Every second of every day, unseen forces move among us, through us, and sometimes against us. These tiny agents—bacteria and viruses—are so small they’re invisible to the naked eye, yet they have shaped human history more profoundly than any war, invention, or political movement. From the Black Death to the COVID-19 pandemic, infections have toppled empires, rewritten laws, and transformed societies.
But what exactly are these microscopic menaces? How do they spread from person to person, animal to animal, or even from surfaces to skin? What tricks do they use to bypass our defenses, and how does the human body respond? Understanding how infections spread is not just a matter of curiosity—it’s key to surviving in a world teeming with microbial life.
This article explores the complex, fascinating mechanisms by which infections spread, delving deep into the worlds of bacteria and viruses, their strategies, their evolution, and the medical science fighting to keep them at bay.
Bacteria and Viruses: Know Thy Enemy
To truly grasp how infections spread, we must first understand what’s doing the spreading. Bacteria and viruses are not the same—they’re fundamentally different in structure, behavior, and biological function.
Bacteria are single-celled organisms. Some are shaped like spheres (cocci), rods (bacilli), or spirals (spirilla). They can live in a wide range of environments—from ocean vents to the intestines of mammals. Many bacteria are harmless or even helpful, forming part of the natural flora of the skin and gut. Others, however, are pathogenic, meaning they can cause disease. Think Streptococcus (strep throat), Mycobacterium tuberculosis (TB), or Escherichia coli (E. coli).
Viruses, on the other hand, are not even technically alive by many definitions. They are packets of genetic material—either DNA or RNA—wrapped in a protein coat. Unlike bacteria, viruses cannot replicate on their own. They must hijack a host cell’s machinery to make more copies of themselves. Examples include influenza, HIV, measles, and SARS-CoV-2.
Their strategies differ, but their goal is the same: reproduction and survival.
The Reservoir: Where Infection Begins
All infections begin somewhere. In the world of medicine and microbiology, that starting point is called the reservoir. This is the natural habitat where a pathogen lives, grows, and multiplies.
Reservoirs can be human, animal, or environmental:
- A human reservoir means the pathogen lives primarily in people. This is common for viruses like measles, HIV, and hepatitis B.
- An animal reservoir means the infection cycles through animals before occasionally jumping to humans—this is known as a zoonotic infection. Rabies, Ebola, and many strains of influenza fall into this category.
- Environmental reservoirs are places like soil, water, or surfaces. Clostridium tetani (causing tetanus) lives in soil, while Legionella can live in water systems.
Some infections have more than one type of reservoir. For instance, cholera involves water and humans. Understanding the reservoir is crucial to controlling the spread.
Modes of Transmission: How Pathogens Travel
Once a pathogen exits its reservoir, it must find a new host. This journey is known as transmission, and it happens through several well-studied pathways.
Direct Contact Transmission
This is perhaps the most straightforward method. When one person touches another—through skin, mucous membranes, or bodily fluids—pathogens can pass directly from one body to another. Sexually transmitted infections like syphilis, herpes, and HIV primarily use this mode. Skin infections such as impetigo or ringworm can also spread this way.
Indirect Contact Transmission
In this route, the pathogen travels via an intermediary—called a fomite—such as a doorknob, phone screen, or towel. If an infected person touches an object, and someone else then touches it and their face or wound, transmission can occur. This is common for cold and flu viruses, norovirus, and MRSA.
Droplet Transmission
Sneezing, coughing, or even talking can release respiratory droplets loaded with viral or bacterial particles. These droplets can travel several feet and land in the eyes, nose, or mouth of a nearby person. Influenza, pertussis (whooping cough), and COVID-19 often spread this way.
Airborne Transmission
Smaller than droplets are aerosols—tiny particles that can remain suspended in the air for hours and travel farther. Measles and tuberculosis are classic airborne diseases. These are much harder to control because physical distance may not be enough.
Vector-Borne Transmission
Some pathogens hitch rides on other organisms known as vectors. Mosquitoes transmit malaria and dengue, ticks carry Lyme disease, and fleas helped spread the plague. Vector control—like bed nets or insect repellents—is essential in managing these diseases.
