When a young person walks into an emergency room with chest pain just a day or two after receiving an mRNA COVID-19 vaccine, doctors face a difficult puzzle. There is no virus in sight. No clogged arteries. But there is pain, inflammation and, in many cases, a troubling rise of cardiac troponin in the blood, a sign that heart muscle cells are suffering.
For years, scientists understood only the outline of this rare reaction known as vaccine-associated myocarditis. They knew it happened quickly, tended to affect young men most often and usually resolved with time. But the deeper question remained stubbornly unanswered. What exactly was happening inside the body to cause heart tissue to react this way.
A new study from Stanford Medicine, published in Science Translational Medicine, now opens a door into that hidden biology. The research offers not only a mechanism but also a potential way to reduce the risk without weakening protection against COVID-19.
The Search for a Hidden Sequence
Joseph Wu, MD, PhD, director of the Stanford Cardiovascular Institute, began with a simple but crucial truth. “The mRNA vaccines have done a tremendous job mitigating the COVID pandemic,” he said. “Without these vaccines, more people would have gotten sick, more people would have had severe effects and more people would have died.”
Still, the lingering question demanded attention. “Medical scientists are quite aware that COVID itself can cause myocarditis,” Wu said. “To a lesser extent, so can the mRNA vaccines. The question is, why.”
To find answers, Wu, senior author Masataka Nishiga, MD, PhD, and lead author Xu Cao, PhD, turned to data from vaccinated individuals. Among those who developed myocarditis, two proteins consistently appeared in elevated amounts in their blood. “Two proteins, named CXCL10 and IFN-gamma, popped up. We think these two are the major drivers of myocarditis,” Wu said.
Both belong to the immune system’s chemical messaging system, cytokines—molecules that help immune cells communicate. But the Stanford team suspected these two weren’t simply sending messages. They were triggering a damaging sequence.
A Conversation Between Cells
To listen to this biological conversation more closely, the researchers created human immune cells called macrophages in a dish and exposed them to mRNA vaccine. The macrophages reacted like soldiers on high alert, pumping out cytokines—especially CXCL10. This mirrored what has been observed in human vaccine responses.
Then the scientists brought in another cast member of the immune system: T cells. These patrolling cells can spark targeted attacks, but they can also arouse broad immune activity.
When T cells were introduced to the macrophage bathwater—the solution that held everything the macrophages had secreted—the T cells responded with a surge of IFN-gamma. But when T cells encountered the vaccine alone, without the influence of macrophages, they behaved normally. This revealed a two-step cascade. Macrophages produce CXCL10. That CXCL10 awakens T cells. The T cells then release IFN-gamma.
In other words, the vaccine’s interaction with macrophages starts a conversation that ends with heightened immune activity. Enough activity, the team suspected, to damage heart cells.
When the Heart Feels the Fire
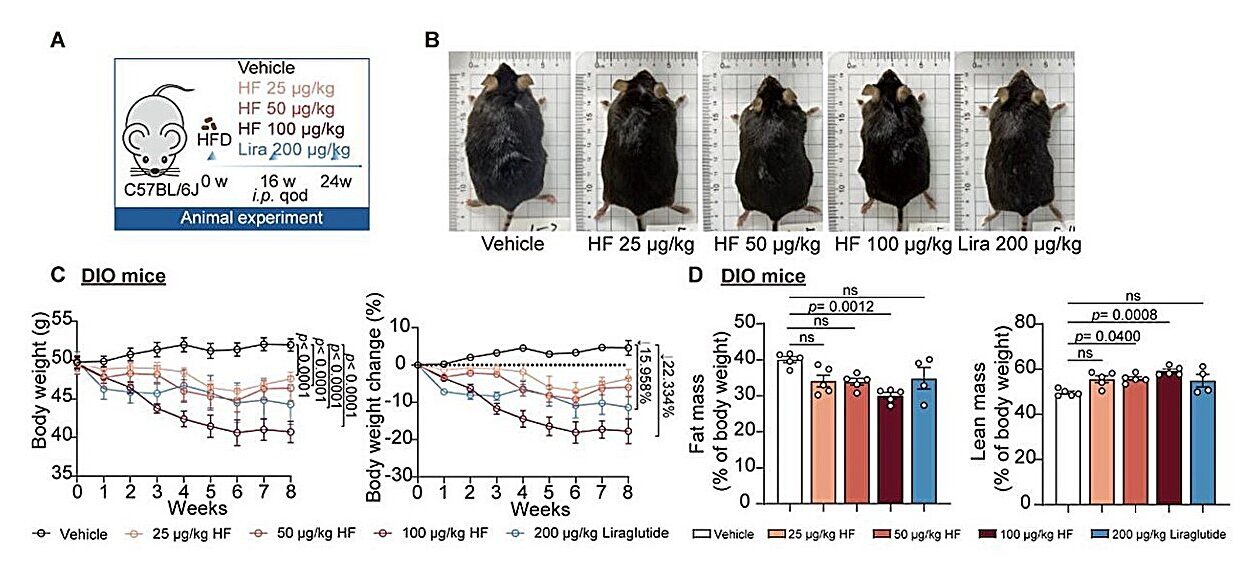
To test whether these two cytokines truly caused harm, the researchers vaccinated young male mice. The results mirrored human cases. Levels of cardiac troponin rose—an unmistakable sign that heart muscle cells were under stress or being injured.
