You’ve had a great week—slept well, exercised, ate clean, and still, out of nowhere, anxiety floods in. Or perhaps you’ve felt like crying for no clear reason, even as everything in life seems to be going right. These experiences can be confusing and unsettling, especially when we can’t tie our feelings to something tangible. But often, what we chalk up to “just being emotional” has more to do with what’s going on inside us than around us. Specifically, it has everything to do with hormones.
Hormones are chemical messengers that regulate virtually every process in our body—from hunger to sleep, reproduction to metabolism, and yes, even our emotions and mental well-being. The brain and body are in constant communication through a symphony of hormones, and when that delicate balance is thrown off, the results can be mood swings, anxiety, depression, irritability, or even a complete emotional shutdown.
Understanding how hormones affect our mental health is essential—not just for women navigating monthly cycles or menopause, but for everyone who wants to better understand the often invisible factors that shape our mood, memory, and motivation.
Hormones: The Mind’s Quiet Architects
To understand the connection between hormones and mental health, we first need to appreciate what hormones actually are. Produced by glands throughout the endocrine system—such as the pituitary, adrenal, thyroid, ovaries, and testes—hormones act like chemical postmen, delivering messages between cells and systems. These messages affect your heart rate, digestion, immune function, sleep patterns, sexual desire, and how you respond to stress.
In the brain, hormones work closely with neurotransmitters like serotonin, dopamine, and GABA to regulate emotional states. But unlike neurotransmitters, which act within the nervous system, hormones travel through the bloodstream and take longer to kick in, often creating longer-term effects on mood and cognition. That’s why hormonal fluctuations—whether gradual or sudden—can lead to noticeable emotional and psychological changes that feel disproportionate to your external circumstances.
In essence, hormones are not just part of your body—they are part of your mind. And when they whisper (or scream), your brain listens.
Estrogen’s Influence on Mood and Cognition
Among the most powerful hormones affecting mental health is estrogen, often referred to as the “female hormone,” although it plays important roles in all genders. Estrogen doesn’t just regulate the menstrual cycle or fertility—it also acts in the brain, particularly in areas associated with mood regulation, such as the hippocampus and prefrontal cortex.
Estrogen increases the availability of serotonin, the “feel-good” neurotransmitter, while also enhancing the effects of endorphins and influencing dopamine pathways. This is why estrogen is often linked to feelings of well-being, calm, and resilience. When estrogen levels are high, many women report better mood, clearer thinking, and more stable emotions. But when estrogen drops—such as during PMS, after childbirth, or in perimenopause—the changes can be profound.
Low estrogen can lead to irritability, anxiety, fatigue, memory lapses, and a vulnerability to depression. These aren’t just emotional reactions—they are neurochemical shifts that change how the brain processes information and regulates feelings.
It’s no coincidence that mood disorders in women often correlate with periods of hormonal upheaval. From puberty to menopause, estrogen plays an ongoing role in shaping mental health. And when that balance is disrupted, even temporarily, it can feel like losing your emotional compass.
Progesterone: The Soothing—or Sedating—Counterpart
While estrogen gets much of the spotlight, progesterone is equally important in the hormonal landscape, especially when it comes to mental well-being. Often described as having a calming or even sedative effect, progesterone promotes sleep, reduces anxiety, and balances the excitatory effects of estrogen.
One of the ways it does this is through its interaction with GABA, the brain’s primary inhibitory neurotransmitter. GABA helps to quiet the nervous system, making us feel more relaxed and less reactive. Progesterone enhances GABA’s activity, which is why women often feel more emotionally stable during the mid-luteal phase of their cycle when progesterone peaks.
But when progesterone levels fall—as they do before menstruation or during the transition to menopause—this calming effect disappears. The result can be insomnia, mood swings, and heightened emotional sensitivity. Some women even describe this phase as “living in a different brain,” where the world feels more chaotic, louder, and harder to handle.
For those with a history of anxiety or depression, these hormonal drops can trigger full-blown episodes. Recognizing progesterone’s role in mental health gives us a clearer picture of why mood changes can be so closely tied to the menstrual cycle and reproductive milestones.
Testosterone and Emotional Resilience
Although testosterone is primarily associated with men, it plays a critical role in the mental health of all genders. In men, low testosterone has been linked to irritability, fatigue, depression, and difficulty concentrating—a constellation of symptoms sometimes referred to as “andropause.”
Testosterone affects the brain’s reward system and helps maintain motivation, confidence, and a sense of drive. It also influences serotonin and dopamine levels, helping to regulate mood and protect against feelings of helplessness or low energy.