Food and Waterborne Transmission
Pathogens can contaminate what we eat or drink. Infections like cholera, typhoid, E. coli, and hepatitis A are often spread through fecal contamination of food or water. Safe food handling and sanitation are crucial preventive measures.
Incubation and Latency: The Silent Phase
One of the most dangerous aspects of infection is what happens before symptoms appear.
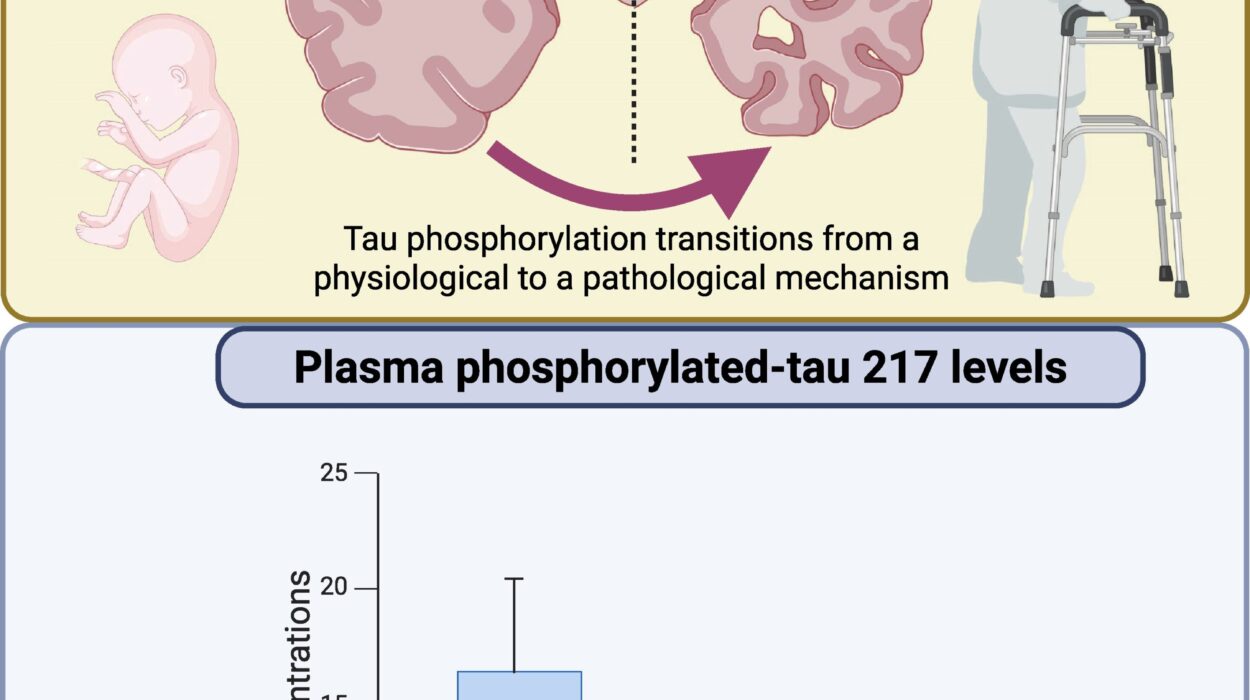
The incubation period is the time between exposure and the onset of symptoms. It can be hours (as in food poisoning), days (influenza), or even years (HIV). During this time, the infected person might not feel sick but can still be contagious.
Some pathogens also go into a latent phase, where they remain dormant inside the body and reactivate later. Herpes viruses are famous for this. After the initial infection, the virus hides in nerve cells and can reemerge during times of stress or immune suppression.
These silent phases make containment and diagnosis much more difficult. A person can unknowingly spread the infection far and wide.
