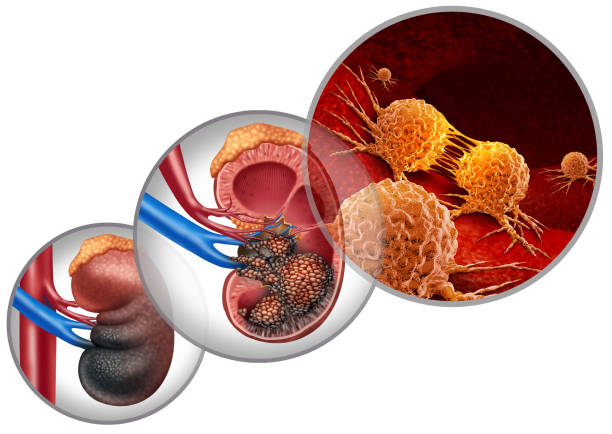
The kidneys are two bean-shaped organs nestled deep in the back of the abdomen, quietly working to filter blood, remove toxins, and balance the body’s fluids. They rarely call attention to themselves until something goes wrong. Kidney cancer, however, often grows in silence. In many cases, it is discovered unexpectedly—during a scan for an unrelated issue—because its earliest stages may not cause pain or obvious symptoms.
This hidden nature makes kidney cancer particularly daunting. It develops in one of the body’s most essential systems, often progressing quietly until it demands attention. But with advances in medical science, earlier detection, and effective treatments, survival rates have improved significantly in recent decades. Understanding the causes, symptoms, diagnosis, and treatment of kidney cancer is essential—not just for patients and families facing it, but for anyone seeking to better understand the human body and the illnesses that can affect it.
Understanding Kidney Cancer
Kidney cancer, also known as renal cell carcinoma (RCC) in its most common form, originates in the cells lining the tiny tubes within the kidneys. These tubes filter waste from blood, reabsorb nutrients, and regulate water balance. When the DNA in these cells mutates, they may begin to grow uncontrollably, forming a tumor.
There are several types of kidney cancer:
- Renal Cell Carcinoma (RCC): The most common type, accounting for about 90% of cases. Subtypes include clear cell RCC, papillary RCC, and chromophobe RCC.
- Transitional Cell Carcinoma: Begins in the renal pelvis, the part of the kidney where urine collects before moving to the bladder.
- Wilms’ Tumor: A rare type affecting mostly children.
- Renal Sarcoma: An uncommon cancer arising from the connective tissues of the kidney.
Each type behaves differently, but all share a potential to disrupt the delicate equilibrium the kidneys maintain.
Causes and Risk Factors
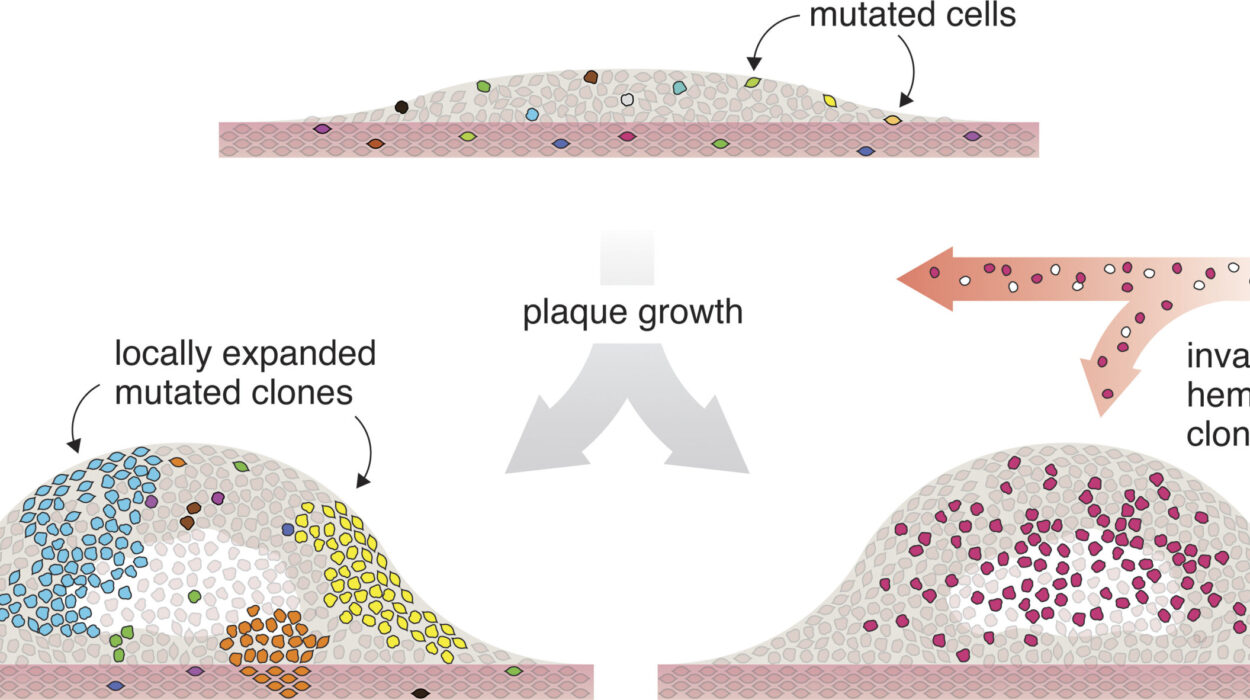
Cancer rarely has a single cause; it develops from a complex interaction of genetics, environment, and lifestyle. In kidney cancer, certain risk factors increase the likelihood of developing the disease.
Genetic Mutations and Inherited Conditions
Some cases of kidney cancer are linked to inherited genetic syndromes such as Von Hippel-Lindau disease, hereditary papillary renal carcinoma, or Birt-Hogg-Dubé syndrome. These syndromes increase susceptibility by causing mutations in specific genes that regulate cell growth.
