In the vast symphony of life, our bodies function with breathtaking precision. Every second, trillions of cells work in concert—dividing, communicating, dying, and renewing. This elaborate cellular choreography is what keeps us alive, healing, growing, and thriving. But sometimes, within this orderly system, a single cell makes a subtle mistake. And if that mistake is left unchecked, it may multiply into a force of astonishing destructiveness.
Cancer does not begin as a monster. It begins as a small rebellion—a single cell stepping out of line. At first, it might just divide when it shouldn’t or ignore a signal to rest. But gradually, it forgets its place in the body. It stops cooperating. It cheats, it lies, and eventually, it starts to grow with abandon, like a weed breaking through the cracks of a meticulously laid garden path.
Cancer is not a foreign invader. It is a distorted reflection of our own biology. That is what makes it both fascinating and terrifying. Understanding cancer means understanding how ordinary cells, governed by natural laws and built-in safeguards, can slowly transform into rogue agents. These cells evolve inside us, adapt to the body’s defenses, and sometimes—if unchecked—reshape the architecture of life itself.
Cellular Cooperation and the Laws of the Body
To understand how cancer begins, we must first understand how healthy cells behave. The human body is made of more than 30 trillion cells, and each one must obey a strict set of rules. These rules are enforced through molecular signaling pathways and genetic blueprints encoded in DNA.
Every cell in the body carries the same genetic code, but not every gene is active in every cell. Skin cells behave differently from liver cells or neurons because different genes are switched on or off depending on their function. This specialization is called differentiation. And it’s this specialization that allows your brain to think, your heart to pump, your skin to protect, and your bones to support.
To maintain this order, cells have a system of checks and balances. They can divide, but only when prompted. They can grow, but only within the space allowed. When damaged, they repair themselves—or if the damage is too great, they undergo programmed death, known as apoptosis. It is a beautifully evolved system where individual cells prioritize the greater good of the organism.
But when this system breaks down, the consequences can be catastrophic.
Mutations and the First Steps Toward Chaos
The transformation from a normal cell into a cancer cell begins with mutations—changes in the DNA. These changes can be caused by a variety of factors: ultraviolet radiation from sunlight, chemicals in tobacco smoke, errors during DNA replication, or inherited genetic defects.
But not all mutations are created equal. Cells accumulate mutations throughout life, and most are harmless. Some even go unnoticed. For a mutation to lead to cancer, it usually has to occur in specific types of genes that control how a cell grows and divides. These include oncogenes, which can push cells to divide, and tumor suppressor genes, which act like brakes to stop uncontrolled growth.
If an oncogene becomes overactive or a tumor suppressor gene is silenced, the cell can begin to act abnormally. It may divide too quickly or refuse to die when damaged. The result is a small cluster of misbehaving cells, quietly building a foothold in the tissue.
But cancer is rarely the result of a single mutation. It usually takes several hits to key regulatory systems for a cell to go fully rogue. This is one reason why cancer risk increases with age—the longer we live, the more opportunities for these mutations to accumulate.
The Hallmarks of a Cellular Revolution
As scientists have studied cancer over the decades, they’ve come to recognize certain defining traits that most cancer cells acquire over time. These are sometimes called the hallmarks of cancer, and they help describe how cells break free from the normal rules of biology.
One hallmark is sustained proliferative signaling—cancer cells can send their own signals to grow, even in the absence of external stimuli. Another is evading growth suppressors—ignoring commands that would normally shut down unnecessary division.
Cancer cells also develop resistance to cell death. When most healthy cells experience severe stress or DNA damage, they initiate apoptosis. Cancer cells, however, learn how to disable this self-destruct mechanism.
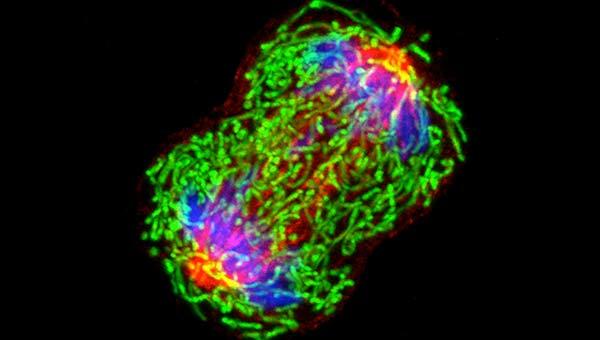
Another key feature is replicative immortality. Normal cells can only divide a limited number of times before their telomeres—protective caps on the ends of chromosomes—become too short, triggering senescence. Cancer cells often activate enzymes like telomerase to keep their telomeres intact, allowing them to divide endlessly.
