For decades, one haunting question has lingered in the minds of colon cancer survivors and their doctors: When can we finally say a person is cured? Now, a powerful collaboration between IRCCS Ospedale Policlinico San Martino, the Mayo Clinic, and several other international cancer research centers may have finally delivered an answer — one grounded in data, science, and renewed hope.
In an extraordinary pooled analysis published in JAMA Oncology titled “The Definition of Cure in Colon Cancer,” researchers have revealed that the risk of colon cancer recurrence falls below 0.5% after six years following surgery. For patients who have lived through the anxiety of relapse fears, this discovery provides more than just numbers — it offers peace, clarity, and a practical definition of cure.
The Struggle to Define “Cure”
Colon cancer is one of the most common cancers worldwide. While survival rates have steadily improved over the past decades thanks to early detection, surgery, and chemotherapy, the question of when a patient can be considered truly cured has remained uncertain.
Traditionally, studies assessing colon cancer outcomes have combined multiple end points: deaths, recurrences, and even the appearance of unrelated second tumors. While these comprehensive measures provided a broad view of outcomes, they often blurred the boundary between “living without disease” and “being cured.”
For patients and clinicians alike, this ambiguity has real emotional weight. Every follow-up test, every scan, every doctor’s visit carries the silent question: Is it back? Defining a precise moment when relapse risk becomes negligible could fundamentally change how survivors live after treatment — allowing them to reclaim their futures without the constant shadow of uncertainty.
A Landmark Pooled Analysis
To tackle this question with statistical rigor, researchers conducted one of the largest and most comprehensive analyses ever undertaken in colon cancer. The study included 35,213 patients with stage II to stage III colon cancer, drawn from 15 Phase III randomized clinical trials conducted between 1996 and 2015.
All patients in the study underwent radical surgery — the complete removal of the primary tumor — followed by adjuvant chemotherapy, a standard treatment designed to eliminate any lingering cancer cells. Each trial provided a median follow-up of at least six years, ensuring robust long-term data.
This enormous dataset allowed scientists to observe relapse patterns across time with unprecedented clarity. Rather than lumping all events together, the team separated true relapses — actual returns of the original cancer — from competing events like deaths from other causes or new primary tumors. This distinction was crucial, because these competing events can distort recurrence statistics, especially in older patients or those with other health conditions.
The Telling Pattern of Time
The findings were both illuminating and reassuring. The incidence of relapse peaked early, at about 6.4% between six and twelve months after surgery — a reminder of how critical close monitoring is during the first year of recovery. After this initial peak, the risk began to decline steadily.
By the sixth year, the probability of recurrence had dropped below 0.5%, and it remained below that threshold through the tenth year of observation. In other words, after six years of remaining disease-free, the chance of colon cancer returning was less than one in two hundred.
That statistical threshold — a relapse risk of under 0.5% — is what the researchers propose as a practical definition of cure for patients with stage II or stage III colon cancer.
The Hidden Influence of Competing Events
One of the most insightful aspects of the study was its careful separation of relapse from other outcomes. When deaths or new, unrelated tumors were counted as recurrences, the apparent risk of relapse became inflated — particularly among older patients, whose mortality risk from other causes was naturally higher.
By adjusting for these competing events, researchers were able to see a truer picture: not all post-treatment “events” are cancer relapses. This correction not only clarified the real risk of recurrence but also revealed subtle patterns among different subgroups.
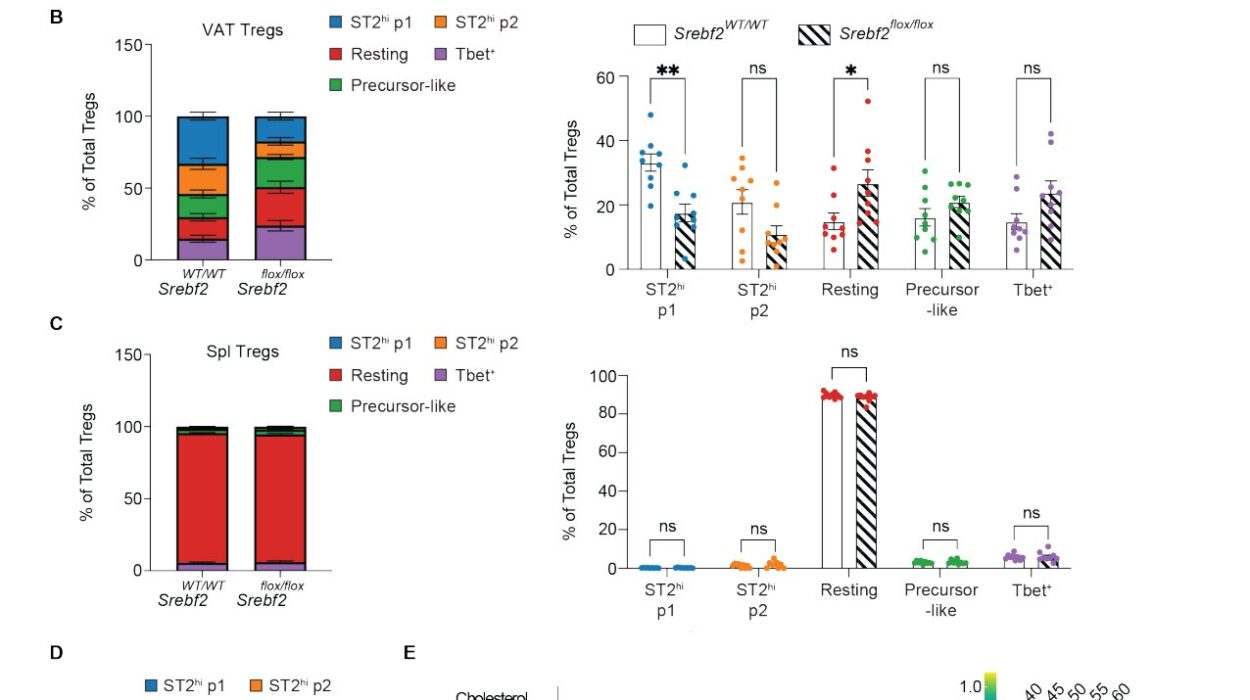
Age and Gender Patterns in Relapse Risk
Interestingly, the study found differences in recurrence risk depending on age and gender. Female patients showed a lower risk of recurrence when deaths were modeled as competing events, with a hazard ratio (HR) of 0.58, suggesting a potential biological or lifestyle factor offering women some protection.
