For centuries, people have described having a “gut feeling” or feeling “sick to the stomach” when anxious or upset. While these expressions might have seemed metaphorical in the past, modern science is uncovering just how literal they are. There’s a profound and intricate connection between your digestive system and your brain—a connection that researchers are calling the “gut-brain axis.”
The gut is no longer seen merely as a system for digesting food. It is now understood as a complex, semi-autonomous organ that plays a vital role in mental well-being. From mood and behavior to memory and emotional resilience, your gut can shape your mind in ways most people never imagined. In this article, we’ll explore the fascinating link between gut health and mental health, how your digestive system communicates with your brain, and what you can do to nurture both.
Understanding the Gut-Brain Axis: Two Minds, One System
The gut-brain axis is a bidirectional communication network that connects your central nervous system (CNS) with your enteric nervous system (ENS)—often referred to as the “second brain.” This network uses neural, hormonal, and immunological signaling to allow constant dialogue between your digestive tract and your brain.
At the heart of this communication is the vagus nerve, the longest cranial nerve in the body. It acts as a superhighway, transmitting signals both from the brain to the gut and vice versa. But that’s just the start. The gut also produces neurotransmitters, sends hormonal messengers, and houses immune cells—all of which influence how we think and feel.
While the brain controls complex thoughts and decision-making, the gut houses over 500 million neurons—more than the spinal cord—and plays a direct role in generating emotions, processing stress, and modulating mental health.
The Microbiome: Your Invisible Inner World
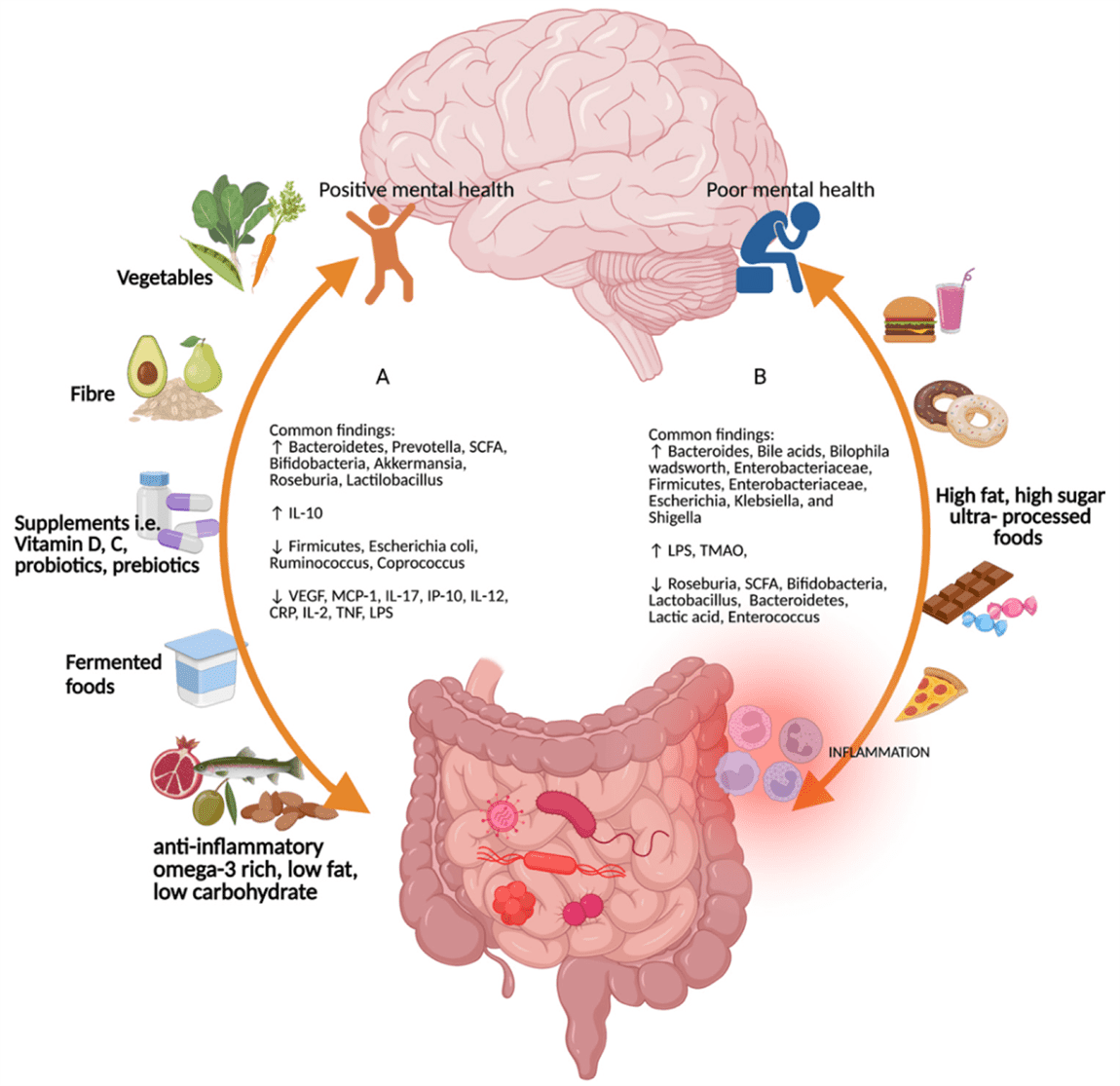
One of the most exciting discoveries of the last decade is the role of the gut microbiome in shaping mental health. The microbiome is a vast community of trillions of microorganisms—bacteria, viruses, fungi, and more—that live in your digestive tract. Each person’s microbiome is unique, much like a fingerprint, and these tiny tenants perform crucial tasks such as:
- Aiding in digestion and nutrient absorption
- Producing vitamins and hormones
- Training the immune system
- Synthesizing neurotransmitters like serotonin and GABA
A balanced microbiome acts like a well-functioning ecosystem, fostering health and harmony. But when it’s disrupted—a state known as dysbiosis—it can trigger inflammation, mood disorders, and even neurochemical imbalances that affect cognition and behavior.
Serotonin and the Gut: The Happiness Connection
Most people associate serotonin with the brain. After all, it’s the “feel-good” neurotransmitter that regulates mood, sleep, and appetite. What’s less known is that nearly 90% of the body’s serotonin is produced in the gut.
Specialized cells in the lining of the gastrointestinal tract, known as enterochromaffin cells, manufacture serotonin. This serotonin doesn’t just help regulate gut motility; it also signals the brain and helps modulate mood and emotional states.
