From the moment we are born, the very first thing we do is breathe. That first gasp of air signifies life, and each breath thereafter carries oxygen to our cells and fuels every biological process in our body. Breathing is automatic—effortless, most of the time—yet intricately complex. We take it for granted until something disrupts it. When that disruption is caused by asthma or other breathing disorders, the simplicity of breath becomes a struggle for survival.
Breathing disorders are among the most common medical conditions worldwide, affecting people of all ages and backgrounds. Of these, asthma stands as both one of the most prevalent and the most enigmatic. Despite decades of research, its full nature remains elusive. What causes the wheeze? Why does the air feel thick and tight? Why are some people more vulnerable than others?
To truly grasp asthma and breathing disorders, we must journey deep into the lungs—into the airways, immune system, genetics, and even the emotions that can trigger or ease a breath. This article unravels the science of respiration and explores the fragile dance between air and life.
The Respiratory System: A Biological Symphony
Breathing begins in the nose or mouth, where air enters the body, travels down the throat (pharynx), passes the voice box (larynx), and descends through the trachea. The trachea splits into two bronchi, each leading to a lung. Within the lungs, the bronchi divide into smaller bronchioles, ending in alveoli—tiny air sacs surrounded by capillaries. Here, oxygen enters the blood and carbon dioxide exits.
The lungs are marvels of biology. A healthy adult has about 300 million alveoli, offering a surface area roughly the size of a tennis court. Every minute, your lungs move about six liters of air, and your heart pumps that oxygenated blood to every organ.
But this process doesn’t happen in isolation. The brainstem monitors carbon dioxide levels and sends signals to breathe more or less. Muscles like the diaphragm and intercostals contract and expand the chest cavity. It’s a seamless, choreographed performance—until something goes wrong.
What Is Asthma?
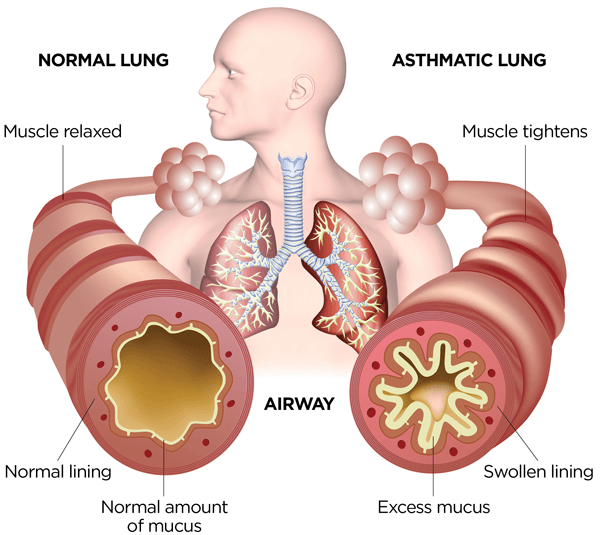
Asthma is a chronic inflammatory disease of the airways. In an asthmatic person, the bronchial tubes are hypersensitive and prone to narrowing in response to certain triggers. This leads to a set of classic symptoms: wheezing, coughing (especially at night or early morning), shortness of breath, and chest tightness.
Unlike acute respiratory infections, asthma is not caused by a pathogen but by a complex interaction of genetic, environmental, and immunological factors. It is episodic—meaning it can flare up unexpectedly—but it is also chronic, requiring long-term management.
Asthma can be mild and barely noticeable or severe and life-threatening. Globally, it affects over 300 million people, and while treatments exist, there is no definitive cure.
To understand why asthma happens, we need to look deeper at how the immune system interacts with the lungs.
The Immune System and Inflammation: The Double-Edged Sword
In asthma, the immune system becomes an overzealous guardian. Normally, immune cells patrol the lungs and respond only when pathogens are present. In an asthmatic lung, however, the immune system sees threats everywhere—dust mites, pollen, cold air, even exercise—and overreacts.
The key players in this immune misfire are:
- Mast cells, which release histamines and other chemicals that cause inflammation.
- Eosinophils, white blood cells that exacerbate tissue swelling and damage.
- T-helper cells (especially Th2), which coordinate the immune response and are more active in allergic types of asthma.