In women, too much testosterone (as seen in conditions like polycystic ovary syndrome, or PCOS) can contribute to mood disturbances, irritability, and even symptoms of aggression. On the flip side, too little testosterone can lead to fatigue, brain fog, and a lack of sexual desire.
Balanced testosterone supports emotional strength, resilience, and mental clarity. Disruption of this balance—whether due to aging, illness, or other factors—can quietly erode emotional well-being.
Cortisol: The Stress Hormone That Won’t Let You Rest
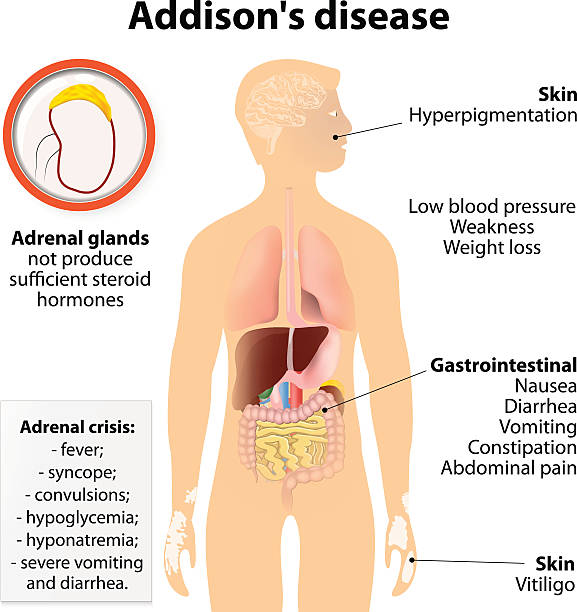
When we talk about hormones and mental health, it’s impossible to ignore cortisol, the body’s primary stress hormone. Produced by the adrenal glands, cortisol helps us respond to danger by increasing blood sugar, sharpening focus, and preparing the body for “fight or flight.” This was helpful when humans were fleeing predators. But in modern life, where the stressors are constant and cortisol remains elevated, the effects can be damaging.
Chronically high cortisol levels are linked to anxiety, depression, memory loss, and sleep disturbances. It shrinks the hippocampus, the brain’s center for learning and memory, and weakens the immune system. It also disrupts other hormones—like estrogen, progesterone, and thyroid hormone—creating a cascade of imbalances that further impact mood and cognition.
What makes cortisol especially tricky is that it can be both a cause and consequence of mental health issues. Stress raises cortisol, which increases vulnerability to anxiety and depression, which in turn heightens stress—a vicious cycle that can be hard to escape.
On the other hand, abnormally low cortisol levels—as seen in adrenal fatigue or Addison’s disease—can also result in depression, apathy, and physical exhaustion. Whether it’s too much or too little, cortisol imbalance creates a mental and physical state that feels unsustainable.
Thyroid Hormones and the Brain’s Metabolic Engine
The thyroid gland, though small and butterfly-shaped, has a sweeping influence on mental health. Thyroid hormones regulate metabolism, energy production, and brain activity. When thyroid levels are off, the effects are often first felt in the brain.
Hypothyroidism, or low thyroid function, is strongly associated with depression, brain fog, low motivation, and fatigue. People with underactive thyroids may feel slowed down, emotionally flat, or disconnected from life. In some cases, they are misdiagnosed with clinical depression when the root cause is hormonal.
Conversely, hyperthyroidism, or an overactive thyroid, can create a sense of racing thoughts, nervousness, irritability, and sleep problems—symptoms that mimic anxiety or panic disorder.
Thyroid imbalances are more common than many people realize, especially in women, and often go undiagnosed. Blood tests can help identify abnormalities, but understanding the connection between thyroid function and mental health is key to getting the right support.
Puberty, Pregnancy, Menopause: Hormonal Storms of Transformation
Certain life stages are known for their emotional upheaval—and not without reason. These are periods of intense hormonal change, where the endocrine system is reshaping the brain’s wiring in profound ways.
Puberty is the first major hormonal earthquake, where a surge of sex hormones rewires the adolescent brain. The emotional volatility, mood swings, and risk-taking behaviors typical of adolescence are largely driven by these changes.
Pregnancy brings another hormonal tidal wave. Estrogen and progesterone levels skyrocket—up to 50 times higher than normal—and create a heightened emotional sensitivity. Some women feel euphoric; others experience depression or anxiety, particularly if they have a history of mood disorders. The sudden drop in hormones after childbirth can trigger postpartum depression, a serious condition affecting one in seven women.
