The human brain is the most complex structure known to science. It is the command center of our bodies, controlling thoughts, emotions, memory, movement, and the very sense of who we are. When something as invasive as a tumor develops inside this delicate organ, it disrupts not only biological functions but also a person’s identity and quality of life. Brain tumors are not just a medical condition; they are a profound human challenge that affects patients and their families emotionally, physically, and socially.
To understand brain tumors fully, we must explore their causes, symptoms, methods of diagnosis, and available treatments. This journey into the world of neuro-oncology is not only about biology and medicine but also about resilience, hope, and the relentless effort of science to preserve life and dignity.
What Are Brain Tumors?
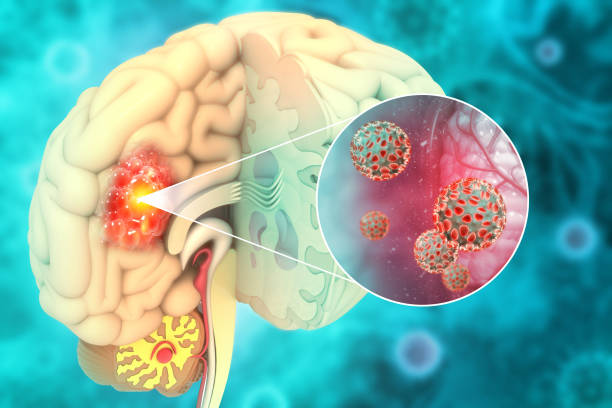
A brain tumor is an abnormal growth of cells within the brain or the tissues surrounding it. Unlike most organs, the brain exists in a rigid skull that leaves little room for expansion. As a result, even a small mass can disrupt vital functions.
Tumors may be benign (noncancerous) or malignant (cancerous). Benign tumors generally grow slowly and do not spread to other parts of the body. However, within the confined space of the skull, they can still cause significant harm by compressing brain tissue, blocking cerebrospinal fluid pathways, or increasing intracranial pressure. Malignant tumors, by contrast, grow aggressively and may infiltrate surrounding tissues, making them more dangerous and difficult to treat.
Brain tumors are also classified as primary or secondary. Primary tumors originate in the brain itself, while secondary (metastatic) tumors spread from cancers in other parts of the body, such as the lungs, breasts, or skin. Metastatic tumors are more common than primary brain tumors, highlighting the interconnectedness of systemic disease and neurological health.
Causes of Brain Tumors
One of the most challenging questions in medicine is: Why do brain tumors form? The answer is complex, involving genetic, environmental, and lifestyle factors.
Genetic Mutations and Cellular Changes
At the core of brain tumor formation lies a breakdown in normal cellular regulation. Healthy cells grow, divide, and die in a controlled cycle. In tumors, mutations disrupt this balance, causing cells to grow uncontrollably. These mutations may affect oncogenes (genes that promote growth) or tumor suppressor genes (genes that prevent overgrowth).
Some brain tumors are linked to inherited genetic syndromes. For example:
- Li-Fraumeni syndrome increases the risk of gliomas.
- Neurofibromatosis type 1 and 2 predispose individuals to tumors like schwannomas and meningiomas.
- Turcot syndrome is associated with brain tumors and colon cancer.
However, inherited syndromes account for only a small fraction of cases. Most genetic changes are acquired during life rather than inherited.
Environmental and Lifestyle Factors
Scientists continue to investigate environmental contributors. Exposure to ionizing radiation is a well-documented risk, whether from therapeutic treatments in childhood or rare accidental exposures. Other suspected contributors—such as long-term exposure to certain chemicals, pesticides, or industrial pollutants—remain less clearly defined but are areas of active research.
Lifestyle factors, such as diet, physical activity, and smoking, have stronger links to systemic cancers but are less directly tied to brain tumors. However, obesity and immune suppression can indirectly increase risk.
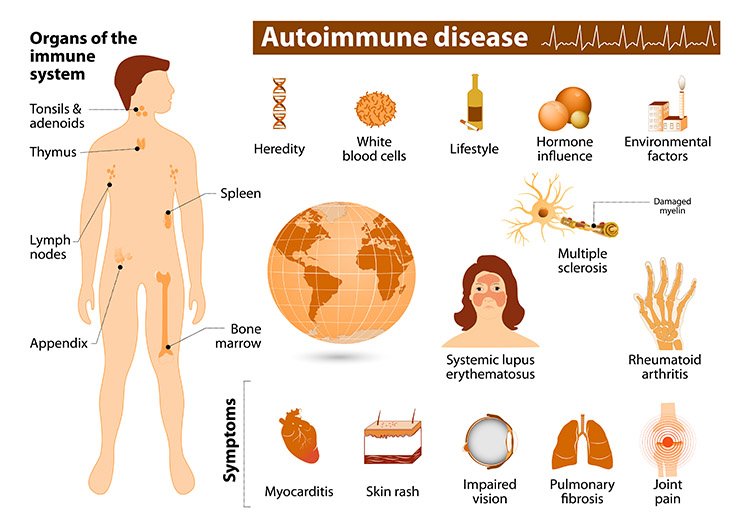
The Role of the Immune System
The immune system plays a crucial role in identifying and eliminating abnormal cells. When it falters—whether due to disease, medications, or aging—abnormal cells may escape detection and form tumors. This may explain why individuals with HIV/AIDS or those on long-term immunosuppressive therapy are at higher risk for certain brain tumors, like primary central nervous system lymphoma.