The scientists also saw macrophages and neutrophils infiltrating the heart tissue. Neutrophils, short-lived immune cells that specialize in fast, aggressive attacks, often create collateral damage. Their presence in the heart hinted at a system responding with more force than necessary.
Both macrophage and neutrophil infiltration diminished when CXCL10 and IFN-gamma were blocked. Notably, the protective effect did not weaken the broader immune response to vaccination. The heart was spared without sacrificing defense.
They found something else too. The hearts of vaccinated mice displayed increased levels of molecules that help immune cells stick to blood vessel walls—like microscopic hooks that pull more immune cells into the area. These also decreased when the two cytokines were inhibited.
At this point, the Stanford team had strong evidence. CXCL10 and IFN-gamma were not just markers or correlates. They were active participants in cardiac injury.
The Heart in a Dish
Wu’s lab used an advanced technique to grow miniature beating heart structures called cardiac spheroids. These tiny models mimic real heart tissue, allowing researchers to test effects in a controlled environment.
When bathed in CXCL10 and IFN-gamma—the same cocktail produced by the immune cell dance—the spheroids showed stress. Their beating weakened. Their rhythm faltered. Their molecular markers signaled distress.
When inhibitors of the cytokines were added, the damage eased. The heart models stabilized. The story unfolding in human data, in immune cells and in mice played out again in these tiny beating spheres.
The Unexpected Clue Hidden in Soybeans
Wu had one more idea. Years earlier, his team had studied a soybean-derived compound called genistein. In 2022, they published research showing that genistein had anti-inflammatory properties and could protect cardiovascular tissue from certain forms of damage. And genistein had another curious property. It acts a bit like estrogen—a hormone with known anti-inflammatory effects. Young men, the group most affected by post-vaccine myocarditis, have less estrogen than women.
So the team tested genistein again.
They pre-treated cells, cardiac spheroids and even live mice with purified, concentrated genistein. The results echoed across every experiment. The damage caused by the mRNA vaccine, by CXCL10 and by IFN-gamma diminished. Heart cells fared better. Troponin levels fell. Function improved.
The doses used in the experiments were far stronger than what a person could get by eating soy products. But the concept was clear. An anti-inflammatory agent, even one modeled after something found in common food, could calm the cytokine storm before it harmed the heart.
“Nobody ever overdosed on tofu,” Wu said, noting that dietary versions of genistein are too weak to cause concern. But purified forms might eventually help scientists design ways to reduce myocarditis risk.
Why This Discovery Matters
The vast majority of myocarditis cases linked to mRNA vaccines are mild and resolve quickly. “It’s not a heart attack in the traditional sense,” Wu said. “When symptoms are mild and the inflammation hasn’t caused structural damage to the heart, we just observe these patients to make sure they recover.”
Severe cases are rare. Deaths are rarer still. Meanwhile, COVID-19 itself is about ten times more likely to cause myocarditis than the vaccines—a point Wu emphasizes repeatedly.
But understanding the biology behind this reaction is more than an academic victory. It offers a path toward safer vaccine strategies, especially as mRNA technology expands beyond COVID-19 to other diseases. It suggests that cytokine signaling, especially involving CXCL10 and IFN-gamma, may be a shared mechanism behind inflammatory effects in other organs as well. And it invites the possibility that targeted inhibitors—or compounds like purified genistein—could tame excessive immune responses while preserving protection.
Most importantly, this research removes uncertainty. It replaces speculation with clarity, mapping a molecular chain of events from the first immune spark to the final moment when heart cells feel the consequences. In doing so, it strengthens confidence in vaccination and builds tools to make future versions even safer.
The mystery of vaccine-related myocarditis is not fully solved, but the path forward is now illuminated. Through careful experiments, patient observation and a touch of insight from an ordinary soybean, scientists have pieced together a story the body has been telling all along.
More information: Xu Cao et al, Inhibition of CXCL10 and IFN-γ ameliorates myocarditis in preclinical models of SARS-CoV-2 mRNA vaccination, Science Translational Medicine (2025). DOI: 10.1126/scitranslmed.adq0143 , www.science.org/doi/10.1126/scitranslmed.adq0143