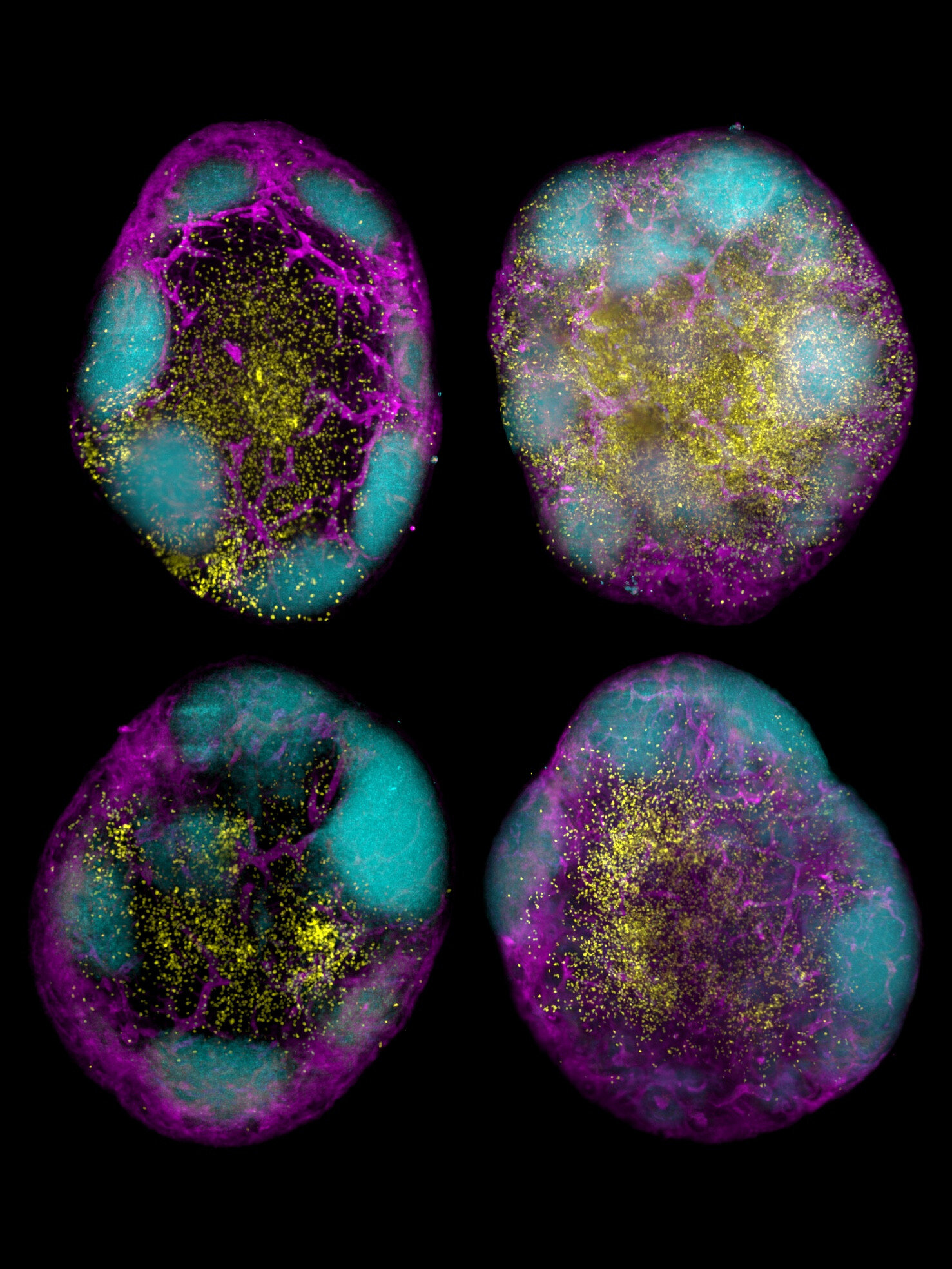
In a transformative leap for immunology and vaccine science, researchers at Melbourne’s Walter and Eliza Hall Institute of Medical Research (WEHI) have unveiled a groundbreaking approach that could redefine how we protect against infectious diseases and even treat cancer. Published in the Journal of Experimental Medicine, the WEHI-led study offers a tantalizing glimpse into the future of long-lasting, booster-free vaccines—and it all centers on a rare and powerful type of immune cell: stem cell-like memory CD8+ T cells.
These remarkable cells have long intrigued scientists for their enduring memory and resilience. But now, with the aid of cutting-edge mRNA vaccine technology and strategic immunomodulation, WEHI scientists have found a way to supercharge their formation, paving the way for more durable vaccines and potentially revolutionary cancer immunotherapies.
The Achilles’ Heel of Traditional Vaccines
Vaccines are humanity’s most potent shield against infectious diseases, responsible for saving countless lives each year. Yet, even the most effective vaccines come with limitations. The majority rely heavily on the body’s antibody response—proteins that identify and neutralize pathogens. While powerful, antibodies have a flaw: they fade over time. This waning immunity is the reason we routinely receive booster shots, from seasonal flu jabs to the more recent COVID-19 vaccine updates.