Menopause marks the final major shift, as estrogen and progesterone levels decline and eventually flatline. Many women report increased anxiety, irritability, or depression during this time—not because of psychological issues, but because their neurochemical environment has changed drastically.
These transitions are not flaws in the system; they are biologically natural. But without support and understanding, they can become periods of mental distress. Recognizing the hormonal root of these feelings allows for compassion and more effective treatment.
The Gut-Brain-Hormone Connection
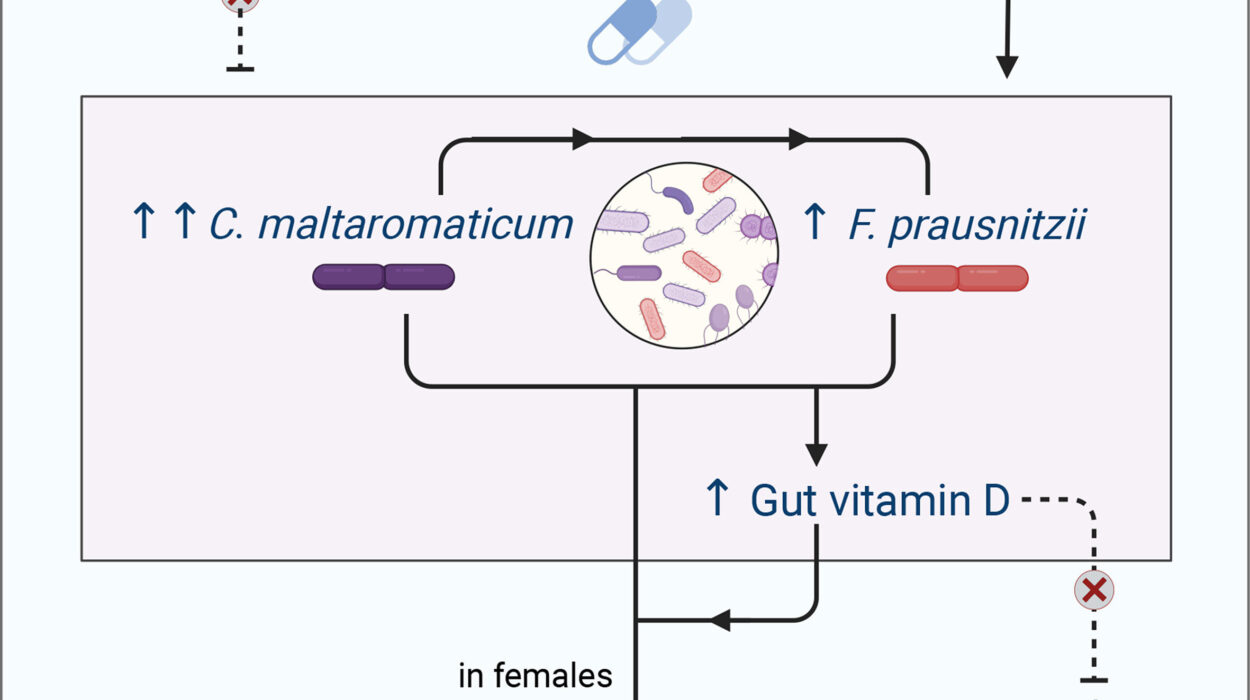
Emerging research is revealing a fascinating link between gut health, hormones, and mental well-being. The gut microbiome—the trillions of bacteria living in our intestines—plays a key role in hormone regulation and neurotransmitter production.
Gut bacteria influence the breakdown of estrogen, the balance of cortisol, and the production of serotonin (up to 90% of which is made in the gut). Dysbiosis, or imbalance in the gut flora, can lead to inflammation, hormonal disruption, and mood disorders.
What you eat, how you digest food, and the health of your gut lining all feed into this hormonal network. Supporting gut health through nutrition, probiotics, and stress reduction can have profound effects on both hormone balance and emotional health.
