Imagine your body as a well-guarded castle. The walls are high, the gates are secure, and your loyal soldiers—your immune system—stand watch around the clock. Now, imagine that one section of the wall starts to crack. Tiny invaders sneak in through the fissures, and your soldiers, confused and alarmed, begin to attack everything in sight—both friend and foe. This is the basic idea behind a mysterious and controversial condition known as leaky gut syndrome.
For many people, the journey to discovering leaky gut starts with vague, frustrating symptoms: chronic bloating, fatigue that coffee can’t fix, stubborn weight gain, food sensitivities, unexplained inflammation, and even mental fog. Doctors may dismiss these as anxiety, IBS, or simply part of getting older. But more and more patients and health practitioners are discovering that the gut—specifically the permeability of the gut lining—may be at the heart of it all.
In this article, we’ll explore what leaky gut syndrome really is, how it develops, why it’s controversial in mainstream medicine, and how it might be the missing piece in understanding autoimmune disorders, mood swings, skin conditions, and much more.
The Gut: More Than a Digestion Machine
Before diving into leaky gut, it’s important to understand what the gut is and what it does—because it’s far more than just a food processor. Your gastrointestinal (GI) tract is a complex and highly intelligent system responsible for digestion, nutrient absorption, immune function, and even mental health.
In fact, about 70-80% of your immune system resides in your gut. The gut is lined with a single layer of specialized cells called enterocytes, forming a thin but crucial barrier between the outside world (everything you eat and drink) and your inner bloodstream. These cells are tightly connected by structures known as tight junctions, which regulate what gets absorbed into your body and what gets kept out.
Your gut is also home to trillions of microorganisms, collectively known as the gut microbiome. These microbes are essential partners in your health—they digest fiber, synthesize vitamins, regulate hormones, and help educate your immune system about what to fight and what to tolerate.
When everything is working properly, this barrier system and its microbial allies keep you healthy. But when it fails—when the tight junctions loosen and the lining becomes too permeable—things can go wrong fast.
Leaky Gut: Cracks in the Armor
Leaky gut syndrome, more formally referred to as increased intestinal permeability, occurs when the lining of the small intestine becomes compromised. Instead of selectively allowing only nutrients and beneficial molecules to pass through, the gut wall becomes porous, allowing bacteria, toxins, partially digested food particles, and waste products to “leak” into the bloodstream.
This triggers an immune response, as the body sees these invaders as foreign threats. The result? Chronic inflammation. This systemic, low-grade inflammation is believed to be a root cause of a wide array of health issues—from digestive complaints to autoimmune diseases to neurological symptoms.
Symptoms commonly associated with leaky gut include:
- Chronic bloating, gas, and indigestion
- Food sensitivities or intolerances
- Fatigue, even after a full night’s sleep
- Brain fog, memory lapses, and difficulty concentrating
- Skin problems such as eczema, acne, or rosacea
- Joint pain and stiffness
- Autoimmune conditions like Hashimoto’s thyroiditis, rheumatoid arthritis, or lupus
- Mood disorders, including depression and anxiety
Leaky gut doesn’t just affect digestion—it may affect your entire body.
What Causes the Gut to Leak?
So how does this crucial intestinal barrier become compromised? There isn’t just one culprit—leaky gut is more of a domino effect, a complex interplay between diet, lifestyle, stress, and microbiome imbalances.
Processed Foods and Sugar
Highly processed foods, refined sugar, and artificial additives are top offenders. Sugar feeds harmful bacteria and yeast in the gut, leading to microbial imbalances (a state called dysbiosis). Many processed foods also contain preservatives, emulsifiers, and synthetic compounds that irritate the intestinal lining, increasing permeability.
Gluten and Zonulin
In susceptible individuals, gluten—a protein found in wheat, barley, and rye—can trigger the release of zonulin, a molecule that regulates the tight junctions between cells in the gut. When zonulin levels rise, those tight junctions loosen, allowing unwanted substances to escape into the bloodstream.
Although not everyone is sensitive to gluten, those with celiac disease or gluten intolerance may experience severe intestinal permeability as a result of gluten exposure.
Chronic Stress
Stress doesn’t just affect your mind—it has a profound effect on your gut. Chronic psychological stress has been shown to alter the gut barrier, impair digestive function, and disrupt microbial balance. It also lowers immunity, making it easier for pathogens to take hold.