The problem intensifies with viruses that mutate rapidly. As viral surfaces evolve, the antibodies tailored to previous strains lose effectiveness. This dynamic has driven a ceaseless cycle of booster vaccinations, a model both cumbersome and unsustainable in the face of future pandemics.
But what if a vaccine could create an immune response so robust, so long-lasting, that boosters became obsolete? What if, instead of fading within months, immunity endured for years—or even decades?
The Power of Memory: CD8+ T Cells Take Center Stage
The answer may lie within a lesser-known yet extraordinary immune warrior: the CD8+ T cell. More specifically, a subtype known as stem cell-like memory CD8+ T cells.
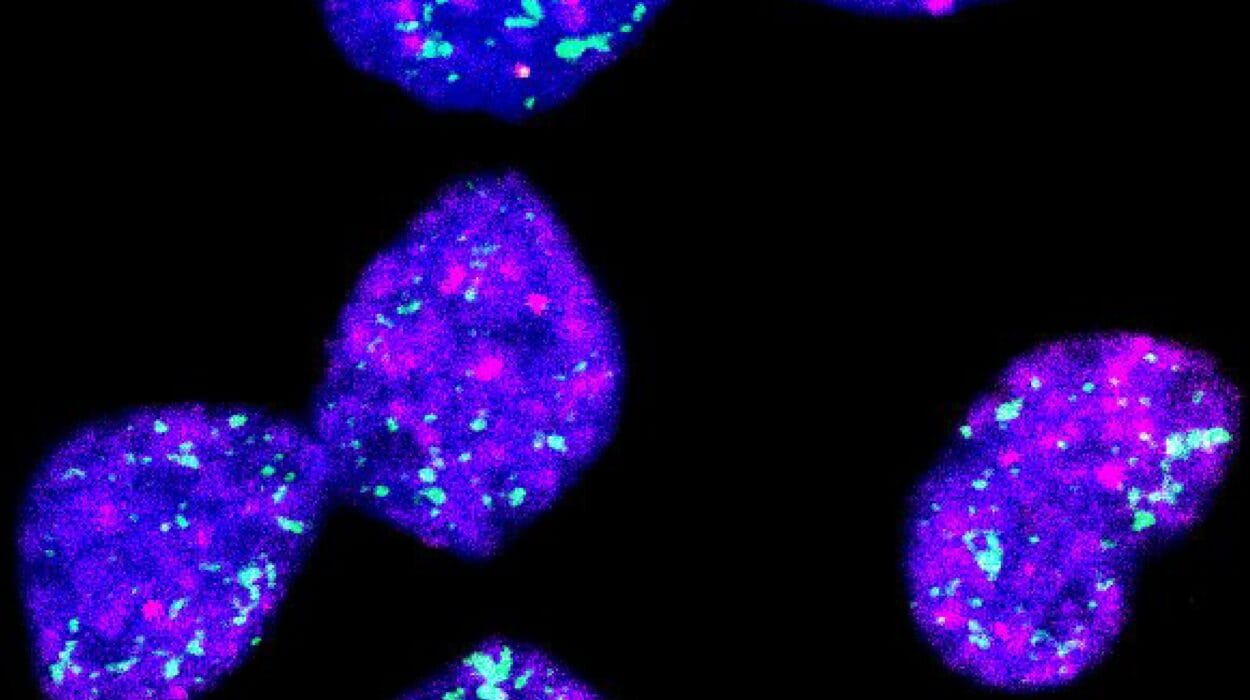
Unlike antibodies, which float in the bloodstream scanning for familiar pathogens, CD8+ T cells seek and destroy infected or abnormal cells. They are the immune system’s elite assassins. Within this population, the stem cell-like memory subset acts as a long-lived reservoir, capable of both self-renewal and rapid deployment when danger arises. These are the memory banks of the immune system—durable, adaptable, and incredibly efficient.
Associate Professor Joanna Groom, head of WEHI’s Immunology Division and lead author of the study, explained the magnitude of this discovery: “We’ve believed for some time that stem cell-like memory CD8+ T cells correlate with long-lasting protection, and this study is the first to prove this benefit.”
These cells, she elaborated, function much like the memory of an elephant—retaining a record of past infections and leaping into action when similar threats appear again. The challenge, until now, has been coaxing the immune system to produce them in meaningful quantities.
Engineering Super Immunity with mRNA and Immunomodulation
The WEHI study overcame this hurdle using a two-pronged strategy: immunomodulation and mRNA vaccine technology.
First, immunomodulation techniques were employed to steer the immune response toward the desired cell type. Rather than indiscriminately amplifying immune reactions, this approach fine-tunes the system—essentially reprogramming it to favor the production of stem cell-like memory CD8+ T cells.