An imbalance in gut bacteria can lead to reduced serotonin production, contributing to symptoms of depression, anxiety, and emotional instability. This makes gut health a major factor in mental wellness—and a potential therapeutic target for mood disorders.
Inflammation and the Gut-Brain Firestorm
Inflammation is a natural immune response, but chronic low-grade inflammation is a silent saboteur, especially when it originates in the gut. When the gut lining becomes permeable—a condition often referred to as “leaky gut”—undigested food particles and toxins can escape into the bloodstream, triggering systemic inflammation.
This inflammation doesn’t stay in the gut. It can cross the blood-brain barrier, affecting brain function and mood regulation. Pro-inflammatory cytokines have been shown to interfere with neurotransmitter signaling, alter neuroplasticity, and even contribute to symptoms of depression and anxiety.
In essence, a troubled gut creates a ripple effect of inflammation that can cloud thinking, dampen mood, and amplify stress. Healing the gut, then, is about more than digestion—it’s about cooling an inflammatory storm that may be burning in both the belly and the brain.
Anxiety and the Gut: A Two-Way Street
Have you ever felt butterflies in your stomach before a big presentation? Or lost your appetite during times of extreme stress? These are textbook examples of how psychological stress affects the gut. But the reverse is also true: an imbalanced gut can trigger or worsen anxiety.
When the microbiome is out of balance, the vagus nerve can carry distress signals to the brain, activating the body’s stress response. At the same time, poor gut health may reduce levels of calming neurotransmitters like GABA, leading to a heightened state of anxiety.
This feedback loop means that anxiety and gut dysfunction often reinforce each other. Treating one without addressing the other is like trying to patch a leaking boat while ignoring the hole in the hull. True healing requires treating the gut and the mind as interconnected pieces of a larger puzzle.
Depression and the Digestive Tract
Depression is often treated as a purely neurological disorder, but emerging evidence shows that the gut may play a critical role. A disrupted microbiome, inflammation, and altered neurotransmitter production can all contribute to the symptoms of depression.
Interestingly, people with depression often experience gastrointestinal issues like constipation, bloating, or IBS. This overlap isn’t coincidental—it’s a reflection of the gut-brain axis in action. Studies have shown that restoring microbial balance through diet or probiotics can significantly improve depressive symptoms.
Furthermore, certain gut bacteria produce short-chain fatty acids (SCFAs) like butyrate, which have been shown to reduce inflammation and support brain health. When these beneficial microbes are wiped out—by stress, antibiotics, or poor diet—depression may deepen.
Stress and Digestion: A Delicate Dance
Stress doesn’t just affect your mind; it can wreak havoc on your digestive system. Chronic stress disrupts gut motility, alters microbial composition, and reduces digestive secretions. This can lead to bloating, discomfort, and nutrient malabsorption.