When a trigger is inhaled, these cells activate and set off a cascade of responses: blood vessels dilate, airway walls swell, mucus production increases, and smooth muscles around the airways tighten. The result? Narrowed bronchial tubes that resist airflow.
This inflammation is not just a temporary event. In chronic asthma, the airways can undergo remodeling: the walls thicken, the smooth muscle layers grow, and the lungs become more prone to future attacks.
Ironically, the immune system, which is designed to protect, becomes the very source of harm.
Triggers: The Enemies of the Breath
Asthma is often said to be “triggered”—a word that suggests a sudden explosion. Triggers are environmental or behavioral factors that provoke symptoms. They differ from person to person, but common culprits include:
- Allergens: pollen, dust mites, pet dander, mold.
- Irritants: cigarette smoke, air pollution, chemical fumes.
- Infections: viral colds and flu are frequent triggers.
- Physical exertion: exercise-induced asthma affects many athletes.
- Weather: cold air, dry wind, sudden changes in temperature.
- Emotions: stress, anxiety, and even laughter can induce attacks in sensitive individuals.
The unpredictability of these triggers adds to the psychological burden of asthma. Imagine feeling breathless every time the seasons change or someone lights a cigarette nearby. This ever-present risk influences behavior, choices, and lifestyle.
Types of Asthma: A Diverse Disease
Not all asthma is the same. Clinically, asthma is categorized into different phenotypes—subtypes with distinct causes and manifestations.
Allergic (extrinsic) asthma is most common in children and linked to other allergic conditions like eczema or hay fever. It’s driven by immunoglobulin E (IgE) responses to specific allergens.
Non-allergic (intrinsic) asthma usually appears later in life and isn’t tied to identifiable allergens. It’s often harder to treat and may be more severe.
Exercise-induced asthma manifests during or after physical activity, especially in cold or dry environments.
Occupational asthma results from exposure to irritants in the workplace—such as flour in bakers or chemicals in factory workers.
Aspirin-exacerbated respiratory disease (AERD) occurs in individuals sensitive to nonsteroidal anti-inflammatory drugs (NSAIDs) and often coexists with nasal polyps.
Each form requires tailored treatment, and emerging research into asthma phenotyping aims to customize therapy to the individual.
Asthma in Children vs. Adults
Asthma doesn’t play by a single rulebook when it comes to age.
In children, asthma is often linked to allergies and is sometimes outgrown after puberty. But it can also be severe and persistent, especially when combined with environmental exposures like secondhand smoke or poor air quality.
In adults, asthma can be new-onset or a continuation from childhood. Hormonal changes, occupational factors, and chronic inflammation often contribute. Adult-onset asthma is frequently less responsive to standard treatments and may progress more quickly.
One of the tragedies of pediatric asthma is its impact on growth, school attendance, and even mental health. For adults, the concern is often on managing long-term health, preventing complications like chronic obstructive pulmonary disease (COPD), and maintaining quality of life.
Other Breathing Disorders
While asthma takes the spotlight, it’s part of a broader family of respiratory diseases that affect millions:
Chronic Obstructive Pulmonary Disease (COPD)
COPD, which includes chronic bronchitis and emphysema, is a progressive disease usually caused by long-term smoking. Unlike asthma, its damage is often irreversible, and symptoms steadily worsen over time. Patients experience chronic cough, sputum production, and increasing shortness of breath.
Cystic Fibrosis
A genetic disorder caused by mutations in the CFTR gene, cystic fibrosis leads to thick, sticky mucus in the lungs and digestive tract. This results in frequent infections, lung damage, and reduced life expectancy. Advances in gene therapy are offering new hope for CF patients.
Pulmonary Fibrosis
This disorder involves scarring of lung tissue, making it stiff and unable to expand properly. Causes range from environmental exposures to unknown origins. It’s a serious condition with limited treatment options, though antifibrotic drugs can slow progression.
Sleep Apnea
A breathing disorder during sleep, where airflow is intermittently blocked. It results in fragmented sleep, fatigue, and increased cardiovascular risk. CPAP machines (Continuous Positive Airway Pressure) are a standard treatment.
Bronchiectasis
Often a complication of repeated infections or autoimmune diseases, bronchiectasis involves permanent widening and damage to the bronchi, leading to mucus buildup and chronic infection.
