In a discovery that could mark a turning point in the fight against Alzheimer’s disease, researchers at the University of California, Irvine have identified a promising new way to revive aging brain cells and clear out the harmful proteins at the heart of this devastating illness—all without the use of pharmaceutical drugs.
Published in the journal GeroScience, the study shows that a simple combination of naturally occurring compounds—nicotinamide, a form of vitamin B3, and epigallocatechin gallate (EGCG), a potent antioxidant found in green tea—can restore essential energy levels in neurons. The treatment improved the brain cells’ ability to clear toxic amyloid plaques, which are widely believed to contribute to the progression of Alzheimer’s disease.
The implications are as startling as they are hopeful: by recharging the energy systems within neurons, the aging brain might recover its natural capacity to clean itself, resist damage, and even reverse early signs of neurodegeneration.
Aging, Energy, and the Cleanup Crisis in the Brain
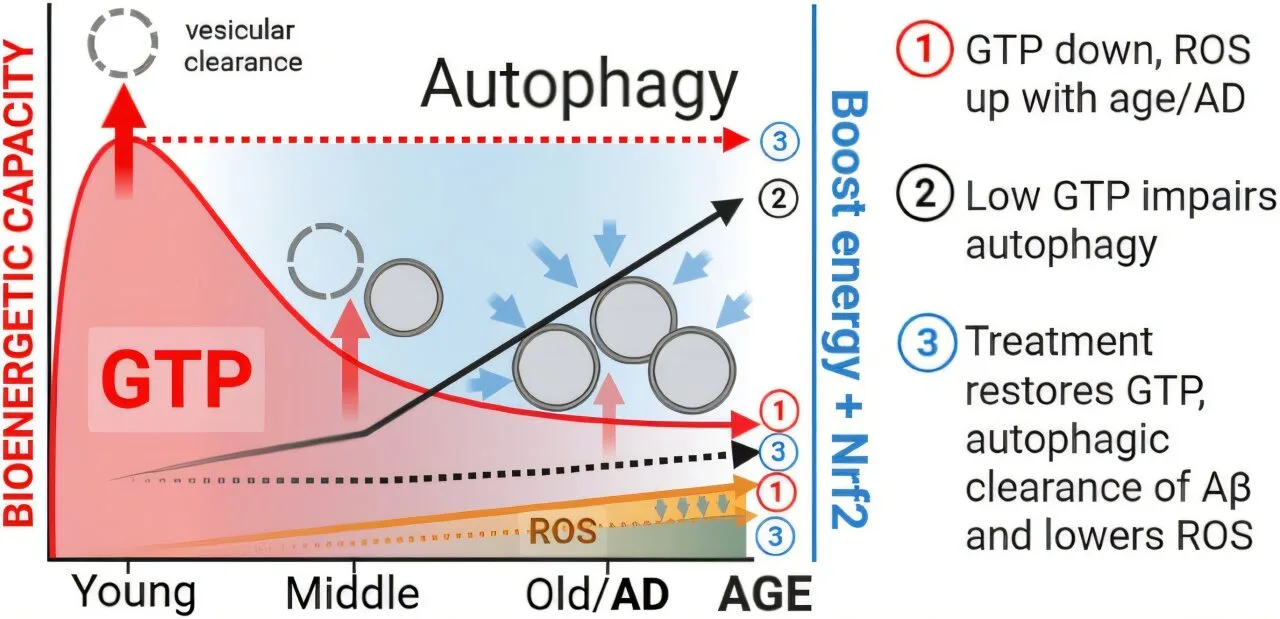
As we age, our brains don’t just slow down—they start losing the internal energy necessary for vital housekeeping. This decline in energy makes it harder for neurons to perform autophagy, the internal cleanup process that removes damaged parts and toxic proteins. In Alzheimer’s, this impairment is especially catastrophic.
“Our brains need energy not just to think, but to take out the trash,” explained Dr. Gregory Brewer, the study’s lead author and adjunct professor of biomedical engineering at UC Irvine. “When that energy dips too low with age, neurons start failing to clear out harmful substances like amyloid beta proteins, which then pile up and destroy brain function.”
Brewer’s team used a sophisticated imaging tool called GEVAL, a genetically encoded fluorescent sensor, to watch how guanosine triphosphate (GTP)—a key molecule for cellular energy—declines in aged neurons. Their results showed that in older brain cells, GTP levels were markedly reduced, especially within mitochondria, the cell’s primary energy producers.