The body’s stress hormone, cortisol, also plays a dual role. While it helps you respond to immediate threats, chronic elevations can suppress immunity in the gut, weaken the intestinal lining, and shift microbial balance toward more harmful species.
On the flip side, poor gut health can increase the body’s sensitivity to stress, creating a vicious cycle. Healing this dynamic requires calming both the mind and the belly—often through lifestyle interventions like mindfulness, breathing exercises, and nutrition.
Childhood, Microbes, and Mental Health
The foundation for the gut-brain connection is laid early in life. The first three years are critical for establishing a healthy microbiome, and events during this time—such as mode of birth, breastfeeding, antibiotic use, and diet—can shape future mental health.
Children exposed to a diverse range of microbes early in life often develop more resilient immune systems and are less prone to allergies, anxiety, and mood disorders later on. Conversely, a sterile or disrupted microbial environment may increase the risk of developing neurodevelopmental conditions like ADHD, autism spectrum disorder, or anxiety.
This makes early-life gut care not just a digestive concern, but a mental health investment. It also highlights the importance of avoiding unnecessary antibiotics, promoting healthy diet diversity, and allowing children to interact with natural environments.
Food, Mood, and the Microbiome
You are what you eat, and nowhere is this more true than in the gut-brain connection. Diet plays a powerful role in shaping the microbiome—and, by extension, mental health.
Fiber-rich foods like fruits, vegetables, legumes, and whole grains nourish beneficial bacteria, leading to the production of SCFAs and other anti-inflammatory compounds. Fermented foods like yogurt, kefir, sauerkraut, and kimchi introduce probiotics that support microbial diversity.
On the other hand, diets high in sugar, processed foods, and artificial additives promote dysbiosis and inflammation. These foods may feed pathogenic bacteria, reduce microbial diversity, and increase the risk of mood disorders.
The Mediterranean diet—rich in fiber, healthy fats, and fermented foods—has been repeatedly associated with lower rates of depression and anxiety, in part due to its positive effects on gut health.
Psychobiotics: Probiotics for the Mind
A new class of probiotics, called “psychobiotics,” is gaining attention for its potential to support mental health. These are specific strains of bacteria shown to influence neurotransmitter production, reduce inflammation, and improve mood.
For example, certain strains of Lactobacillus and Bifidobacterium have been found to reduce symptoms of anxiety and depression in clinical studies. These bacteria interact with the vagus nerve, modulate immune responses, and even influence brain-derived neurotrophic factor (BDNF), which supports brain plasticity.
While psychobiotics are still an emerging field, they represent a promising frontier in mental health treatment—one that targets the gut as a doorway to the mind.
Sleep, Circadian Rhythms, and the Gut
Sleep and gut health are intricately linked. Your microbiome follows a circadian rhythm, with different species dominating at different times of day. Disruptions in sleep can alter these rhythms, affecting digestion, immunity, and mood.
Poor sleep reduces microbial diversity and increases inflammation. At the same time, a disrupted microbiome can impair melatonin production and disturb sleep quality. This reciprocal relationship means that improving sleep hygiene may benefit gut health—and vice versa.
Supporting circadian rhythms with regular sleep schedules, natural light exposure, and microbiome-friendly foods can enhance both mental clarity and digestive harmony.
Healing the Gut to Heal the Mind
The science is clear: a healthy gut lays the foundation for a healthy mind. So how can you support your gut-brain connection and promote mental well-being?
Start by focusing on dietary diversity. Include fiber-rich plant foods, fermented items, and prebiotic ingredients like garlic, onions, and bananas. Reduce consumption of processed foods, artificial sweeteners, and unnecessary antibiotics.
Manage stress through mindfulness, movement, and connection. Practice relaxation techniques, spend time in nature, and prioritize meaningful relationships. These behaviors nurture both your mental health and your gut flora.
Consider probiotics or psychobiotics if recommended by a healthcare provider. And remember: while supplements can help, nothing replaces a balanced lifestyle and a nurturing approach to food and self-care.
Conclusion: Listening to Your Inner Voice
The gut is more than an organ—it’s a sensory powerhouse, an emotional compass, and a partner in mental health. By tuning in to your body’s inner dialogue, you can uncover insights about your well-being that no scale or symptom chart can provide.
The gut-brain connection invites us to rethink the way we approach mental health. It encourages a holistic view, one that sees anxiety, depression, or cognitive fog not just as neurological imbalances, but as signs of systemic disharmony.
When we nourish the gut, we do more than improve digestion—we strengthen the foundation of resilience, clarity, and emotional vitality. In a world full of noise, your gut may be the quiet voice of wisdom you’ve been ignoring. Listen closely. It knows more than you think.