Each of these disorders impacts the same respiratory system but in different ways. Diagnosis and treatment rely heavily on imaging, lung function tests, and understanding the patient’s history.
Diagnosing Asthma: Not Just a Stethoscope and Guesswork
Asthma diagnosis isn’t always straightforward. Doctors combine patient history, physical examination, and objective testing. Common tools include:
- Spirometry: Measures how much air you can inhale and exhale, and how quickly. It’s essential in detecting airflow limitation.
- Peak Expiratory Flow (PEF): A portable tool that measures the fastest speed you can blow air out of your lungs. Useful for home monitoring.
- Bronchodilator response: Improvement in lung function after using a bronchodilator confirms reversible airway obstruction.
- Methacholine challenge test: Used when asthma is suspected but not confirmed. Methacholine triggers mild airway narrowing in sensitive individuals.
- Allergy testing: Identifies specific allergens that may be contributing.
Asthma is a diagnosis that demands both science and intuition—especially since its symptoms often mimic other conditions.
Treatment: Controlling the Fire Within
Asthma cannot be cured, but it can be controlled. The goals of treatment are to reduce symptoms, prevent flare-ups, and improve quality of life.
The cornerstone of asthma treatment is a two-pronged approach:
- Controller medications: Taken daily to reduce inflammation and prevent symptoms. The most common are inhaled corticosteroids, sometimes combined with long-acting beta-agonists (LABAs).
- Rescue medications: Fast-acting drugs like short-acting beta-agonists (SABAs) (e.g., albuterol) used during acute attacks to relieve symptoms quickly.
In severe cases, other treatments include:
- Leukotriene modifiers (e.g., montelukast) which block inflammatory chemicals.
- Biologics like omalizumab or mepolizumab that target specific immune pathways.
- Oral corticosteroids for severe flare-ups (though long-term use is avoided due to side effects).
- Bronchial thermoplasty, a procedure that uses heat to reduce smooth muscle in the airways.
Patient education is also critical—knowing how to use inhalers correctly, monitoring symptoms, and avoiding triggers are as important as the drugs themselves.
Living with Asthma: Beyond the Prescription
Asthma isn’t just a medical condition—it’s a life condition. It affects school, work, sports, relationships, and mental health.
Some patients avoid exercise out of fear, while others suffer sleep disruption due to nighttime symptoms. Anxiety is common, especially after experiencing a severe attack.
Yet, with proper management, most people with asthma can live full, active lives. Athletes with asthma have competed—and won—at the Olympics. Children with asthma grow up to become doctors, scientists, and even astronauts.
Support systems, access to healthcare, environmental justice (clean air), and patient advocacy play powerful roles in the asthma journey.
Breathing Disorders and the Mind-Body Connection
Breathing is one of the few bodily functions controlled both voluntarily and involuntarily. This makes it a bridge between mind and body.
Stress, anxiety, and depression can worsen asthma symptoms. Conversely, breath control practices—like yoga, meditation, and diaphragmatic breathing—can improve lung function and reduce attacks.
Understanding the psychosocial dimension of asthma opens new avenues of healing. It’s not just about inhalers—it’s about empowerment, resilience, and mindfulness.
The Future of Respiratory Medicine
Exciting developments are shaping the future of asthma and breathing disorder management:
- Precision medicine aims to tailor treatments based on genetic and molecular profiles.
- Wearable devices track lung function and alert users to changes.
- Smart inhalers log usage and send data to healthcare providers.
- AI algorithms help diagnose and predict attacks using big data.
- Gene editing may one day offer cures for conditions like cystic fibrosis.
Our growing understanding of respiratory biology, combined with technological advances, promises a future where no one has to suffer silently with shortness of breath.
Conclusion: A Deeper Breath
Asthma and other breathing disorders remind us how fragile, and how vital, the simple act of breathing is. These conditions are complex, multifaceted, and deeply personal—but they are also manageable, and in some cases, preventable.
Understanding the science behind these diseases empowers patients, families, and healthcare professionals to act wisely. It turns fear into knowledge, suffering into strategy, and gasps into full, confident breaths.
In the end, every breath matters—not just as a function of life, but as a testament to how science, compassion, and human will come together to overcome adversity.