The Mystery That Remains
Despite these known factors, the majority of brain tumor cases arise without clear causes. This uncertainty adds to the emotional burden for patients and families, who often search for explanations where science cannot yet provide definitive answers.
Symptoms of Brain Tumors
Brain tumors announce themselves in diverse ways. The specific symptoms depend on the tumor’s size, growth rate, and location. Because different brain regions control different functions, tumors in each area produce unique patterns of disturbance.
General Symptoms
Some symptoms arise from the pressure that tumors exert on brain tissue, regardless of location. These include:
- Headaches that worsen in the morning or with activity.
- Nausea and vomiting due to increased intracranial pressure.
- Seizures, which may be the first sign in many patients.
- Cognitive or personality changes, such as confusion, memory loss, or mood swings.
Location-Specific Symptoms
- Frontal lobe tumors may alter personality, decision-making, and movement.
- Temporal lobe tumors can affect speech, memory, and emotional regulation.
- Parietal lobe tumors may interfere with sensation, spatial awareness, and coordination.
- Occipital lobe tumors often produce visual disturbances or loss of vision.
- Cerebellar tumors disrupt balance, coordination, and fine motor skills.
- Brainstem tumors can impair vital functions like breathing, heartbeat, and swallowing.
The variability of these symptoms means that brain tumors are often mistaken for other conditions, leading to delays in diagnosis.
Diagnosis of Brain Tumors
The path to diagnosis begins with careful observation of symptoms, but it relies heavily on advanced medical imaging and laboratory techniques.
Neurological Examination
Doctors assess reflexes, coordination, balance, vision, hearing, and cognitive function. This initial evaluation often suggests which part of the brain may be affected.
Imaging Technologies
- Magnetic Resonance Imaging (MRI): The gold standard, offering detailed images of soft tissues. Specialized forms like functional MRI or diffusion tensor imaging reveal brain activity and connections.
- Computed Tomography (CT): Useful in emergencies, particularly for detecting bleeding or calcifications.
- Positron Emission Tomography (PET): Provides metabolic insights, distinguishing between tumor tissue and scar tissue.
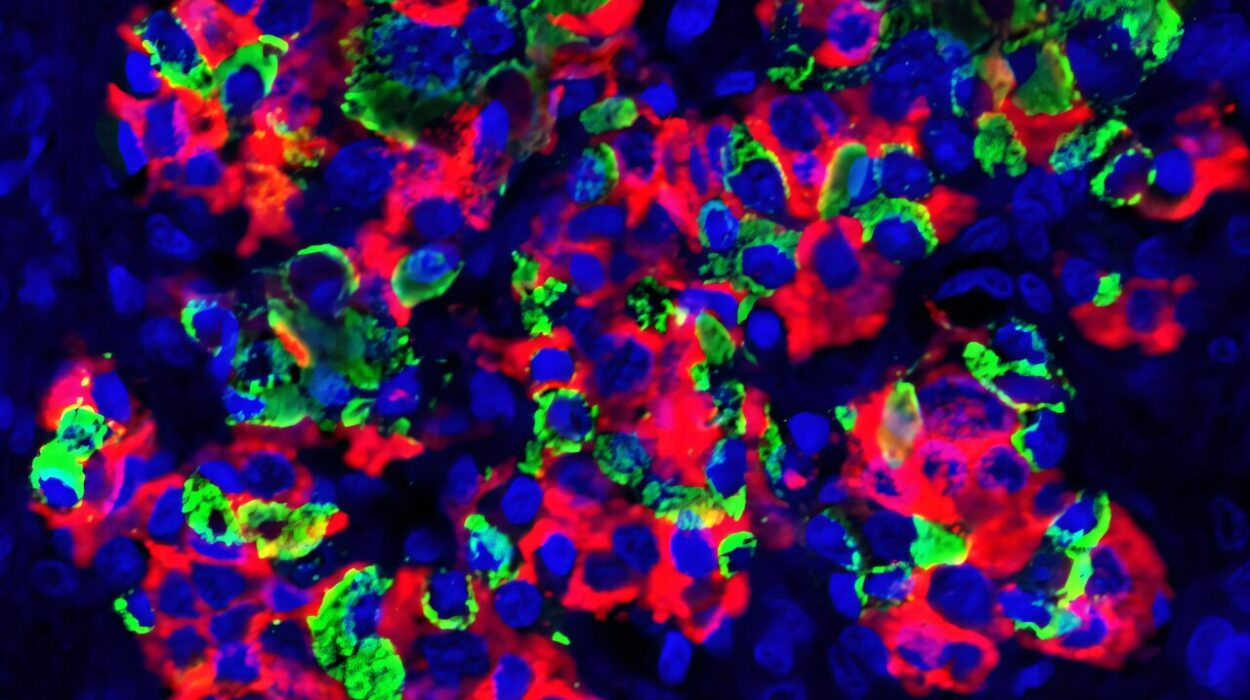
Biopsy and Histological Analysis
Definitive diagnosis requires examining tumor tissue under a microscope. Biopsies can be performed via surgery or minimally invasive stereotactic techniques. Pathologists classify tumors based on cell type and grade, following the World Health Organization (WHO) classification system.
