The world often tells a new mother that she should be glowing. That the tiny bundle in her arms should make every sleepless night worth it. That this is the most magical time of her life. But behind the Instagram posts and baby shower balloons, there’s a quiet, persistent fear creeping in. A pounding heart at 3 a.m. over something that hasn’t even happened. A gnawing sense of dread when the baby finally sleeps. A hyper-vigilance so consuming it becomes its own form of exhaustion.
This is not simply new mom jitters or the infamous “baby blues.” This is postpartum anxiety—a condition that affects countless women in the shadows of their new motherhood. Unlike postpartum depression, which has increasingly entered mainstream conversations, postpartum anxiety often goes unnamed, undiagnosed, and misunderstood. But it is no less real and no less disruptive.
Understanding Postpartum Anxiety Beyond the Stereotypes
Postpartum anxiety is a mental health condition characterized by excessive, persistent worry that occurs after giving birth. While every new parent experiences concern for their child’s safety and wellbeing, postpartum anxiety takes those concerns and spins them into overwhelming spirals. It can latch onto thoughts that feel impossible to ignore, creating physical symptoms like racing heart, dizziness, nausea, restlessness, and even panic attacks.
What makes postpartum anxiety so tricky is that it doesn’t always look like someone who’s visibly struggling. Many mothers who suffer from it are able to perform daily caregiving tasks, which makes it even more insidious. They may look composed on the outside—feeding, diapering, rocking the baby to sleep—but internally, their minds are in constant overdrive. They’re battling the “what-ifs” relentlessly, even when nothing is actually wrong.
Unlike depression, which often brings sadness and detachment, anxiety is the voice screaming, “What if you drop the baby? What if she stops breathing while she sleeps? What if you made a terrible mistake becoming a parent?” It’s hyper-awareness. It’s fight-or-flight mode on a loop. And it’s exhausting.
A Battle Between Biology and Emotion
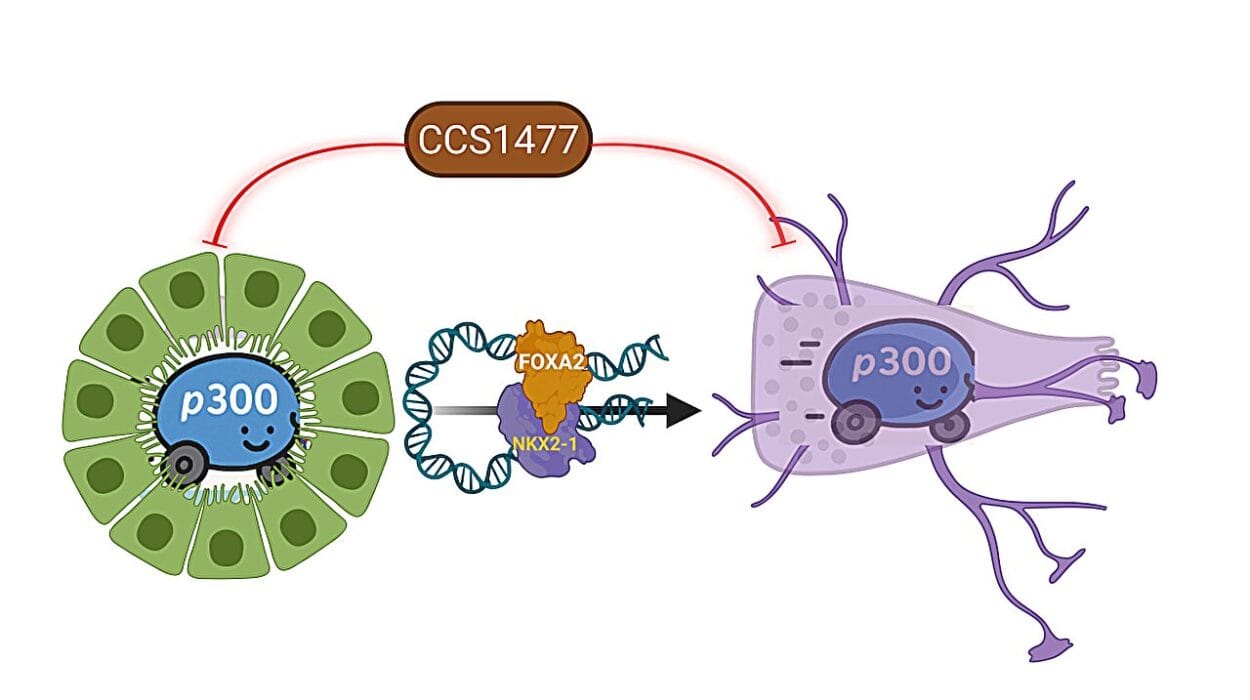
It’s easy to assume anxiety is just an emotional response to stress, but the truth is, it’s deeply rooted in biology. After childbirth, a woman’s body undergoes a dramatic hormonal shift. Estrogen and progesterone levels, which soared during pregnancy, plummet within hours of delivery. Add to that the flood of oxytocin during breastfeeding, the lack of sleep, and the physiological demands of recovery, and you have the perfect biochemical storm for anxiety to brew.