This GTP deficiency crippled the neurons’ ability to perform autophagy and led to dangerous buildups of amyloid beta, one of the biological hallmarks of Alzheimer’s disease.
Nature’s Toolkit: How Nicotinamide and Green Tea Made a Difference
The researchers then tested whether supplementing aging neurons with nicotinamide and EGCG could restore their energy and function. Remarkably, after just 24 hours of treatment, GTP levels rebounded to those typically seen in young brain cells.
That simple boost set off a chain reaction: the cells’ energy metabolism improved, oxidative stress diminished, and key cellular pathways linked to waste clearance—specifically the GTPase proteins Rab7 and Arl8b—were reactivated. Most importantly, the neurons began clearing amyloid beta aggregates more efficiently, suggesting that even in an aging brain, the capacity for self-repair can be reignited.
“This study highlights GTP as a previously underappreciated energy source driving vital brain functions,” Brewer said. “We’re essentially giving neurons the fuel they need to start cleaning up after themselves again.”
Not Just Another Supplement—A Potential Therapeutic Pathway
While both nicotinamide and EGCG are already available as over-the-counter dietary supplements, Brewer is cautious about jumping straight from the lab bench to the health store shelf. A recent clinical trial at UC Irvine showed that oral nicotinamide had limited effectiveness, likely because the compound was inactivated in the bloodstream before it could reach the brain.
“This doesn’t mean the idea doesn’t work—it means we need to find the right delivery method,” Brewer emphasized. “Whether that’s a different formulation, intravenous delivery, or something else entirely remains to be seen.”
Still, the results offer a compelling new angle on treating age-related brain decline—not by targeting amyloid plaques directly, but by restoring the cell’s ability to handle them.
“Instead of sweeping harder,” Brewer noted, “we’re fixing the broom.”
Redefining the Role of Energy in Brain Health
One of the most profound aspects of this study is its redefinition of what drives brain health in aging. Traditionally, treatments have focused on attacking the visible hallmarks of Alzheimer’s—like plaques and tangles—but this research shifts attention back to the metabolic machinery of the cell.
“People think about glucose and ATP when they think about energy in the brain,” said co-author Ricardo Santana, a UC Irvine associate specialist in biomedical engineering. “But GTP is critical too, especially in the processes that move cargo inside cells and control protein recycling. It’s been overlooked for too long.”
The identification of GTP as a central player opens new doors for understanding—and potentially treating—not just Alzheimer’s, but other neurodegenerative diseases that also involve energy deficits and protein mismanagement, such as Parkinson’s and Huntington’s disease.
A Hopeful Step Toward a Disease-Free Mind
Though this discovery is still in its early stages and primarily based on cell culture models, the results are energizing for a field that has faced repeated disappointments in the search for a cure for Alzheimer’s. Traditional drug development has struggled to produce effective therapies, and most pharmaceutical interventions have offered only modest benefits.
What makes this study stand out is its nonpharmaceutical approach: a strategy that works with the brain’s natural systems rather than against them. It’s also a gentle reminder that compounds found in our everyday diet might hold powerful secrets when studied deeply and used wisely.
Joshua McWhirt, a junior specialist at UC Irvine and now a Ph.D. candidate at the Medical University of South Carolina, was instrumental in executing the experiments. “This isn’t just a lab curiosity,” he said. “We’re looking at something that could change how we think about aging, energy, and healing the brain.”
Where Science Goes Next
There’s still a long journey ahead before this treatment could be available to patients. The next steps will involve animal studies to confirm the cellular results in living brains, followed by careful development of delivery methods that ensure the compounds reach their targets intact.
If successful, these compounds—or improved versions of them—might one day form part of a new class of therapies aimed not just at treating symptoms, but restoring function in the aging brain.
“We’re not promising a cure,” Brewer said. “But we are pointing toward a pathway that’s been largely ignored—and it’s one that appears to work with the brain’s own ability to heal.”
In a world where the burden of dementia is growing by the day, such a path is worth following.
More information: R. A. Santana et al, Treatment of age-related decreases in GTP levels restores endocytosis and autophagy, GeroScience (2025). DOI: 10.1007/s11357-025-01786-4