The frozen dinners, sugary cereals, fizzy sodas, and processed meats that fill grocery store aisles may be doing more than just expanding waistlines. According to a new study published in Neurology, these ultra-processed foods might be quietly interfering with your brain—well before the first tremor or shuffle of Parkinson’s disease ever appears. For a condition known for its mysterious origins and slow onset, this discovery adds a compelling new layer to the unfolding story of how what we eat shapes our future health.
The Invisible Beginnings of Parkinson’s
Parkinson’s disease is often thought of as a disorder of movement—shaking hands, stiff limbs, and slow steps. But in reality, the disease begins long before these visible symptoms emerge. This pre-diagnostic period is called the prodromal phase, and it can last more than a decade. In this phase, the body whispers subtle signals that something isn’t quite right: sleep disturbances, chronic constipation, depressive moods, or an odd loss of smell. These signs are easy to ignore or misattribute, but they’re actually early markers of a brain that’s starting to struggle.
Scientists are increasingly interested in this phase, not just because it might hold clues about how the disease develops, but because it may offer a window of opportunity—an opening where intervention could delay or even prevent the disease from taking hold.
The Curious Case of Diet and Brain Health
In recent years, a striking trend has emerged: the realization that ultra-processed foods are not just empty calories—they’re potentially dangerous. Studies have already shown that these foods are linked to obesity, heart disease, diabetes, and even cancer. But more alarmingly, mounting evidence suggests that they may also impair brain health.
A 2022 study linked high ultra-processed food intake to a greater risk of dementia. This prompted researchers to ask a new question: if these foods are associated with one major neurodegenerative disease, could they be connected to another?
A New Study, A Troubling Connection
Led by Xiang Gao of the Institute of Nutrition at Fudan University, the new study zeroed in on this very question. Gao and his team examined decades of data from two of the largest and most respected health studies in the world: the Nurses’ Health Study and the Health Professionals Follow-Up Study. These long-term investigations have followed the health habits of tens of thousands of American adults—nurses, doctors, dentists, and other medical professionals—since the 1980s.
For this new research, the team analyzed information from nearly 43,000 participants, most in middle age and about 59% women. They looked at self-reported dietary data collected every few years and matched it against early signs of Parkinson’s disease.
Crucially, they didn’t study people already diagnosed with Parkinson’s. Instead, they focused on the prodromal symptoms—those subtle signs that often appear long before a diagnosis. These included constipation, REM sleep behavior disorder (where people act out their dreams), reduced sense of smell, vision changes, body pain, daytime drowsiness, and depressive symptoms.
Processed Foods and Early Brain Warnings
The findings were sobering. People who consumed the highest amounts of ultra-processed foods were significantly more likely to show three or more early signs associated with Parkinson’s disease. In fact, compared to those who ate the least ultra-processed foods, individuals in the top fifth of consumption were 2.5 times more likely to exhibit multiple prodromal symptoms.
Even after accounting for potential confounders—age, smoking, physical activity, alcohol use, caffeine intake, and even total calorie consumption—the pattern remained.
Certain types of symptoms were particularly linked to processed food consumption. Probable REM sleep behavior disorder, depressive symptoms, constipation, and unexplained body pain were all more common in heavy consumers of ultra-processed foods. While links with smell loss and visual impairment were less consistent, the overall trend was clear: the more ultra-processed food people ate, the more likely they were to show signs of a brain heading toward Parkinson’s.
What Counts as “Ultra-Processed,” Anyway?
The term “ultra-processed” isn’t just a buzzword. According to the NOVA food classification system used in the study, ultra-processed foods are those that go far beyond simple canning or freezing. They are industrially manufactured products, often containing a laundry list of additives, colorants, flavor enhancers, artificial sweeteners, preservatives, and emulsifiers. Their ingredients are typically not found in a home kitchen—think protein isolates, hydrogenated oils, high-fructose corn syrup, and flavoring agents created in laboratories.
The team found that certain categories of ultra-processed foods were especially problematic. These included processed meats like hot dogs and deli slices, sugary snacks, artificially sweetened beverages, dairy-based desserts, and packaged sauces and condiments. Each of these food groups was linked with a higher likelihood of experiencing the early warning signs of Parkinson’s disease.
A Long Road to Symptoms
One strength of this study was its attempt to sidestep one of the common pitfalls of dietary research: reverse causality. Could it be that people already developing symptoms changed their eating habits, rather than the other way around?
To address this, the researchers analyzed only dietary data that was collected at least six years before participants reported prodromal symptoms. In some cases, they looked back as far as 1986, allowing them to establish long-term patterns of food consumption before any early symptoms appeared. Even with this buffer, the associations remained strong.
A Gut Feeling About Parkinson’s
So, what could explain the connection between ultra-processed foods and early signs of Parkinson’s? One intriguing possibility involves the gut.