These hormones don’t just regulate reproductive function—they play a key role in mood stability, stress regulation, and emotional resilience. When they fluctuate wildly, as they do postpartum, the brain’s capacity to manage fear and worry is compromised. Cortisol, the stress hormone, may remain elevated in some women, keeping them in a state of heightened alertness long after the actual need has passed.
This doesn’t mean anxiety is “all in your head.” On the contrary, it means it’s very much in your body—embedded in neural circuits and chemical balances that are profoundly affected by childbirth. Understanding this is the first step toward breaking the stigma. A woman with postpartum anxiety isn’t weak, dramatic, or failing. She’s undergoing a massive neurochemical adjustment and trying to survive it while caring for a newborn.
The Silent Sister of Postpartum Depression
Postpartum depression and postpartum anxiety often go hand in hand, but they are not the same. In fact, many mothers with postpartum anxiety never experience the classic signs of depression like deep sadness or disinterest in the baby. Instead, they feel on edge, frantic, and panicked.
Yet because postpartum depression is more widely recognized, anxiety often gets lumped under its umbrella. This lack of distinction leads to underdiagnosis and undertreatment. A woman may know to watch for signs of depression but not recognize that her excessive checking, inability to relax, or terrifying intrusive thoughts are also part of a mental health issue.
This is especially problematic because postpartum anxiety can be just as debilitating—if not more so—than depression. It can lead to sleep disturbances that further worsen mental health, interfere with mother-infant bonding, and increase the risk of future psychiatric disorders. And it doesn’t always go away on its own. Without intervention, postpartum anxiety can persist for months or even years, shaping a woman’s experience of motherhood in painful ways.
Intrusive Thoughts: The Anxiety No One Wants to Admit
One of the most terrifying aspects of postpartum anxiety is the presence of intrusive thoughts. These are unwelcome, often violent or disturbing thoughts that seem to pop into the mind without warning. A mother may suddenly imagine dropping her baby down the stairs or smothering her child with a pillow—not because she wants to, but because her brain is misfiring in a way that feels deeply shameful and horrifying.
Many women who experience these thoughts are too scared to talk about them. They fear judgment, or worse, losing custody of their child. But intrusive thoughts are actually very common in postpartum anxiety and are not indicative of intent or character. They are symptoms, not sins.
The truth is, our brains are wired to envision potential dangers as a way of keeping us safe. When anxiety is high, this protective mechanism becomes distorted. The brain begins to misfire safety alarms, producing thoughts that feel terrifyingly real but have no basis in actual desire or intent.
Therapists trained in perinatal mental health understand this phenomenon and can help women manage these thoughts safely and without judgment. But the silence around intrusive thoughts remains a major barrier to recovery.
When Protection Turns into Paranoia
Motherhood awakens a powerful instinct to protect. In many ways, anxiety is born from love—the desperate desire to keep a fragile new life safe in an unpredictable world. But in postpartum anxiety, this protective instinct goes rogue.