Antibiotics and Medications
While antibiotics can be lifesaving, they also kill off beneficial gut bacteria, potentially leading to dysbiosis. Other medications—like NSAIDs (ibuprofen), steroids, and acid blockers—can irritate the gut lining or alter the microbial environment, increasing the risk of leaky gut over time.
Alcohol and Toxins
Excessive alcohol is a well-known irritant to the gut lining. It inflames the intestines, disrupts tight junctions, and compromises the gut’s ability to repair itself. Environmental toxins—like pesticides, heavy metals, and pollutants—can also contribute to gut barrier dysfunction.
The Immune System Goes Rogue
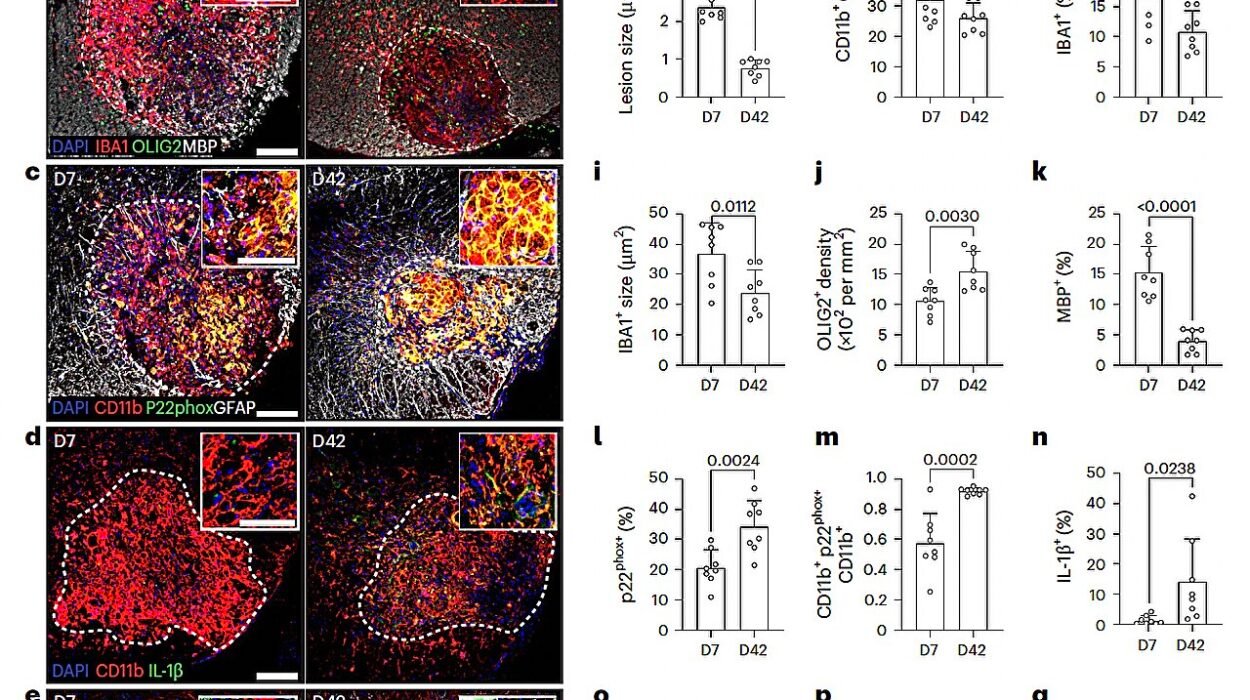
Once the gut becomes permeable, substances that would normally be confined to the digestive tract—like proteins from food or toxins from bacteria—enter the bloodstream. This triggers an immune alarm. Antibodies are produced. Inflammatory chemicals are released. White blood cells are dispatched to fight the intruders.
But when this happens chronically, the immune system becomes confused. It may begin attacking not just foreign invaders but the body’s own tissues. This is how leaky gut is believed to contribute to autoimmune disease. The immune system’s cross-reactivity may mistake thyroid proteins, joint tissues, or nerve fibers for the invaders that originally leaked through the gut.
Researchers have found associations between intestinal permeability and several autoimmune conditions, including:
- Hashimoto’s thyroiditis
- Multiple sclerosis
- Type 1 diabetes
- Psoriasis
- Inflammatory bowel disease (Crohn’s and ulcerative colitis)
Though more research is needed, the theory is gaining traction: to fix the immune system, you may need to start by fixing the gut.
The Gut-Brain Connection
Leaky gut doesn’t just trigger inflammation in the body—it may affect your brain as well. This happens through the gut-brain axis, the complex communication network linking the digestive system and the central nervous system.