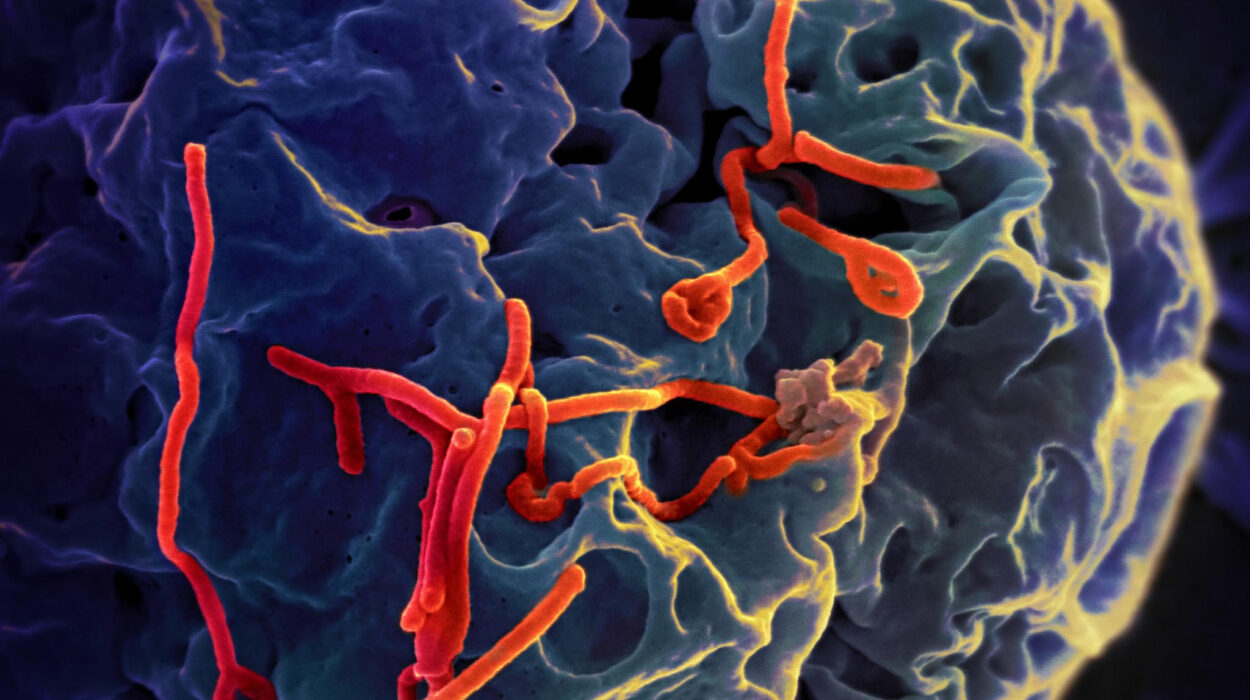
In recent years, researchers have begun to suspect that Parkinson’s disease might actually begin in the gastrointestinal system. Abnormal proteins called alpha-synuclein, which accumulate in the brains of Parkinson’s patients, have also been found in the intestines years before brain symptoms develop. From there, it’s thought they might travel up the vagus nerve—a sort of communication highway between the gut and the brain.
Ultra-processed foods, often low in fiber and high in synthetic ingredients, can disrupt the gut microbiome. This can lead to increased intestinal inflammation, a “leaky gut,” and abnormal immune responses—all of which might contribute to the pathological processes that ultimately damage dopamine-producing neurons in the brain.
Inflammation, Toxins, and Brain Damage
Beyond the gut, ultra-processed foods may also exert direct effects on the brain. Many contain emulsifiers and preservatives that, in animal studies, have been shown to promote systemic inflammation. Others are high in advanced glycation end products (AGEs), toxic compounds formed when food is cooked at high temperatures.
These pro-inflammatory molecules can cross the blood-brain barrier and promote oxidative stress, damaging the very neurons that are most vulnerable in Parkinson’s disease. Additionally, some of the packaging materials used in processed foods—such as BPA in plastics—may act as endocrine disruptors, interfering with brain signaling pathways.
And then there’s the issue of artificial sweeteners. While marketed as healthier alternatives to sugar, some of these compounds have been shown in laboratory studies to alter brain chemistry and affect the gut microbiome in unpredictable ways.
A Word of Caution: Correlation Is Not Causation
Despite the strong associations, the researchers were careful to point out that their findings do not prove that ultra-processed foods cause Parkinson’s disease. This was an observational study, which means it can show links but not direct cause and effect.
There could be unmeasured factors—such as genetics, environmental exposures, or other lifestyle habits—that partly explain the association. Moreover, the participants in the study were mostly White health professionals, which may limit how generalizable the results are to more diverse populations.
Dietary intake was self-reported, introducing the possibility of recall bias or underreporting. And while the NOVA system is widely used, categorizing foods based on processing can be tricky, especially when meals contain a mix of ingredients.
So, What Should You Eat Instead?
Still, the findings support a growing body of research suggesting that a diet high in ultra-processed foods is bad for your brain. On the flip side, diets rich in whole foods—vegetables, fruits, legumes, nuts, and unprocessed grains—have been associated with lower risks of neurodegenerative diseases.
The Mediterranean diet, for example, which emphasizes olive oil, leafy greens, fish, and fresh produce, has been linked to better brain aging and reduced risk of cognitive decline. Similarly, the MIND diet (a hybrid of the Mediterranean and DASH diets) is specifically designed to protect brain function.
By choosing foods closer to their natural form and cutting back on industrially processed products, we may be giving our brains the best chance at staying healthy for the long haul.
Looking Ahead
As researchers continue to unravel the causes of Parkinson’s disease, diet is emerging as a critical piece of the puzzle. While we still don’t have a cure—and much remains unknown about the precise mechanisms that link food to brain health—studies like this one offer a powerful reminder: our daily choices matter.
The things we eat every day, often without thinking, are not neutral. They are shaping our bodies, our minds, and perhaps even our futures.
So the next time you’re reaching for a brightly packaged snack or a microwaveable meal, take a moment to ask yourself: is this food fueling my health—or quietly working against it?