In the quiet corridors of the University of Minnesota’s Masonic Cancer Center, a medical revolution is taking shape—one that could redefine the boundaries of cancer therapy. A pioneering team of researchers and clinicians has just completed the world’s first human trial using CRISPR/Cas9 gene-editing technology to supercharge the body’s immune response against some of the deadliest gastrointestinal (GI) cancers. And the early results are nothing short of remarkable.
Published in the prestigious Lancet Oncology, the study has already captured global attention—not just for its scientific innovation, but for the profound implications it holds for cancer patients with few remaining options. What if the key to defeating cancer isn’t external chemotherapy or radiation, but lies deep within our own immune systems—just waiting to be unlocked?
From Lab Bench to Hospital Bedside
Dr. Emil Lou, a physician-scientist and gastrointestinal oncologist at the University of Minnesota Medical School and M Health Fairview, has spent years staring down the harsh realities of advanced colorectal cancer. Stage IV disease, particularly when metastatic, remains among the most difficult to treat. “Despite many advances in understanding the genomic drivers and other factors causing cancer, with few exceptions, stage IV colorectal cancer remains a largely incurable disease,” said Dr. Lou, who served as the principal clinical investigator for the trial.
But this clinical trial, emerging directly from decades of molecular and genetic research, signals a fresh direction. Unlike conventional therapies that often treat cancer with a carpet-bombing approach—damaging healthy and malignant cells alike—this technique turns cancer’s own nemesis into a precision weapon: the patient’s immune system.
The Gene Behind the Barrier: Targeting CISH
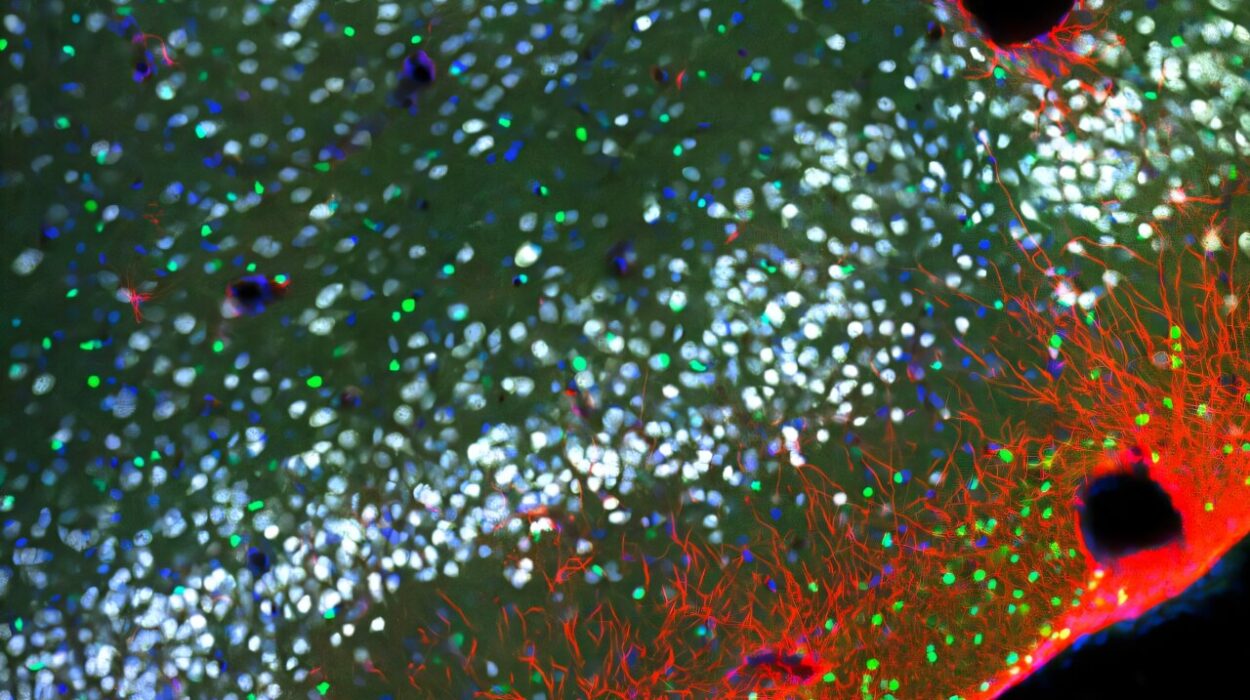
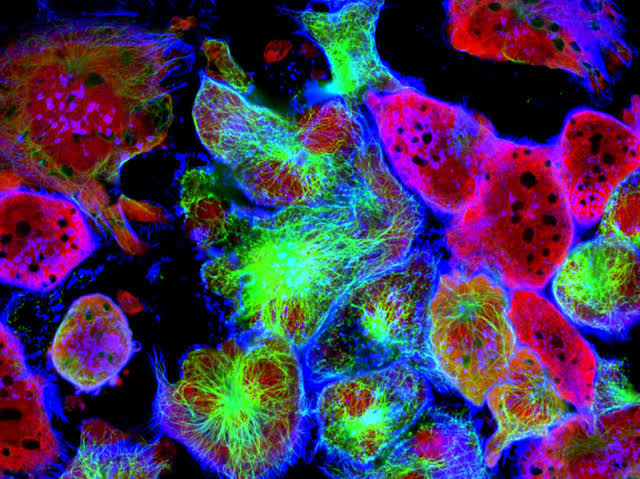
At the heart of this new therapy lies a gene called CISH—a relatively obscure but powerful regulator that acts like a brake on the immune system’s most potent cancer-fighting soldiers: T cells. Specifically, the team focused on tumor-infiltrating lymphocytes (TILs), a specialized subset of immune cells that already exist within tumors and have shown promise in attacking cancerous tissue.