Second, researchers utilized the adaptable power of mRNA vaccines. Unlike traditional vaccines, which use weakened pathogens or protein fragments, mRNA vaccines deliver genetic instructions that prompt cells to produce a specific protein—triggering a tailored immune response. This method, proven effective during the COVID-19 pandemic, is not only faster to develop but also highly customizable.
“When we combined these two approaches, the results were really striking,” said Associate Professor Groom. “We were incredibly excited at how effective our new vaccine strategy was at boosting these cells.”
Toward a New Era of Durable Vaccines
The implications of the WEHI team’s findings are immense. For infectious diseases, this strategy could signal the end of frequent boosters. A single dose of a vaccine designed to stimulate stem cell-like memory CD8+ T cells could offer protection that lasts decades. That’s a game-changer for global health.
Moreover, by creating a reservoir of immune cells that remain alert and ready to attack, vaccines could become more effective against viruses that currently evade long-term immunity—such as HIV, hepatitis C, and rapidly mutating strains of influenza or coronavirus.
“The goal is not just to prevent infection temporarily, but to create a lasting immune army,” said Groom. “Inducing these cells is the next big challenge for improving vaccines, and we’re energized to bring this future closer.”
Cancer Immunotherapy: A Bold New Application
While the study’s implications for infectious disease are revolutionary, its potential impact on cancer treatment may be even more profound.
Stem cell-like memory CD8+ T cells are not just guardians against viruses—they’re also potent anti-cancer agents. These cells are capable of recognizing and destroying cancerous cells that the body’s immune system might otherwise overlook or tolerate.
PhD student Benjamin Broomfield, the study’s first author, sees a bright future for this line of research: “We know the body needs these cells to eliminate cancerous cells, and our lab is now focused on applying the approach used in this study to boost stem cell-like CD8+ T cells to tackle cancer.”
This opens the door to therapeutic cancer vaccines—customized immunizations that train the body to hunt down and destroy cancer cells before they can proliferate. Unlike traditional treatments like chemotherapy or radiation, which often damage healthy cells and carry severe side effects, a vaccine-based approach would work with the body’s own defenses, offering a more precise and less invasive alternative.
“A therapeutic vaccine for cancer would be a total game-changer,” said Broomfield. “And we’re optimistic about where this research can go.”
mRNA Technology: The Vaccine Platform of the Future
Central to this breakthrough is the mRNA platform. Once a niche concept, mRNA vaccines became household terms during the COVID-19 pandemic. Now, they are emerging as the most versatile and responsive tool in the global immunization toolkit.
The beauty of mRNA lies in its speed and adaptability. Within weeks, a vaccine can be developed, manufactured, and deployed to target a newly emerged pathogen. Unlike conventional vaccines that may take years to produce, mRNA vaccines can be altered quickly to meet the demands of evolving threats—whether viral, bacterial, or cancerous.
The WEHI team’s success in using mRNA technology to trigger a durable T cell response adds another layer to its promise. No longer limited to antibody stimulation, mRNA vaccines can now be designed to orchestrate a more robust and lasting cellular immunity—a development that dramatically widens their therapeutic horizon.
The Road Ahead: From Mouse Models to Human Trials
While the results from the mouse models are incredibly promising, translating them into human applications will require rigorous testing. The next steps involve refining the formulation, optimizing dosage, and conducting clinical trials to confirm the safety and efficacy of the approach in people.
But the foundation has been laid. The discovery represents not just an incremental advance, but a seismic shift in how scientists think about vaccines.
Instead of building temporary shields, we can now envision constructing enduring immune fortresses—armies of vigilant, self-renewing cells standing guard for decades.
A Global Impact: Rethinking Immunization Strategies
Imagine a world where one vaccine in childhood grants lifelong protection against measles, or where a single immunization at the onset of adulthood prevents cervical cancer, HIV, or future pandemics. Such a paradigm shift would revolutionize public health logistics, reduce healthcare costs, and extend vaccine equity across low-income regions where access to boosters is limited.
For cancer patients, this strategy could offer a gentler yet more potent tool to complement or even replace traditional treatments. For the aging population, whose immune systems often weaken over time, the induction of long-lasting memory T cells could provide a new lease on life.
Conclusion: A Vaccine Revolution on the Horizon
WEHI’s pioneering work has unveiled a new chapter in the story of immunology—one where long-term immunity is no longer a dream, but a plausible reality. By harnessing the stem cell-like memory CD8+ T cells and leveraging the power of mRNA technology, scientists are pushing the boundaries of what vaccines can achieve.
This is more than a scientific breakthrough—it is the dawn of super vaccines, a future where humanity is better armed not just against known foes, but against the pandemics and cancers yet to emerge.
In the words of Associate Professor Groom, “We’re energized to bring this future closer.” And so is the world.
Reference: Benjamin J. Broomfield et al, Transient inhibition of type I interferon enhances CD8+ T cell stemness and vaccine protection, Journal of Experimental Medicine (2025). DOI: 10.1084/jem.20241148