Eventually, as tumors grow, they begin to demand more resources. They hijack the body’s blood supply by promoting the growth of new blood vessels—a process known as angiogenesis. This ensures a steady flow of nutrients and oxygen to feed their expansion.
Perhaps most dangerously, cancer cells can acquire the ability to invade nearby tissues and spread to distant parts of the body. This is metastasis—the step that transforms a localized problem into a systemic, life-threatening disease.
Immune Evasion and the Disguise of Cancer
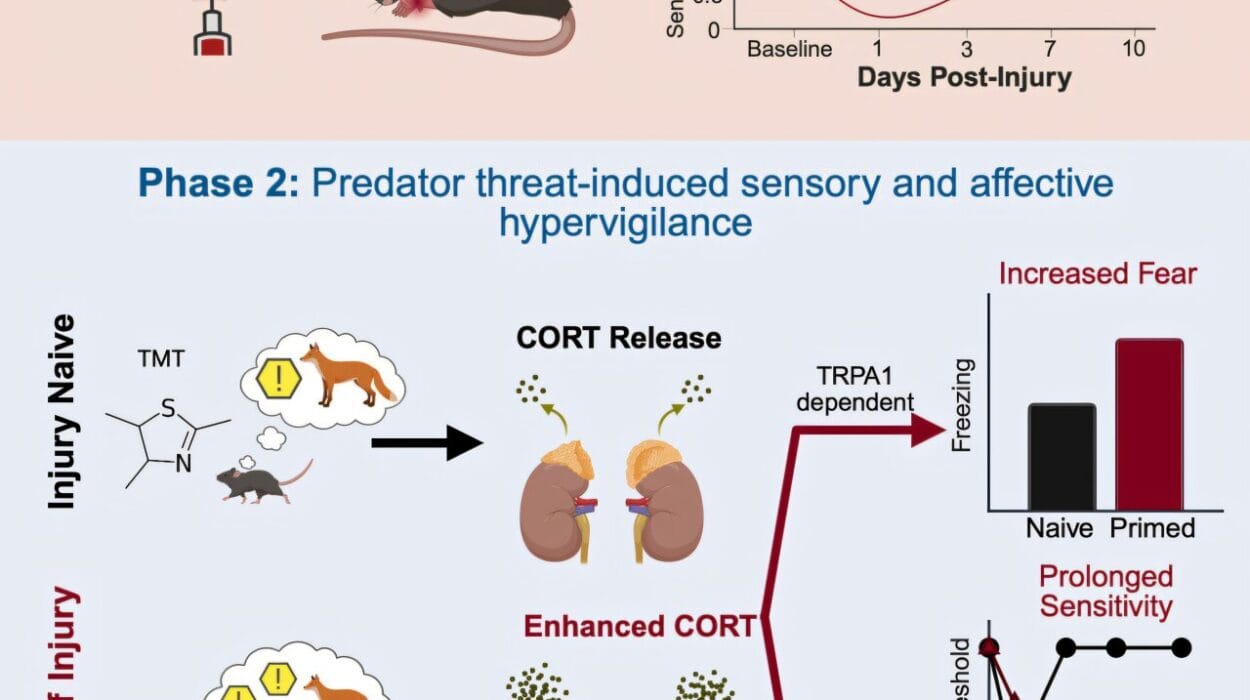
One might assume that the immune system, our body’s powerful defense force, would swiftly detect and destroy rogue cancer cells. And often, it does. Every day, the immune system patrols for abnormal cells and eliminates many before they can gain a foothold. But cancer cells are cunning. They evolve methods to hide from the immune system or even suppress its responses.
Some cancer cells stop displaying the molecular flags that typically alert immune cells to their presence. Others secrete substances that create a microenvironment hostile to immune activity. Certain tumors attract immune cells only to reprogram them into allies, promoting inflammation that actually helps the tumor grow.
This ability to evade immune destruction has become a major focus of cancer research in recent years. Scientists have developed drugs known as immune checkpoint inhibitors that essentially remove the “brakes” from immune cells, allowing them to attack cancer more effectively. This field, known as immunotherapy, has revolutionized treatment for certain types of cancer like melanoma and lung cancer.
Still, the battle between cancer and the immune system is an evolutionary arms race—one that unfolds inside the body in real time, with every patient’s disease taking a unique path.