But even in people without inherited conditions, spontaneous genetic mutations can arise. These alterations can silence tumor-suppressor genes or activate oncogenes, disrupting the normal cycle of cell death and regeneration.
Lifestyle and Environmental Risks
Smoking is one of the most significant lifestyle-related risk factors, doubling the risk of kidney cancer. Carcinogens in cigarette smoke are filtered by the kidneys and can damage renal cells over time.
Obesity also plays a critical role. Excess body fat disrupts hormone balance and promotes chronic inflammation, both of which can drive abnormal cell growth. Hypertension (high blood pressure), whether from obesity or other causes, has also been strongly linked to kidney cancer.
Certain occupational exposures—such as prolonged contact with industrial chemicals, asbestos, cadmium, or some herbicides—can further elevate risk.
Age, Gender, and Other Factors
Kidney cancer is most often diagnosed in people over 60, though it can occur earlier. Men are almost twice as likely as women to develop it, a difference partially explained by higher rates of smoking and occupational exposures historically among men. Family history of kidney cancer also increases risk, although most cases occur sporadically.
Symptoms: When the Body Sends Signals
One of the reasons kidney cancer can be challenging is that it often develops without early symptoms. By the time signs emerge, the tumor may already be relatively large or spreading. Still, there are key symptoms to recognize:
- Blood in the urine (hematuria): This is one of the most common warning signs. The urine may appear pink, red, or cola-colored, even if blood is present only intermittently.
- Persistent pain in the side or back: Often dull and unrelenting, this pain occurs where the kidneys are located.
- A lump or mass in the abdomen: Sometimes detected during a physical exam or imaging test.
- Unexplained weight loss: Cancer often disrupts metabolism and appetite.
- Fatigue and weakness: A general feeling of being drained, even with adequate rest.
- Fever and night sweats: These can occur without infection, signaling the body’s immune response.
- Swelling in the legs or ankles: When the kidneys struggle to regulate fluids, swelling (edema) can occur.
In advanced stages, kidney cancer can spread (metastasize) to the lungs, bones, liver, or brain, leading to symptoms such as persistent cough, bone pain, or neurological changes.
Diagnosis: Detecting the Hidden Enemy
Accurate diagnosis of kidney cancer involves a combination of patient history, imaging, laboratory tests, and sometimes biopsy. Because symptoms may be vague, many cases are first spotted through imaging done for other conditions.
