Pancreatic cancer is often called a “silent killer.” Unlike some other cancers that make themselves known early through clear warning signs, pancreatic cancer grows quietly, hidden deep inside the abdomen, often escaping detection until it has advanced. By the time symptoms appear, the disease is frequently in a stage where treatment becomes more complex and survival rates are lower. Yet despite this grim reputation, research, awareness, and medical innovation are bringing new hope to patients and families affected by this devastating condition.
To understand pancreatic cancer is to step into one of the most intricate battles in modern medicine. It is not just a disease of cells growing uncontrollably; it is a challenge of biology, timing, and resilience. Learning about its causes, symptoms, diagnosis, and treatment is not merely academic—it is an act of awareness that can empower us to recognize risks, support loved ones, and value the cutting-edge science that pushes forward in the face of daunting odds.
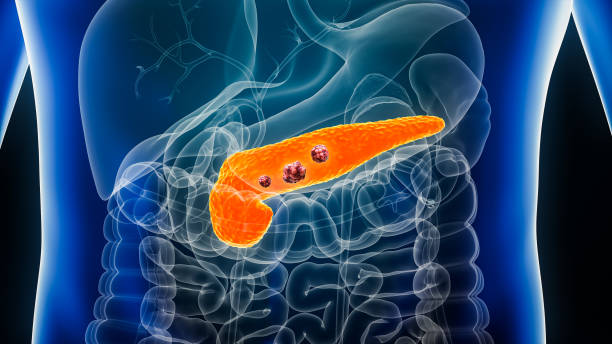
Understanding the Pancreas
Before we can explore pancreatic cancer, we must first understand the organ it arises from. The pancreas is a long, flat gland nestled in the abdomen, lying behind the stomach and in close connection with the liver, intestines, and gallbladder. Despite its discreet position, the pancreas performs essential functions that keep the body alive and thriving.
It has two main roles:
- Exocrine function: The pancreas produces digestive enzymes that help break down fats, proteins, and carbohydrates, ensuring the body can absorb nutrients from food.
- Endocrine function: It secretes hormones, including insulin and glucagon, which regulate blood sugar levels and maintain energy balance.
This dual nature—both digestive and hormonal—makes the pancreas a uniquely important organ. Unfortunately, its deep location also makes early tumors difficult to detect, often delaying diagnosis until the disease has spread.
What is Pancreatic Cancer?
Pancreatic cancer occurs when cells in the pancreas begin to grow uncontrollably, ignoring the normal rules of cell life and death. These rogue cells can form tumors that disrupt the pancreas’s vital functions, spread to surrounding tissues, and metastasize to distant organs.
There are several types of pancreatic cancer, but they generally fall into two categories:
- Exocrine tumors: The vast majority of cases, usually pancreatic ductal adenocarcinoma, which develops in the ducts that carry digestive enzymes.
- Endocrine tumors (pancreatic neuroendocrine tumors): Less common, arising from the hormone-producing cells of the pancreas.
While neuroendocrine tumors can sometimes grow more slowly and may have better treatment outcomes, the exocrine type—adenocarcinoma—is the most aggressive and deadly.
Causes and Risk Factors
Cancer does not develop overnight. It is the result of genetic mutations—changes in the DNA of cells—that accumulate over time and disrupt the normal checks and balances of cell growth. In pancreatic cancer, these mutations may occur in tumor suppressor genes, oncogenes, or DNA repair genes, leading to uncontrolled proliferation.
Some causes and risk factors have been identified:
Genetic Influences
Certain inherited mutations increase the risk of pancreatic cancer. For example, mutations in the BRCA1 and BRCA2 genes, commonly linked to breast and ovarian cancer, also raise pancreatic cancer risk. Familial pancreatic cancer, though rare, occurs when multiple family members are affected, suggesting a genetic predisposition.
Lifestyle and Environmental Factors
- Smoking: One of the most significant modifiable risk factors. Smokers are two to three times more likely to develop pancreatic cancer.
- Obesity: Excess weight contributes to chronic inflammation and insulin resistance, which can promote cancer development.
- Diet: Diets high in processed meats, red meat, or sugary foods may elevate risk, while diets rich in fruits, vegetables, and whole grains may reduce it.
- Alcohol abuse: Long-term heavy drinking can lead to chronic pancreatitis, a condition that increases cancer risk.
Medical Conditions
- Chronic pancreatitis: Persistent inflammation of the pancreas damages cells and can predispose them to malignant transformation.
- Diabetes: Both a risk factor and sometimes an early symptom of pancreatic cancer, particularly when diabetes develops suddenly in older adults.
- Liver conditions: Cirrhosis or chronic hepatitis may contribute to higher risk due to systemic effects on digestion and metabolism.
No single cause guarantees pancreatic cancer, but the combination of genetics, environment, and lifestyle contributes to vulnerability.