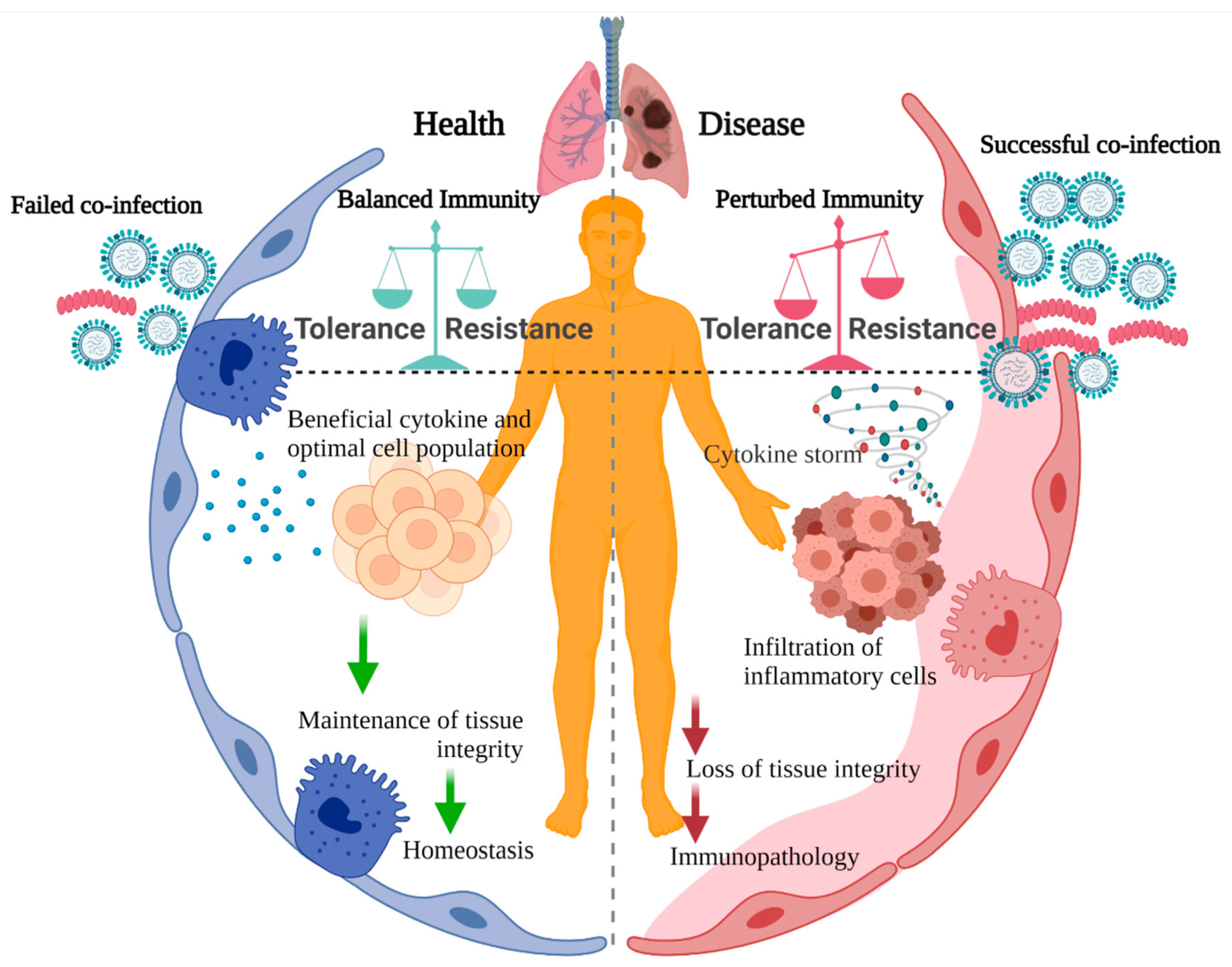
The Human Body’s Response: Immunity in Action
When a pathogen invades, the body doesn’t just sit idle—it fights back with an astonishing array of defenses.
The first line is the innate immune system: skin, mucous membranes, stomach acid, and white blood cells like neutrophils that attack anything foreign. If that fails, the adaptive immune system kicks in, mounting a targeted response with T cells and B cells, which produce antibodies.
