In the early 1980s, cancer treatment looked very different from today. Chemotherapy and radiation were the main options, often with devastating side effects and uncertain outcomes. But in 1984, history was made when Linda Taylor, a 33-year-old woman facing advanced skin cancer, became the first patient ever cured through immunotherapy.
Her physician, Dr. Stephen Rosenberg of the National Cancer Institute in Bethesda, Maryland, believed that the body’s own immune system held untapped potential against cancer. He treated Taylor with interleukin-2 (IL-2), a molecule that rallies immune cells into battle. Against all odds, her tumors vanished. What was once seen as impossible—using the immune system to defeat cancer—suddenly became reality.
Taylor’s story marked the dawn of immunotherapy, offering hope to millions worldwide. IL-2 would go on to become the first immunotherapy approved by the U.S. Food and Drug Administration (FDA). Yet even as it opened doors, it came with heavy costs: harsh side effects and unpredictable responses that limited its use.
Now, nearly four decades later, researchers are pushing immunotherapy into a new era—one where treatments are not only powerful but also safer and smarter.
The Problem with the First Generation
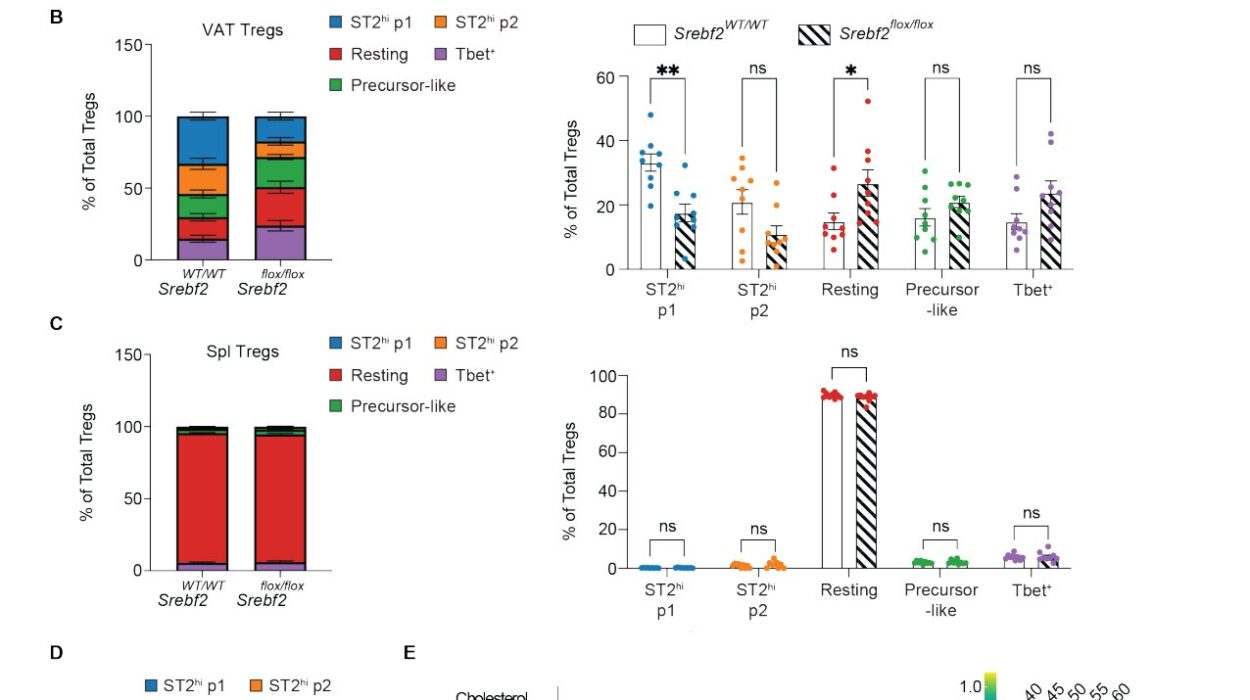
IL-2 was revolutionary, but it was also blunt. It activated many types of immune cells indiscriminately, including regulatory T cells, which suppress rather than boost the immune response. That meant IL-2 could sometimes work against itself, energizing the very cells that put brakes on tumor-fighting forces.
