Some see it as a proactive and loving step—taking responsibility for contraception so their partner doesn’t have to bear the hormonal or surgical burdens. Others wrestle with a quiet fear: will this make me less of a man? (The answer, unequivocally, is no.) Myths about masculinity and virility often swirl around the procedure, but they dissolve quickly in the light of medical fact and lived experience.
Myths and Truths
Few medical topics are surrounded by as many persistent myths as vasectomy. One of the most common is the belief that it will affect sexual performance or pleasure. In reality, neither erections nor orgasms are altered; if anything, couples often report improved intimacy due to reduced anxiety about pregnancy. Another myth suggests it leads to a decline in testosterone levels, but hormone production remains entirely unchanged.
There is also the misconception that vasectomy is instantly effective. In truth, it can take several weeks and dozens of ejaculations before remaining sperm are fully cleared from the system. Men must use alternative contraception until follow-up semen analysis confirms a zero sperm count. This step, while simple, is essential for ensuring the procedure’s success.
Finally, some fear the surgery itself will be deeply painful. Modern vasectomy techniques—particularly the no-scalpel method—are quick, involve minimal discomfort, and often require only local anesthesia. Most men resume light activities within a couple of days and full activity within a week.
The Procedure in the Real World
The no-scalpel vasectomy, now widely practiced, is the most common approach. Instead of making incisions, the doctor uses a special instrument to puncture the skin of the scrotum, spread the tissue, and reach the vas deferens. Each vas deferens is then cut, sealed, or tied to prevent sperm from passing through. The small puncture heals without stitches, and scarring is minimal.
The procedure usually takes about 15–30 minutes. Many men are surprised at how straightforward and unthreatening it feels compared to their fears going in. Some even describe chatting casually with the doctor about sports or weekend plans while it’s happening.
Afterward, the typical advice is rest for a day or two, ice packs for swelling, and avoiding strenuous activity for about a week. Mild soreness is common, but severe complications are rare. Most men return to work quickly—unless their job involves heavy physical labor, in which case a longer recovery is advised.
Emotional Aftermath and Adjustment
For many men, the days and weeks after a vasectomy bring a sense of freedom. The constant background hum of pregnancy risk is gone. For couples, intimacy can become more spontaneous, unshackled from the need for condoms or the side effects of hormonal birth control.
But it’s also normal for men to feel a period of emotional adjustment. Some may experience a fleeting sense of loss, even if they are certain about their decision. It’s not the loss of physical capability—sexual function is intact—but the quiet acknowledgment of closing a chapter in life. This emotional processing is not a sign of regret; rather, it reflects the weight of making a permanent choice about fertility.
Communication with a partner during this time is vital. Open discussion about feelings—both relief and any moments of doubt—can help couples navigate this transition with understanding.
A Broader View: Responsibility and Equality
One of the most important aspects of vasectomy is its role in balancing reproductive responsibility between partners. Historically, women have shouldered the majority of contraception—physically, hormonally, and emotionally. Methods such as the pill, IUDs, injections, and tubal ligation often come with more risks, side effects, or invasive procedures than a vasectomy.
By choosing vasectomy, a man can take on that responsibility in a way that is safe, effective, and final. This act can carry a sense of partnership and fairness in relationships. It says, in effect, “I’m willing to carry my share of the reproductive load.”
Considering Life Scenarios
It’s impossible to predict every twist of life, but part of the vasectomy decision is thinking about “what if” scenarios. What if a tragedy occurred and you later wanted another child? What if you remarried someone who had no children and wanted them? While adoption and assisted reproductive technologies can be options, they are not the same as natural conception.
Doctors sometimes encourage men to wait until they are truly certain about these scenarios—or to consider sperm banking beforehand. Freezing sperm prior to the procedure is an option that provides a kind of insurance, though it comes with its own costs and limitations.
The Global Perspective
Around the world, vasectomy adoption rates vary widely. In countries like Canada, New Zealand, and the UK, vasectomy is a common form of birth control among couples who have completed their families. In contrast, rates are lower in many parts of Asia, Africa, and Latin America, often due to cultural norms, lack of access, or lingering myths about the procedure.
In the United States, vasectomy is chosen by roughly half a million men each year. The conversations surrounding it are becoming more open, aided by public health campaigns and honest stories from men who have undergone the procedure. These narratives help break down stigma and encourage informed decision-making.
The Personal Story Behind the Decision
Numbers and medical facts tell part of the story, but every vasectomy decision is personal. For some men, it comes after years of using other contraceptives and feeling ready to set that responsibility aside. For others, it follows a difficult pregnancy for a partner, or a health condition that makes further pregnancies risky.
There are men who walk into the clinic certain and confident, and others who make the decision only after months of reflection. What unites these experiences is the understanding that this is a choice about the future, love, and responsibility—one that touches both partners deeply.
Life After Vasectomy
In the long term, most men report high satisfaction with their decision. The absence of pregnancy worries can allow couples to focus more on their relationship and less on family planning logistics. Studies show that sexual satisfaction often improves, likely due to the combination of confidence, reduced stress, and maintained physical function.
The body continues to function much as it did before: sperm are still produced, hormones remain stable, and semen volume is nearly identical (since sperm make up only a small fraction of semen). The change is invisible to the naked eye—and often, after the initial healing period, invisible to the man himself in terms of sensation and capability.
Closing Thoughts
A vasectomy is a medical procedure, but it’s also a life decision. It is as much about values, relationships, and self-knowledge as it is about anatomy. The best decisions come from combining clear medical understanding with honest personal reflection.
For the man who knows his family is complete, or who is certain he does not want children, vasectomy offers a safe, effective, and lasting solution. It is an act of trust in oneself and in one’s partner—a quiet but powerful way to take control of the future.
In the end, the conversation about vasectomy is not really about losing something—it’s about gaining peace of mind, shared responsibility, and freedom from the constant calculation of reproductive risk. And that, for many men, is a conversation worth having sooner rather than later.