When the gut leaks, inflammatory cytokines are released. These inflammatory molecules can cross the blood-brain barrier and affect neurotransmitter balance, potentially contributing to:
- Brain fog
- Depression
- Anxiety
- Memory problems
- Poor focus and ADHD symptoms
Additionally, gut microbes produce many of the same neurochemicals used by the brain—including serotonin, dopamine, and GABA. When the microbiome is out of balance, so is your mood.
For people who’ve tried antidepressants or stimulants without success, healing the gut may offer surprising mental health benefits.
Diagnosis: Why It’s So Hard to Detect
Here’s where things get tricky. Despite growing evidence, many conventional doctors remain skeptical of leaky gut syndrome. It isn’t an officially recognized medical diagnosis, and standard testing methods are limited.
However, functional medicine practitioners often use tests such as:
- Lactulose/mannitol urine test: Measures the absorption of sugar molecules to assess permeability
- Zonulin blood test: Looks for elevated zonulin levels, which may indicate loosened tight junctions
- Stool analysis: Identifies microbial imbalances, inflammation, or pathogenic overgrowth
- Food sensitivity panels: May reveal an overactive immune response to common foods
That said, many cases are diagnosed based on symptoms and patient history. While more rigorous research is still needed, the growing interest in gut health is pushing medicine to look deeper.
Healing a Leaky Gut: A Whole-Body Approach
Healing the gut is not about a single pill or protocol. It’s a holistic process involving diet, lifestyle, stress management, and targeted supplementation. Here’s how many health experts recommend addressing it:
Remove Irritants
The first step is eliminating foods and substances that may be irritating your gut. This often includes:
- Gluten
- Dairy
- Refined sugar
- Alcohol
- Artificial additives
- Processed foods
Some people also remove soy, corn, or nightshades temporarily to see if symptoms improve.
Rebuild with Nutrient-Dense Foods
Once irritants are removed, the focus shifts to nourishing and repairing the gut lining. Helpful foods include:
- Bone broth (rich in collagen and glutamine)
- Omega-3 fatty acids (found in wild fish, flaxseed, walnuts)
- Fermented foods (like sauerkraut, kefir, kimchi)
- Cooked vegetables and fiber-rich plant foods
- Herbs like turmeric and ginger
Support the Microbiome
Repopulating the gut with beneficial bacteria is crucial. Probiotics—either through supplements or fermented foods—can help restore balance. Prebiotics (fibers that feed good bacteria) are also important and can be found in onions, garlic, asparagus, and bananas.
Repair the Gut Lining
Certain nutrients and supplements have been shown to help seal and support the gut barrier:
- L-glutamine (an amino acid that helps repair intestinal cells)
- Zinc carnosine
- Quercetin
- Slippery elm, marshmallow root, and licorice root (herbal mucilaginous compounds)
- Vitamin D and omega-3s (to modulate inflammation)
Manage Stress
Chronic stress is a major contributor to leaky gut, so managing stress is essential. This may involve:
- Mindfulness meditation
- Yoga or tai chi
- Therapy or journaling
- Getting regular sleep
- Spending time in nature
Controversy: Why Doctors Don’t Always Agree
Despite the compelling theories and anecdotal evidence, leaky gut remains controversial. Critics argue that increased intestinal permeability may be a symptom, not a cause, of chronic illness. Others say more clinical trials are needed to prove causation.
Part of the problem is that leaky gut sits at the crossroads of multiple systems—digestive, immune, neurological—and doesn’t fit neatly into any one specialty. It’s a messy, multifactorial condition that challenges the reductionist model of Western medicine.
Yet, patient experiences continue to drive interest. As more people seek root-cause solutions rather than symptom suppression, leaky gut is becoming a hot topic not only in functional and integrative medicine but also in research labs.
Conclusion: A Revolution in Understanding Health
Leaky gut syndrome is more than just a buzzword—it’s a paradigm shift in how we understand health. It forces us to see the body as an interconnected web, where what happens in your gut doesn’t stay in your gut. From skin to mood, immunity to metabolism, the gut is ground zero for overall well-being.
If you’re dealing with unexplained symptoms, autoimmune flares, or mood swings that seem to have no medical explanation, the answer might lie in your gut. Healing the gut is not just about digestion—it’s about restoring harmony to the entire body.
And while the science continues to evolve, one thing is clear: the path to better health almost always begins in the gut.