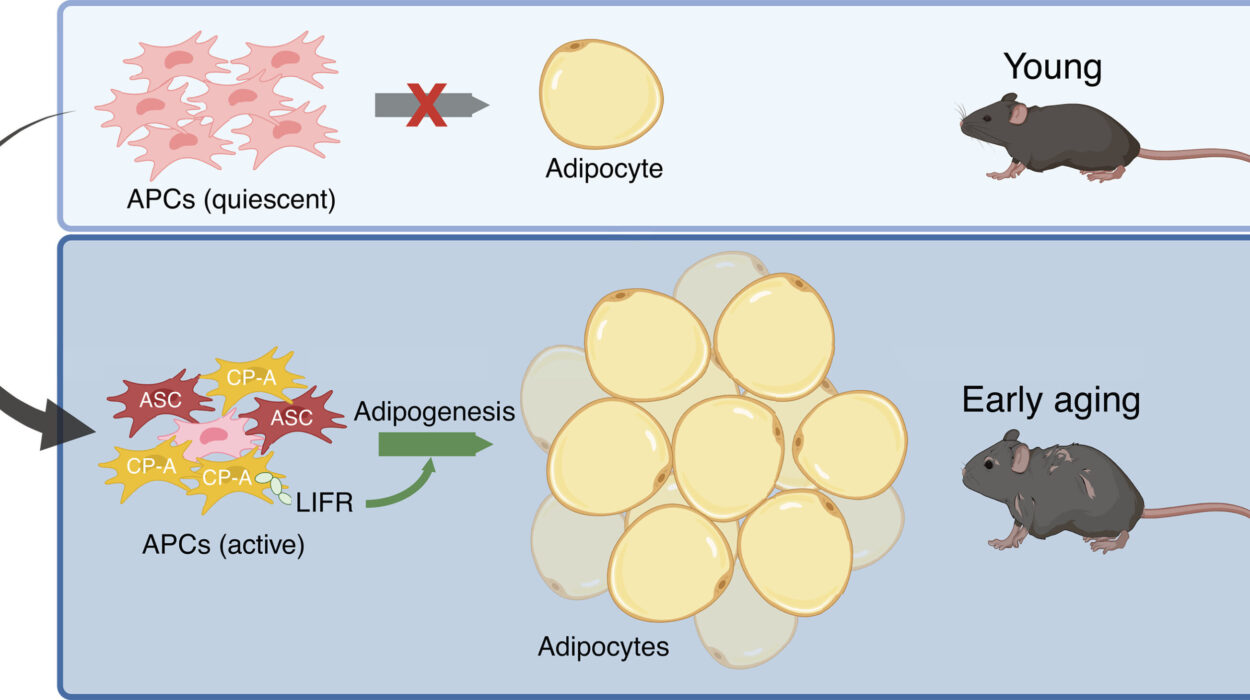
The Strange Ecosystem of the Tumor Microenvironment
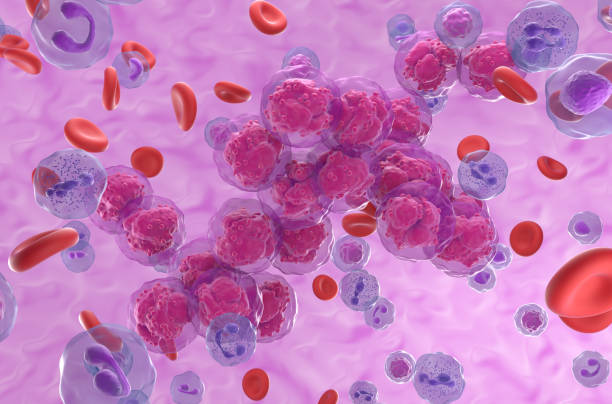
Tumors are more than just collections of mutated cells. They are ecosystems, made up of not only cancer cells but also healthy cells that have been co-opted, tricked, or trapped. Fibroblasts, immune cells, blood vessels, and extracellular matrix components all contribute to what’s called the tumor microenvironment.
This environment shapes how cancer behaves. It can promote or inhibit growth, help resist drugs, or even support metastasis. In some cancers, cells in the microenvironment begin to behave almost like accomplices, reinforcing the tumor’s defenses.
Scientists are now learning to target not just the cancer cells themselves but also this supportive neighborhood—disrupting the conditions that allow the tumor to thrive. It’s a shift in thinking that recognizes cancer not just as a cellular defect, but as a community of dysfunction.