Imaging Tests
- Ultrasound: Can detect kidney masses and differentiate between solid tumors and fluid-filled cysts.
- CT Scan (Computed Tomography): Provides detailed cross-sectional images to reveal the size, shape, and spread of tumors.
- MRI (Magnetic Resonance Imaging): Used when CT scans are inconclusive or when contrast dye is not an option.
- Chest X-ray or bone scan: Helps detect cancer that may have spread beyond the kidney.
Laboratory Tests
Blood and urine tests can provide clues. High levels of certain substances, such as calcium, liver enzymes, or anemia, may point to kidney cancer’s systemic effects.
Biopsy
Though not always required, a biopsy involves taking a small tissue sample from the kidney to confirm the presence and type of cancer. In some cases, imaging is so definitive that surgery proceeds without biopsy.
Staging: Measuring the Extent of Disease
Once kidney cancer is diagnosed, determining its stage is essential. Staging describes how far the cancer has spread and guides treatment decisions.
- Stage I: Tumor is confined to the kidney and measures less than 7 cm.
- Stage II: Tumor is larger than 7 cm but still contained within the kidney.
- Stage III: Cancer has spread to nearby lymph nodes or major blood vessels.
- Stage IV: Cancer has spread to distant organs such as the lungs, liver, bones, or brain.
Staging helps physicians choose the most effective treatment path, balancing aggressiveness with preservation of kidney function and quality of life.
Treatment Options
Treatment for kidney cancer depends on the type, stage, patient’s overall health, and personal preferences. Modern medicine offers a range of approaches, from surgery to targeted therapies.
Surgery: The Cornerstone of Treatment
For many patients, surgery remains the most effective treatment.
- Partial Nephrectomy: Only the tumor and a margin of surrounding tissue are removed, preserving as much of the kidney as possible. This option is often chosen for smaller tumors.
- Radical Nephrectomy: The entire kidney, surrounding fatty tissue, and sometimes nearby lymph nodes are removed. In some cases, the adrenal gland is also removed.
- Minimally Invasive Techniques: Laparoscopic or robotic-assisted surgeries allow smaller incisions, faster recovery, and reduced pain compared to open surgery.
Even with one kidney removed, many patients live normal lives, provided the remaining kidney is healthy.
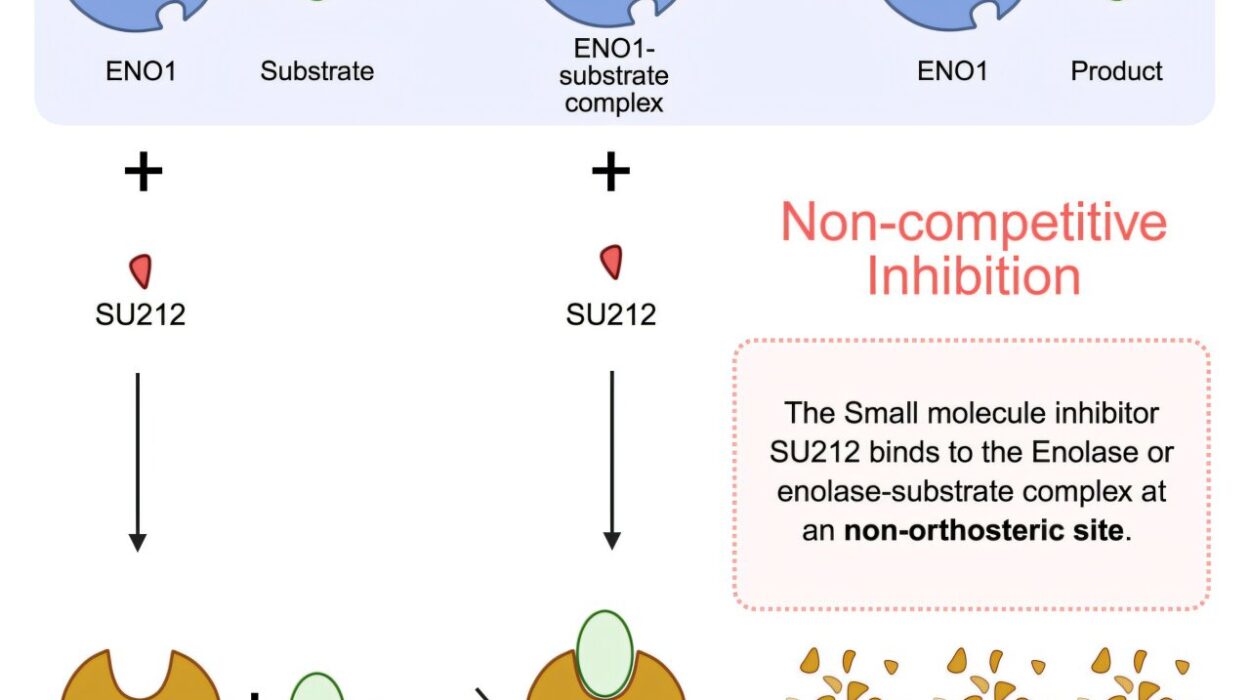
Targeted Therapy
Unlike traditional chemotherapy, which attacks rapidly dividing cells indiscriminately, targeted therapies home in on specific molecular pathways that cancer cells use to grow and spread. Drugs such as sunitinib, pazopanib, and axitinib block blood vessel formation that tumors rely on. These treatments have significantly improved survival for patients with advanced kidney cancer.
Immunotherapy