Psychological Disorders and Hormonal Links
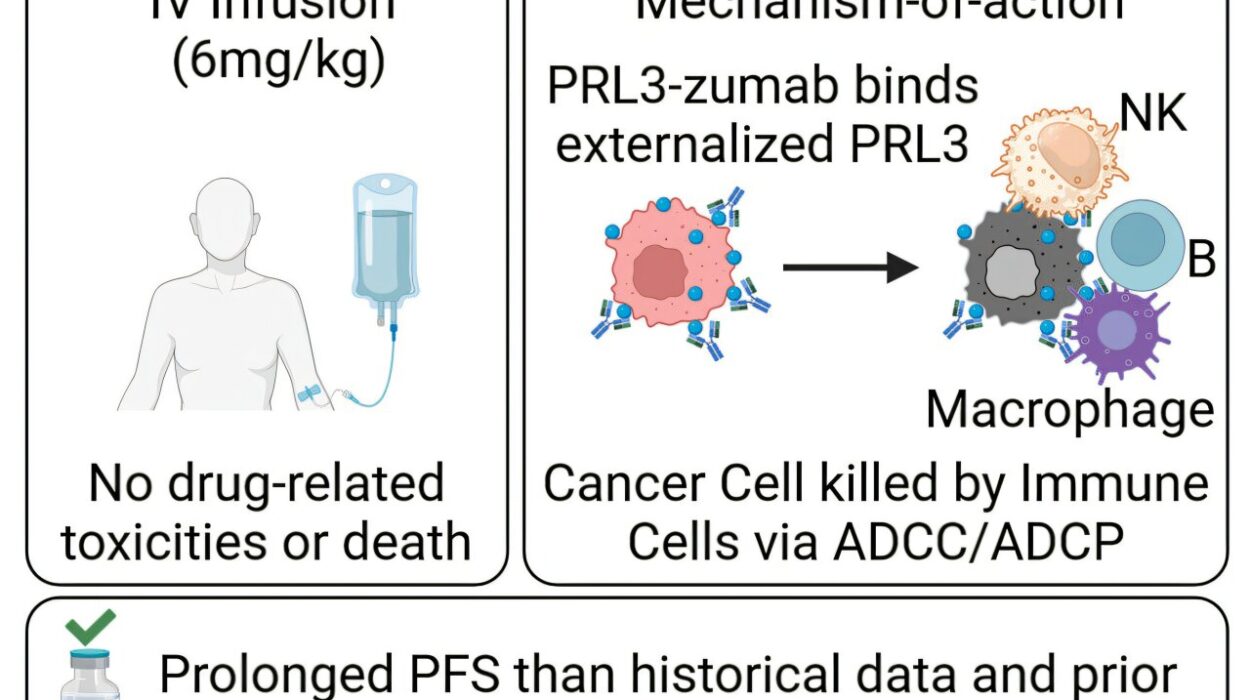
Many mental health disorders have a hormonal component, even when it’s not immediately obvious. Premenstrual Dysphoric Disorder (PMDD), for example, is a severe form of PMS driven by abnormal sensitivity to hormonal fluctuations. Women with PMDD experience debilitating mood swings, depression, and anxiety during the luteal phase of their cycle.
Polycystic Ovary Syndrome (PCOS) is another example. This endocrine disorder is characterized by excess androgens and insulin resistance, and it often comes with mood issues, including increased rates of anxiety and depression.
Even major depressive disorder, bipolar disorder, and schizophrenia have been linked to hormonal disruptions, especially those involving cortisol, thyroid hormones, and sex hormones. These conditions are not “just in your head”—they may be rooted, at least in part, in the body’s chemistry.
Balancing Hormones for Better Mental Health
The good news is that hormonal imbalances can be treated—and when they are, mental health often improves. This doesn’t mean every emotional fluctuation requires hormone therapy, but it does suggest that comprehensive care should include a look at hormonal health.
For some, this might mean thyroid medication or bioidentical hormone replacement therapy. For others, it could involve lifestyle changes that support the endocrine system: reducing sugar, improving sleep, managing stress, and eating a hormone-friendly diet.
Therapists, psychiatrists, and endocrinologists must increasingly work together to address the whole person—not just the mind or the body in isolation. When mental health treatment includes hormonal evaluation, people get better, faster, and in a more sustainable way.
Conclusion: The Chemistry of Being Human
Our moods, thoughts, and feelings are not floating in a vacuum. They are built from the complex interplay of molecules, many of which are shaped by our hormones. To understand mental health fully, we must understand this invisible architecture.
Hormones don’t just regulate our physical bodies—they shape our emotional lives. They influence how we respond to stress, how we feel love and loss, how we connect to others, and how we see ourselves.
Recognizing the link between hormones and mental health isn’t about excusing emotional experiences—it’s about validating them. It’s about creating a language for the times when you feel “off” and don’t know why. And most importantly, it’s about knowing that these feelings are real, rooted, and treatable.
When we align mental health care with hormonal wisdom, we don’t just chase symptoms—we heal at the source.