Even when it worked as intended, IL-2 therapy often came with dangerous side effects, such as extreme inflammation and organ damage. It was like unleashing a storm when what patients really needed was a focused strike.
To refine this approach, scientists began designing improved IL-2 variants—molecules re-engineered to specifically stimulate the immune cells most effective at killing tumors while avoiding regulatory cells. These second-generation IL-2 therapies promised greater precision and fewer side effects, but researchers still wondered: could they be combined with other strategies to unlock even more potent results?
A Fusion of Two Strategies
The answer may lie in a remarkable new molecule developed by Roche and tested by researchers at the University of Basel and University Hospital Basel. This “fusion protein” combines two powerful immunotherapy tactics into one elegant treatment.
On one side of the molecule is a modified IL-2 variant, called IL-2v, engineered to target the tumor-killing immune cells without activating the suppressive ones. On the other side is an antibody designed to bind to PD-1, a receptor on immune cells. Cancer cells exploit PD-1 by sending out a “do not attack” signal, effectively shutting down the immune response. Blocking this pathway—an approach known as checkpoint inhibition—has already proven life-saving for many cancer patients.
By fusing these two components, the therapy acts as both a guide and an activator. The antibody directs IL-2v to the very immune cells within the tumor, ensuring the right soldiers get energized. At the same time, it blocks PD-1, removing the brakes that cancers use to defend themselves.
The result is a two-pronged assault: immune cells are both freed from suppression and supercharged to attack.
Awakening the Immune Army
The impact of this dual approach was revealed in a study published in Science Translational Medicine by a team led by Professor Alfred Zippelius from the Department of Biomedicine in Basel.
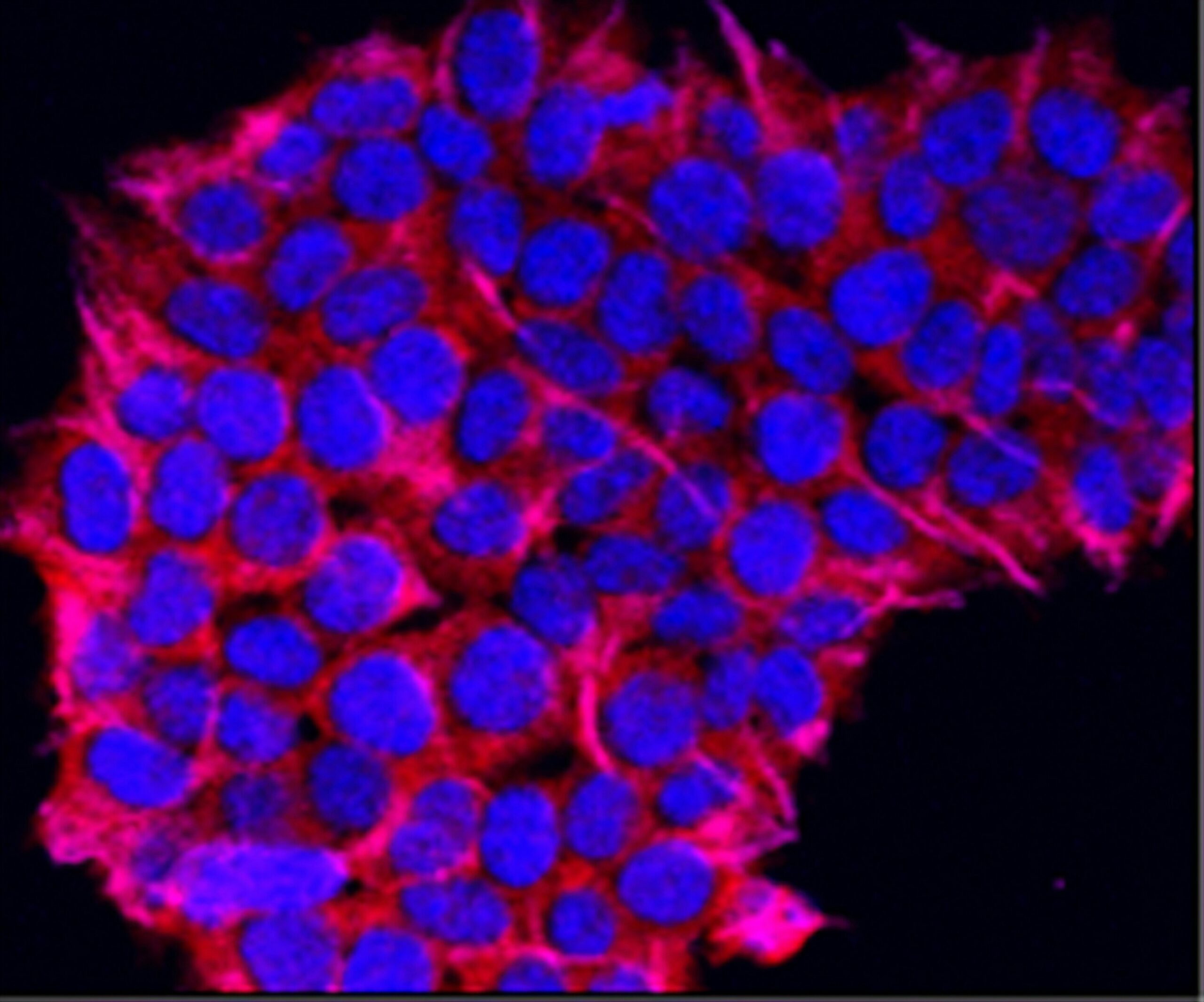
Working with immune and cancer cells from lung cancer patients, the researchers found that the fusion protein selectively reactivated immune cells that had grown “exhausted” from years of battling the tumor environment. These cells, previously dormant and ineffective, were brought back to life, regaining their ability to target and destroy cancer cells.