When Cancer Spreads and the Body Fights Back
Local tumors can often be removed with surgery or treated with localized radiation. But when cancer spreads—when it metastasizes—it becomes much harder to treat. This is because metastatic cells travel through the blood or lymphatic system and settle in new tissues, forming secondary tumors.
These new sites are often more resistant to therapy. Metastatic cells may have different mutations than the original tumor, and their new location may protect them from immune attack or drug penetration. Once cancer has spread to multiple organs, treatment becomes a systemic challenge rather than a localized fix.
Yet even in the face of this spread, the body does not give up. The immune system continues to fight. Doctors apply new strategies—chemotherapy, targeted therapies, immunotherapies, hormone treatments, and more—each aiming to disrupt cancer’s progress. Some patients achieve remission. Others live with cancer as a chronic disease for years.
And behind the scenes, researchers push forward—mapping tumor genomes, studying resistance mechanisms, and testing new drugs that exploit cancer’s weaknesses.
The Genetic Fingerprint of Each Tumor
Thanks to advances in genomics, we now understand that no two cancers are exactly alike. Even within the same type—say, breast cancer or colon cancer—there can be enormous genetic diversity between patients. This has led to a new era of personalized medicine, where treatments are tailored not just to the location of a tumor but to its unique molecular signature.
By sequencing the DNA of a tumor, doctors can identify specific mutations driving its growth and choose drugs that target those mutations. This approach, called precision oncology, is changing the way we treat cancer—from a one-size-fits-all strategy to a custom battle plan.
It’s not just about the cancer’s genetics, either. Scientists now study how cancer cells respond to stress, how they use energy, and how they communicate with neighboring cells. All of this information helps refine treatment, improve outcomes, and reduce side effects.
Still, cancer adapts. Tumors evolve under the pressure of therapy, sometimes developing resistance to even the most advanced drugs. This is why many researchers are turning to combination therapies—attacking the cancer from multiple angles at once, making it harder for resistance to take hold.
Hope, Progress, and the Long Road Ahead
There is no single cure for cancer because there is no single cancer. It is a diverse, adaptable, and evolving family of diseases. But progress has been undeniable. Survival rates for many cancers have improved dramatically in recent decades. Treatments have become less toxic, more targeted, and more effective.
We’ve gone from a time when cancer was spoken of in hushed tones to an era where survivors speak out, raise funds, and advocate for research. Major breakthroughs—like CAR-T cell therapy, checkpoint inhibitors, and molecular diagnostics—have transformed outcomes for some patients who would have had little hope just years ago.
And more advances are coming. Scientists are exploring the microbiome’s influence on cancer, using artificial intelligence to predict treatment responses, and developing vaccines that train the immune system to prevent recurrence. The frontier is vast, and the pace of discovery is accelerating.
Cancer as a Window Into Life Itself
Perhaps one of the most profound insights from cancer research is how much it reveals about life itself. Cancer is not just a disease—it is a malfunction of the very processes that make life possible. Cell division, DNA repair, growth signaling, and tissue organization are essential for development and healing. But when they go awry, they can become instruments of destruction.
In studying cancer, we learn not only how things go wrong but how they normally go right. Every new discovery deepens our understanding of biology, from embryonic development to aging and regeneration.
In this way, cancer research is more than a fight against disease. It is a journey into the machinery of life, into the code that shapes us, and into the evolutionary logic that governs our cells.
Living With the Enemy and Redefining the Battle
For many people today, cancer is no longer a death sentence. It is a chronic condition to be managed. Some cancers never spread. Others respond well to early treatment. And in some cases, the goal shifts from cure to control—to keep the disease in check, preserve quality of life, and extend survival.
This shift in mindset is important. It changes how we talk about cancer, how we treat it, and how we support those who live with it. It also opens the door to new approaches that aim not to eradicate every last cell but to reshape the tumor environment, suppress its growth, and prevent flare-ups.
Living with cancer is not easy. But with knowledge, support, and continued scientific progress, more people are doing just that—living longer, fuller lives despite the disease.
The Future Written in Cells
Cancer begins in the smallest units of life, but it carries implications that are deeply human. It touches our fears, our hopes, our science, and our stories. Each diagnosis is personal. Each battle is unique. And each breakthrough ripples outward, offering new tools, new understanding, and new reasons to believe.
We may never eliminate cancer completely. But we are learning to outthink it, outmaneuver it, and outlast it. The rogue cell, once invisible and unstoppable, is now being unmasked. And in that unmasking, we glimpse something powerful—not just the threat of disease, but the resilience of life.