Symptoms: Why It Is Often Called a Silent Disease
One of the greatest challenges with pancreatic cancer is that its symptoms are often vague, nonspecific, or appear only when the disease has already progressed. This is why it earns the reputation of being silent—and deadly.
Common symptoms include:
- Jaundice: Yellowing of the skin and eyes, caused by a tumor blocking the bile duct. This is often one of the earliest noticeable signs.
- Abdominal or back pain: Pain may develop as the tumor presses on surrounding organs or nerves.
- Unexplained weight loss: Cancer cells consume a large amount of energy, and disrupted digestion prevents proper nutrient absorption.
- Loss of appetite and digestive problems: Tumors can interfere with enzyme secretion, leading to nausea, vomiting, or indigestion.
- New-onset diabetes: Particularly in older adults without risk factors, sudden diabetes can be a warning sign.
- Fatigue: A general sense of weakness or exhaustion is common.
The problem is that these symptoms overlap with many less serious conditions, such as gallstones, ulcers, or gastrointestinal issues. This often leads to delays in diagnosis.
How Pancreatic Cancer Is Diagnosed
Because symptoms appear late, effective diagnosis requires a combination of imaging, laboratory testing, and sometimes genetic analysis. Early detection remains one of the greatest unmet challenges in medicine, but once suspected, the diagnostic pathway is precise and multi-layered.
Imaging Techniques
- CT scans and MRI: Provide detailed images of the pancreas, helping detect tumors and assess their spread.
- Endoscopic ultrasound (EUS): A small ultrasound device inserted through the digestive tract offers high-resolution images and allows tissue sampling.
- Positron Emission Tomography (PET scans): Highlights areas of high metabolic activity, which may indicate cancerous cells.
Biopsy
The definitive diagnosis of pancreatic cancer usually requires a biopsy—removing a small piece of tissue for microscopic analysis. This can be done during an endoscopic procedure guided by ultrasound or imaging.
Blood Tests
While no blood test alone can confirm pancreatic cancer, certain markers like CA 19-9 can indicate disease presence or progression. However, these markers are not specific enough for general screening.
Genetic Testing
In families with a history of pancreatic or related cancers, genetic testing may identify inherited mutations, helping guide both prevention and treatment strategies.
Staging the Cancer
Once pancreatic cancer is diagnosed, staging determines how advanced the disease is and what treatment options may be effective. Staging considers tumor size, lymph node involvement, and metastasis (spread to other organs).
- Stage I: Localized within the pancreas.
- Stage II: Spread to nearby tissues or lymph nodes.
- Stage III: Involvement of major blood vessels, making surgery more complex.
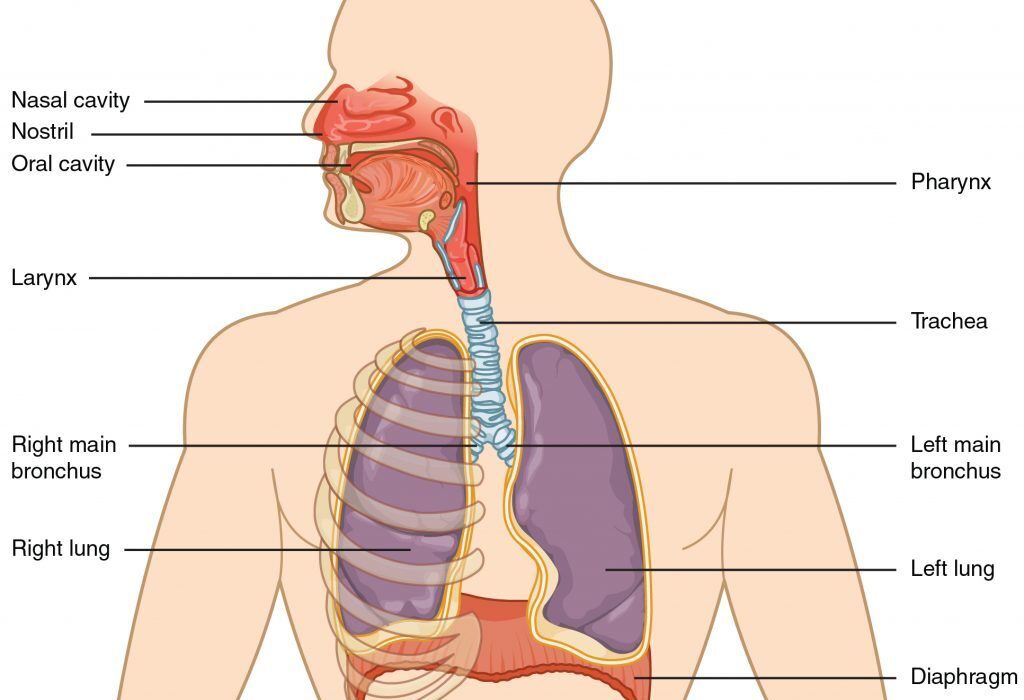
- Stage IV: Spread to distant organs like the liver or lungs.