While TILs naturally recognize and respond to cancer cells, their effectiveness can be muted by internal signals—particularly from the CISH gene. CISH effectively tells T cells to “stand down” rather than launching an all-out assault on tumors.
“Because it acts inside the cell, it couldn’t be blocked using traditional methods,” explained Dr. Branden Moriarity, a co-leader of the study and associate professor at the University of Minnesota Medical School. “So we turned to CRISPR-based genetic engineering.”
Using CRISPR/Cas9—a revolutionary gene-editing tool that acts like molecular scissors—the researchers precisely deleted the CISH gene from the DNA of harvested TILs. The result? A set of hyper-responsive immune cells, genetically optimized to recognize, attack, and destroy cancer cells without the suppressive interference of CISH.
Engineering a Cellular Army
The process of preparing these cells for reinfusion is no simple feat. First, TILs are extracted from a patient’s tumor. Then, in a sterile laboratory environment that meets the strictest clinical manufacturing standards, researchers use CRISPR/Cas9 to delete the CISH gene from millions of cells. These cells are then expanded in number—eventually reaching quantities exceeding 10 billion genetically modified TILs—before being infused back into the patient.
“Delivering this many gene-edited cells without causing adverse side effects has never been done before,” said Dr. Beau Webber, a co-author of the study and associate professor at the University of Minnesota. “But our work proves it can be done safely and at scale.”
This is not simply a tweak or a temporary fix. The genetic changes are permanent and intrinsic to the T cells. Unlike other immunotherapies that rely on repeated administration or temporary modifications, this CRISPR-based approach essentially rewires the immune system for long-term vigilance.
“With our gene-editing approach, the checkpoint inhibition is accomplished in one step and is permanently hardwired into the T cells,” Webber noted.
Trial Results: Safety, Success, and One Extraordinary Response
Twelve patients with metastatic, late-stage gastrointestinal cancers were enrolled in the first-in-human trial. These were individuals for whom standard therapies had failed—patients facing the bleak landscape of cancer with no remaining treatment options.
The results were cautiously optimistic. The treatment was generally well tolerated, with no serious side effects directly linked to the gene-editing procedure. Several patients experienced disease stabilization, meaning their cancers stopped progressing. But one patient experienced a result that electrified the team: a complete response.
Over the course of several months, this individual’s metastatic tumors completely disappeared. Two years later, the cancer remains undetectable—a rare and extraordinary outcome in stage IV gastrointestinal oncology.
“This patient’s experience gives us real hope,” Dr. Lou said. “It suggests that by empowering the immune system in just the right way, we can potentially change the natural history of this disease.”
The Future: Challenges and Possibilities
While the science is promising, it is not without its challenges. The CRISPR-based process, from gene editing to cell expansion, is costly, labor-intensive, and complex. Each batch of modified TILs must be tailored to the individual patient—personalized cellular medicine at its most extreme. At present, the technology requires sophisticated lab infrastructure and weeks of processing time.
But these hurdles, researchers believe, are temporary. The team is actively working to streamline the production pipeline, reduce costs, and develop automation strategies. They’re also conducting deep molecular analyses to determine why the therapy worked so spectacularly in the patient with the complete response—and how to replicate that success across a broader patient population.
“Our hope is to identify biomarkers or patterns that predict which patients will benefit most,” said Dr. Moriarity. “If we can personalize this approach even further, we can increase the chances of success for every patient.”
A Glimpse into the Next Era of Oncology
What sets this research apart from other cutting-edge cancer therapies is its elegant simplicity and profound complexity at once. It doesn’t rely on drugs, radiation, or external agents. Instead, it reactivates a natural defense system—reprogramming cells already primed for battle and sending them back into the fray with new instructions and capabilities.
It’s also a striking example of the promise of CRISPR beyond inherited diseases. While the gene-editing tool is perhaps best known for correcting mutations in genetic disorders, this trial reveals its potential to fight diseases acquired later in life—like cancer—by reengineering our own biology.
For patients and families facing the devastating diagnosis of metastatic GI cancer, this approach offers more than a glimmer of hope. It represents a fundamentally new paradigm: treating cancer not just by fighting the disease, but by enhancing the body’s natural ability to eliminate it.
Ethical Precision and Scientific Courage
As with any new biomedical frontier, the ethical considerations are significant. Gene editing in humans—particularly in a clinical setting—requires extreme precision and oversight. The research team worked under rigorous regulatory guidance and ensured that patients gave full informed consent. Their work not only abides by the highest ethical standards but may serve as a blueprint for future gene-editing therapies in cancer and beyond.
CRISPR is often described as the most powerful genetic tool of our time, but tools are only as transformative as the visionaries who wield them. In this case, the vision was both bold and deeply humane: What if cancer’s endgame could be rewritten from within?
Conclusion: A Turning Point in Cancer Therapy
The University of Minnesota team’s CRISPR-enhanced TIL therapy is more than a scientific milestone—it’s a beacon for what the future of cancer treatment might look like. No longer confined to attacking tumors from the outside, researchers are now learning how to awaken and refine the body’s internal arsenal with molecular precision.
There is still a long journey ahead. But with each trial, each patient, and each promising response, the path forward becomes clearer. The idea that stage IV cancer could be reversed—or even cured—by gene-edited immune cells is no longer science fiction. It is science in motion.
And for the patients who are now living longer, stronger, and with new hope, that motion is everything.
Reference: Emil Lou et al, Targeting the intracellular immune checkpoint CISH with CRISPR-Cas9-edited T cells in patients with metastatic colorectal cancer: a first-in-human, single-centre, phase 1 trial, The Lancet Oncology (2025). DOI: 10.1016/S1470-2045(25)00083-X