Molecular and Genetic Profiling
Modern medicine increasingly uses genetic analysis to understand tumor biology. Identifying mutations in genes like IDH1, TP53, or EGFR not only aids classification but also guides targeted therapies. This shift toward precision medicine is transforming the landscape of brain tumor care.
Treatment of Brain Tumors
Treating brain tumors is one of the most challenging tasks in medicine. The brain’s complexity, the diversity of tumor types, and the risks of damaging healthy tissue demand highly specialized and individualized approaches.
Surgery
Surgical removal is often the first step, especially for accessible tumors. The goal is maximal safe resection—removing as much tumor as possible while preserving brain function.
Modern techniques, such as intraoperative MRI, awake brain surgery, and neuronavigation, have greatly improved precision. For some tumors, complete removal is possible; for others, only partial resection can be achieved. Even partial removal, however, can relieve pressure and improve outcomes.
Radiation Therapy
Radiation uses high-energy beams to target and destroy tumor cells. It is often employed after surgery to eliminate residual cells or as the primary treatment for inoperable tumors.
Techniques include:
- External beam radiation therapy (EBRT), the most common form.
- Stereotactic radiosurgery (e.g., Gamma Knife, CyberKnife), delivering highly focused doses with minimal damage to surrounding tissue.
- Proton beam therapy, which offers precise targeting with reduced side effects.
Chemotherapy
Chemotherapy uses drugs to kill rapidly dividing cells. While its role in brain tumors is more limited than in other cancers, agents like temozolomide have shown effectiveness, especially for glioblastoma.
Because the blood-brain barrier protects the brain from toxins—and unfortunately, from many chemotherapy drugs—delivering effective doses is challenging. Research into novel delivery systems, such as nanoparticles and direct infusion, is ongoing.
Targeted Therapy and Immunotherapy
The newest frontier in treatment involves therapies tailored to the tumor’s genetic and molecular profile. Targeted drugs block specific growth signals in tumor cells, while immunotherapies harness the body’s immune system to fight cancer.
Checkpoint inhibitors, CAR-T cell therapy, and cancer vaccines are being tested for brain tumors. While still in early stages, these approaches represent hope for more effective and less toxic treatments.
Supportive and Palliative Care
Not all tumors are curable, but every patient deserves quality of life. Supportive care includes managing seizures, reducing swelling with steroids, controlling pain, and providing psychological support. Palliative care focuses on dignity, comfort, and emotional well-being, reminding us that health is not just survival but the ability to live meaningfully even in the face of illness.
Living with a Brain Tumor
A diagnosis of a brain tumor is life-changing. It challenges not only the patient but also families and caregivers. Emotional responses range from fear and anger to resilience and hope. Support groups, counseling, and rehabilitation programs are essential for helping patients adapt.
Rehabilitation may include physical therapy, occupational therapy, speech therapy, and cognitive training to restore lost functions. Equally important is addressing the emotional and social impact—helping patients rebuild confidence, maintain relationships, and find meaning in life despite uncertainty.
The Future of Brain Tumor Research
The fight against brain tumors continues in laboratories and clinics worldwide. Advances in genetics, stem cell research, and artificial intelligence are opening new possibilities. AI algorithms now assist in analyzing imaging data, predicting tumor behavior, and guiding surgical precision. Stem cell research may one day offer regenerative treatments for damaged brain tissue.
Perhaps most inspiring is the global collaboration of scientists, doctors, and patients pushing forward research. Clinical trials test innovative therapies, while advocacy groups raise awareness and funds. The shared determination to defeat brain tumors is itself a testament to human resilience.
Conclusion: Science, Humanity, and Hope
Brain tumors are among the most daunting challenges in medicine. They arise from mysterious causes, present with complex symptoms, and demand intricate treatments. Yet, the story of brain tumors is not one of despair but of courage, progress, and hope.
Every breakthrough in imaging, surgery, radiation, and molecular medicine represents not just a scientific victory but a human triumph. Each patient who fights, each family that supports, and each doctor or researcher who dedicates their life to this cause embodies the resilience of the human spirit.
To ask about brain tumors is to ask about life itself—its fragility, its resilience, and the endless drive to understand and preserve it. While science continues its pursuit of cures, one truth remains: within the challenge of brain tumors lies the opportunity to discover not only medical solutions but also the depths of compassion, strength, and hope that define humanity.