The earlier the stage, the more treatment options are available, particularly surgical removal.
Treatment Options
Pancreatic cancer treatment is complex, requiring a multidisciplinary approach. Doctors, surgeons, oncologists, radiologists, nutritionists, and palliative care specialists often work together to provide the best outcome for each patient.
Surgery
Surgery offers the only potential cure, but only a minority of patients (around 15–20%) are diagnosed early enough to be eligible. The main surgical procedures include:
- Whipple procedure (pancreaticoduodenectomy): Removes the head of the pancreas along with part of the stomach, duodenum, gallbladder, and bile duct.
- Distal pancreatectomy: Removes the body and tail of the pancreas, often along with the spleen.
- Total pancreatectomy: Removes the entire pancreas, requiring lifelong insulin and enzyme replacement.
Surgery is demanding, but advances in technique and post-operative care are improving survival and recovery.
Chemotherapy
Chemotherapy uses powerful drugs to kill rapidly dividing cancer cells. Common regimens for pancreatic cancer include FOLFIRINOX (a combination of four drugs) or gemcitabine-based therapies. These may be used before surgery to shrink tumors (neoadjuvant therapy), after surgery to reduce recurrence risk (adjuvant therapy), or as the main treatment in advanced cases.
Radiation Therapy
Radiation uses high-energy beams to target and destroy cancer cells. It is often combined with chemotherapy to improve effectiveness, especially in cases where surgery is not possible.
Targeted Therapy and Immunotherapy
Modern medicine is increasingly turning toward personalized approaches:
- Targeted therapies block specific molecules involved in cancer growth. For example, PARP inhibitors may help patients with BRCA mutations.
- Immunotherapy aims to harness the immune system against cancer. While progress has been slower in pancreatic cancer compared to other cancers, ongoing trials hold promise.
Palliative Care
When cure is not possible, treatment focuses on quality of life—relieving pain, managing digestion, and providing emotional support. Palliative care is not about giving up; it is about ensuring dignity, comfort, and meaning for patients and families.
Emotional and Social Dimensions
Beyond biology, pancreatic cancer is also an emotional and social battle. Patients and their loved ones face fear, uncertainty, and often grief. The rapid progression of the disease can leave little time to process, adapt, or plan.
Emotional support, counseling, and connection to patient communities become essential parts of care. Sharing experiences with others who understand can provide strength. For families, the journey often involves balancing hope with realism, advocacy with acceptance, and love with loss.
Research and Future Directions
Although pancreatic cancer remains one of the most difficult cancers to treat, research is moving forward. Scientists are exploring:
- Liquid biopsies: Blood tests that detect cancer DNA fragments, potentially allowing earlier detection.
- Genomic medicine: Tailoring treatments to a patient’s unique tumor mutations.
- Nanotechnology: Delivering drugs directly to cancer cells with precision.
- New immunotherapies: Training the immune system to better recognize and attack pancreatic tumors.
Every discovery brings a step closer to turning pancreatic cancer from a deadly disease into a manageable condition.
The Importance of Awareness and Prevention
While not all cases of pancreatic cancer can be prevented, awareness and lifestyle choices can reduce risk. Avoiding smoking, maintaining a healthy weight, eating a nutrient-rich diet, and limiting alcohol are meaningful steps. For those with strong family histories, genetic counseling may provide critical insights.
Early detection remains the greatest hope. Awareness of warning signs, such as sudden unexplained diabetes or persistent jaundice, can lead to earlier investigation and potentially life-saving interventions.
Living with Pancreatic Cancer
For those diagnosed, living with pancreatic cancer means navigating uncertainty but also discovering strength. Many patients describe a new appreciation for time, relationships, and small joys. Families often come together in profound ways, building memories even in the shadow of illness.
Healthcare teams emphasize not only medical treatment but also nutrition support, pain management, psychological counseling, and spiritual care. Hope may not always mean cure, but it can mean comfort, dignity, and love.
Conclusion: A Journey of Science and Humanity
Pancreatic cancer is one of the greatest challenges in modern oncology. It is relentless, often silent, and biologically complex. Yet, within this challenge lies an extraordinary story of resilience—from the courage of patients to the dedication of doctors, from the compassion of caregivers to the determination of scientists.
Understanding pancreatic cancer—its causes, symptoms, diagnosis, and treatment—is more than knowledge. It is a call to awareness, to prevention, to advocacy, and to hope. Even in the face of a disease so formidable, humanity’s response is clear: to fight with science, to care with compassion, and to live with meaning.