Equally important, the molecule avoided stimulating regulatory T cells, meaning it sidestepped one of the major pitfalls of earlier IL-2 therapies. The therapy not only amplified the immune response but also sharpened its focus, turning a broad and sometimes chaotic system into a precise weapon.
“The tumor normally restricts the immune system, but the fusion molecule overcomes this inhibition and additionally activates the immune cells,” explained Dr. Clara Serger, co-first author of the study.
From Lab to Patients
The research in Basel is more than a proof of concept. The fusion protein is already being tested in a phase I clinical trial led by Roche, bringing it one step closer to patients. These early studies will determine safety, dosage, and the first signals of effectiveness in humans.
While it is still early days, the approach embodies a powerful shift in cancer medicine: treatments that are not just stronger but smarter, combining different strategies into a single, unified therapy. If successful, it could reduce side effects, enhance efficiency, and open new doors for patients who have run out of options with existing therapies.
A Future Shaped by Immunotherapy
The journey from Linda Taylor’s groundbreaking cure in 1984 to today’s sophisticated fusion proteins illustrates just how far cancer immunotherapy has come. What began as a radical idea—turning the body’s immune system against cancer—has become one of the most promising frontiers in modern medicine.
The fusion of IL-2v with PD-1 blockade is more than a technical innovation. It represents a vision of cancer therapy that learns from past struggles, refines old tools, and boldly combines them to create something new. By awakening immune cells, guiding them directly to the tumor, and releasing the restraints that cancers exploit, researchers are giving the body its best chance to win.
For patients facing diagnoses that once felt hopeless, this science carries not just knowledge but hope—the hope of safer, stronger treatments and the dream of cures once thought impossible.
The story of immunotherapy is still being written. And with each chapter, it becomes clearer: the immune system, when guided by human ingenuity, may be the most powerful ally in the fight against cancer.
More information: PD1-targeted cis-delivery of an IL-2 variant induces a multifaceted anti-tumoral T cell response in human lung cancer, Science Translational Medicine (2025). DOI: 10.1126/scitranslmed.adr3718