Fever, inflammation, and fatigue aren’t just symptoms—they’re evidence of battle. The body raises its temperature to slow down bacterial growth, floods the infected area with white blood cells, and triggers rest to conserve energy.
Sometimes the immune response is so powerful that it becomes a problem itself. Cytokine storms, overreactions of the immune system, have been implicated in severe cases of influenza and COVID-19.
Antibiotics and Antivirals: The Medical Counterattack
When natural immunity isn’t enough, we turn to medicine. But the weapons we use differ for bacteria and viruses.
Antibiotics are powerful drugs designed to kill or inhibit bacteria. Penicillin, discovered in 1928, revolutionized medicine and saved millions of lives. Modern antibiotics target specific bacterial functions: cell wall synthesis, protein production, or DNA replication.
However, antibiotics do not work on viruses. Taking antibiotics for a viral infection not only won’t help—it can contribute to antibiotic resistance, a major global health crisis.
Antivirals, on the other hand, are much trickier. Because viruses use our own cells to replicate, it’s hard to kill the virus without harming the host. Antivirals like oseltamivir (for flu) or antiretrovirals (for HIV) work by interfering with viral entry, replication, or release.
Vaccines are another form of defense, training the immune system to recognize pathogens before real infection occurs. They’ve been enormously successful—eliminating smallpox, nearly eradicating polio, and saving millions annually from flu and measles.
Superbugs and Mutation: When Pathogens Fight Back
Unfortunately, bacteria and viruses don’t just sit still either. They evolve.
Bacteria develop resistance through mutation and horizontal gene transfer. One bacterium can pass resistance genes to another, even across species. That’s why MRSA (Methicillin-Resistant Staphylococcus aureus) and multi-drug resistant TB are so hard to treat.
Viruses mutate too. Influenza mutates so quickly that a new vaccine is needed every year. HIV mutates so fast that it’s nearly impossible to develop a one-size-fits-all cure. SARS-CoV-2 has demonstrated just how dangerous viral mutation can be, producing new variants that can spread faster or evade immunity.
Social Behavior and Infection Spread
Beyond biology, human behavior plays a huge role in how infections spread.
Urbanization, travel, and globalization have brought people into close contact, making it easier for diseases to hop continents. Air travel can move an infected person across the globe in less than a day.
Social habits—like handshakes, hugging, or communal eating—can enhance transmission. Hygiene practices, access to healthcare, and cultural beliefs all affect outcomes.
Infection control measures such as handwashing, wearing masks, isolating sick individuals, and widespread vaccination campaigns can drastically reduce the spread of disease.
Emerging Infections and the Role of Zoonoses
Over 60% of emerging infectious diseases are zoonotic—they originate in animals and jump to humans. This includes HIV (from chimpanzees), Ebola (likely from bats), and coronaviruses (from bats via intermediate hosts).
Deforestation, animal farming, wildlife trade, and climate change all increase human-animal interactions, raising the risk of future pandemics. As humans push deeper into wild ecosystems, the microbial world pushes back.
Preventing the Next Pandemic: A Holistic Approach
Understanding how infections spread is more important than ever. Preventing future pandemics will require a multidisciplinary approach:
- Surveillance systems to detect outbreaks early
- Rapid diagnostics and genome sequencing
- Investment in public health infrastructure
- Global cooperation and information sharing
- Responsible antibiotic use
- Research into new vaccines and treatments
Doctors, epidemiologists, environmental scientists, and even behavioral psychologists all have a role to play.
Conclusion: A Delicate Balance
Infections have always been with us—and they always will be. They’re a natural part of life on Earth, a consequence of living in a world filled with microscopic organisms that evolve as fast as we do, if not faster.
But knowledge is power. The more we understand about how bacteria and viruses spread, the better we can protect ourselves, our communities, and future generations. From the individual level—washing hands, covering coughs, getting vaccinated—to the global stage of pandemic preparedness, every action counts.
In the end, the story of infections is not just one of suffering and survival. It’s also one of discovery, resilience, and the incredible complexity of life. Because while pathogens are formidable foes, human ingenuity—and the human immune system—remain among the most powerful forces on Earth.