The immune system can be trained to recognize and attack cancer cells. Immune checkpoint inhibitors, such as nivolumab and pembrolizumab, unleash T-cells against tumors. Interleukin-2, an older form of immunotherapy, can also stimulate immune responses, though with more side effects.
Radiation Therapy
Radiation is not typically the first-line treatment for kidney cancer but may be used to ease symptoms, especially in metastatic cases where tumors spread to bones or the brain.
Clinical Trials and Emerging Treatments
Ongoing research explores new drug combinations, vaccines, and gene therapies. Participation in clinical trials can provide access to cutting-edge treatments not yet widely available.
Living with Kidney Cancer
A diagnosis of kidney cancer changes life overnight. Beyond medical treatment, patients must navigate emotional, psychological, and practical challenges. Support networks—family, friends, counselors, and patient advocacy groups—are vital.
Nutrition, exercise, and mental health care play essential roles during and after treatment. Balanced diets rich in fruits, vegetables, and lean proteins support healing, while gentle physical activity can improve mood and reduce fatigue. Mindfulness, meditation, and therapy can help manage the anxiety and uncertainty that often accompany cancer.
Prevention and Reducing Risk
While not all kidney cancers can be prevented, certain lifestyle choices lower risk:
- Quitting smoking.
- Maintaining a healthy weight.
- Controlling high blood pressure.
- Avoiding unnecessary exposure to harmful chemicals.
- Eating a nutrient-rich diet that supports kidney health.
These steps not only reduce the risk of kidney cancer but also improve overall health and resilience.
Hope on the Horizon
The story of kidney cancer is not only about risk and illness but also about progress and hope. Survival rates have risen steadily thanks to better imaging, earlier detection, and innovative treatments. What was once considered a devastating diagnosis is now increasingly manageable, even in advanced cases.
Researchers continue to uncover new insights into the genetic and molecular foundations of kidney cancer, opening doors to treatments that are more precise, less toxic, and more effective. With each scientific breakthrough, the landscape of kidney cancer care shifts toward greater hope.
Conclusion: Life Beyond Diagnosis
Kidney cancer reminds us of the fragility and resilience of the human body. It begins quietly, sometimes unnoticed, but its impact is profound. Yet, with awareness, timely diagnosis, and effective treatment, many people not only survive but thrive after kidney cancer.
Health is never guaranteed, but knowledge empowers us to protect it. By understanding the causes, recognizing the symptoms, pursuing early diagnosis, and embracing the latest treatments, we take back some measure of control against this hidden adversary. For those facing kidney cancer today, science, compassion, and determination offer not just survival, but the chance to live fully in the face of challenge.