A mother with postpartum anxiety might avoid leaving the house for fear of germs or accidents. She might refuse to let anyone else hold the baby, convinced that only she can do it right. She may obsessively monitor every breath, every sound, every nap, unable to relax even for a moment. These behaviors are driven by fear, not logic, and they can quickly escalate into compulsions that control her life.
The line between vigilance and obsession can become blurred. What starts as cautious parenting can spiral into a prison of routines and restrictions, all in the name of safety. And ironically, this attempt to protect often ends up hurting—by isolating the mother, creating conflict in relationships, and interfering with the joy of bonding with her baby.
Recognizing this spiral is difficult. Anxiety often disguises itself as responsibility, as love, as “just being careful.” But when the anxiety becomes the loudest voice in a mother’s head, it’s time to listen and seek help.
Fathers and Postpartum Anxiety: The Hidden Sufferers
Though postpartum anxiety is more commonly associated with mothers, it’s important to recognize that fathers and non-birthing partners can also experience it. The pressure to provide, the fear of not being good enough, the sleep deprivation, and witnessing a partner’s distress can all trigger anxiety in new dads.
Men are less likely to seek help due to societal expectations around masculinity and emotional expression. This often leads to irritability, anger, withdrawal, or even substance use as coping mechanisms. Raising awareness that postpartum anxiety affects the whole family—regardless of gender—can help normalize help-seeking and create a more supportive postpartum environment for everyone.
What Recovery Looks Like: Hope in the Chaos
The good news is that postpartum anxiety is treatable. With the right support, most women (and men) recover fully and go on to enjoy healthy, balanced parenthood. The path to healing is not one-size-fits-all, but it often involves therapy, support groups, self-care, medication when necessary, and most of all—validation.
Cognitive-behavioral therapy (CBT) is one of the most effective treatments, helping individuals identify and challenge distorted thought patterns. Exposure therapy may also be used to reduce compulsive checking or avoidance behaviors. For those with severe symptoms, medication like SSRIs can provide much-needed relief and balance.
Equally important is the role of community. Postpartum anxiety thrives in isolation, but it often weakens in the light of shared experience. Support groups, whether in person or online, give mothers a space to speak their fears without shame. Even just hearing another mom say, “I felt that too,” can be profoundly healing.
Self-care is not just bubble baths and quiet time—it’s about reclaiming a sense of self outside of motherhood. It’s sleep. It’s nourishment. It’s boundaries. It’s asking for help, unapologetically. And most of all, it’s the radical act of choosing to prioritize your mental health not just for your baby, but for yourself.
Why We Need to Talk About It More
Postpartum anxiety affects an estimated 10-15% of new mothers, but experts believe the real number is much higher due to underreporting. The silence surrounding maternal mental health, especially anxiety, is rooted in centuries of societal expectations that idealize motherhood and demonize any deviation from it.
There is still a cultural script that says a good mother should be selfless, tireless, and unflinchingly joyful. That script leaves little room for the complex emotional realities of postpartum life. When mothers do speak out, they’re often met with platitudes—“It’s just hormones,” or “You’ll feel better soon”—that minimize their experience and delay healing.
We need more than awareness. We need action. That means better screening at postpartum check-ups, increased access to perinatal mental health specialists, parental leave policies that support both parents, and a cultural shift toward honesty over perfection.
Motherhood is not a fairytale. It’s a messy, miraculous, and often maddening journey that deserves compassion at every step.
A Future Where Anxiety Doesn’t Win
Imagine a world where a new mother can walk into her pediatrician’s office and say, “I’m feeling overwhelmed and anxious,” and be met with support, not suspicion. A world where postpartum care includes mental health as a standard, not a luxury. A world where mothers don’t feel like they have to pretend they’re okay when they’re falling apart inside.
That world is possible. But only if we keep talking about it. Only if we choose to believe women when they say they’re struggling. Only if we replace judgment with empathy and silence with understanding.
Postpartum anxiety doesn’t mean you’re a bad mother. It means you’re a mother who needs support, just like every other human navigating one of life’s biggest transformations.
So if you’re reading this and recognizing yourself in these words—know this: You are not alone. You are not broken. And you do not have to suffer in silence.
Healing is not only possible—it’s your birthright too.