In contrast, older patients faced higher event rates when death was treated as a competing factor. For example, those aged 40 years and older had a hazard ratio of 2.93 compared to younger patients, with similar patterns observed at age cutoffs of 50 and 70 years.
Despite these variations, the central finding held true across all groups: by six years post-surgery, recurrence risk consistently dropped below 0.5%, marking the turning point where doctors could reasonably declare a practical cure.
The Human Face Behind the Data
For patients, this research is not just a statistical milestone — it’s a deeply emotional one. The years following cancer surgery are filled with uncertainty. Every follow-up appointment is a mix of hope and fear. Each clear scan feels like a breath of relief, yet anxiety lingers in the background: What if it returns?
The new definition changes that emotional landscape. Knowing that, statistically, the chance of recurrence after six disease-free years is less than half a percent allows survivors to move forward — to celebrate birthdays, anniversaries, and ordinary days with a little less fear.
It also gives doctors a new, evidence-based tool to communicate hope more clearly. Instead of vague reassurance, they can now offer data-backed confidence: You’ve passed the six-year mark. Your risk of recurrence is now below 0.5%. You are, for all practical purposes, cured.
Why This Matters for the Medical Community
For clinicians and researchers, this study marks a major step toward a more refined understanding of colon cancer outcomes. It offers a practical, data-driven benchmark for defining cure — something that has long been elusive in oncology.
By separating true relapses from unrelated events, the study provides a cleaner measure of long-term success. This clarity can guide how long patients are monitored, how follow-up tests are scheduled, and how health systems allocate resources for surveillance.
Prolonged monitoring can be stressful and costly, and unnecessary follow-up tests can add to a patient’s emotional and financial burden. By establishing six years as a meaningful milestone of safety, oncologists can now personalize follow-up care more intelligently — reducing excessive surveillance while maintaining confidence in long-term outcomes.
The Scale of the Findings
Across the study population, 9,587 patients — or about 27.2% of the cohort — experienced local or distant recurrences during follow-up. This proportion highlights both the seriousness of colon cancer and the effectiveness of modern treatments. The vast majority of patients, especially those who remain disease-free for the first few years, now have an excellent chance of long-term survival.
Moreover, the study’s massive sample size and inclusion of data from 15 international clinical trials lend enormous weight to its conclusions. By harmonizing findings across decades and diverse patient populations, the researchers created a global snapshot of what colon cancer outcomes truly look like today.
Toward a New Definition of Cure
The authors conclude that when colon cancer relapse risk falls below 0.5% at six years, it can be considered a practical definition of cure for patients with stage II or III disease.
This may seem like a small statistical nuance, but its implications are profound. It gives structure to survivorship. It tells patients and families, with confidence, This is the moment when you can exhale.
It also challenges the way we think about cancer follow-up care. Instead of treating survival as an indefinite waiting game, we can now mark milestones along the journey — moments that recognize healing not just in the body, but in the mind and spirit.
Looking Ahead: A Future of Hope and Clarity
The collaboration between IRCCS Ospedale Policlinico San Martino, Mayo Clinic, and other leading institutions represents the best of global science — rigorous, compassionate, and deeply human. Together, they have turned decades of fragmented data into a single, hopeful message: Cure is not just possible. It can be defined.
This doesn’t mean every case will follow the same trajectory — each patient’s journey is unique. But it does mean that for the majority of those who make it six years cancer-free after surgery and chemotherapy, the shadow of recurrence has finally lifted.
For patients, doctors, and families alike, that realization carries immense emotional power. It’s the moment a survivor can finally look forward instead of back. It’s the point where statistics transform into hope.
The Quiet Power of Science
In the end, this study is more than a set of numbers; it is a testament to what science can do when guided by empathy. Behind every data point is a person — someone who endured diagnosis, surgery, chemotherapy, and years of uncertainty.
By defining what it means to be cured, the research honors those journeys. It provides answers where once there were only questions. And perhaps most importantly, it helps turn survival into something even greater: peace.
For countless colon cancer survivors around the world, six years is now more than a measure of time. It’s a milestone of life reclaimed — the moment science finally says, You are free.
More information: Alessandro Pastorino et al, The Definition of Cure in Colon Cancer, JAMA Oncology (2025). DOI: 10.1001/jamaoncol.2025.3760