Deep in the folds of your abdomen lies a quiet but essential organ—the pancreas. Most people rarely think about it until something goes wrong, yet it plays a central role in life itself. The pancreas is a dual-function organ: it produces digestive enzymes that break down food, and it regulates blood sugar through hormones like insulin and glucagon. It works silently, tirelessly, behind the scenes.
But when the pancreas becomes inflamed, this vital organ can turn from friend to foe. That inflammation is called pancreatitis. Unlike some conditions that creep in gradually, pancreatitis can appear suddenly with searing abdominal pain, or it can simmer slowly over years, eroding health silently. Either way, its impact on the body can be devastating if left untreated.
To truly grasp pancreatitis, we must explore its causes, its symptoms, the science behind its diagnosis, and the treatments that can restore balance—or, in severe cases, save lives.
What is Pancreatitis?
Pancreatitis is the inflammation of the pancreas, a condition that disrupts its normal function and can damage surrounding tissues. When functioning normally, the pancreas secretes digestive enzymes in an inactive form, which only activate once they reach the small intestine. In pancreatitis, these enzymes activate prematurely within the pancreas itself, leading to a self-destructive process—essentially, the pancreas begins to digest itself.
There are two primary forms:
- Acute pancreatitis: Sudden inflammation that may resolve within days if treated properly but can also become life-threatening.
- Chronic pancreatitis: A long-term inflammation that leads to permanent structural damage, scarring, and loss of function.
Though different in progression, both forms share one devastating truth: they interfere with the body’s ability to digest food and regulate blood sugar, two processes essential for survival.
Causes of Pancreatitis
The causes of pancreatitis are diverse, but they all involve something that triggers pancreatic inflammation or premature enzyme activation.
Gallstones
Gallstones are the most common cause of acute pancreatitis. These small, hardened deposits form in the gallbladder and can travel into the bile duct, blocking the flow of pancreatic enzymes. With no outlet, the enzymes build up and activate inside the pancreas, sparking inflammation.
Alcohol Use
Chronic alcohol consumption is another leading cause, especially for chronic pancreatitis. Alcohol alters the secretion of pancreatic enzymes and can increase the sensitivity of pancreatic cells to injury. Over time, repeated alcohol-induced damage creates scarring, calcification, and irreversible damage.
High Triglycerides
Severely elevated triglyceride levels in the blood—often above 1,000 mg/dL—can lead to acute pancreatitis. Though less common, this cause is particularly dangerous and requires both immediate and long-term management of lipid levels.
Genetic Factors
Certain inherited conditions, such as mutations in the PRSS1, SPINK1, or CFTR genes, predispose individuals to recurrent or chronic pancreatitis. These genetic variants affect enzyme regulation or fluid balance within the pancreas.
Medications and Toxins
Some drugs can trigger pancreatitis as a rare side effect. Common culprits include certain antibiotics, chemotherapy agents, diuretics, and immune-suppressing drugs. Environmental toxins and even venom from specific animals (like scorpions) have also been reported in rare cases.
Trauma or Surgery
Blunt abdominal trauma, accidents, or surgical interventions involving the pancreas or biliary system can physically damage the organ and provoke inflammation.
Other Causes
Autoimmune conditions, infections, and metabolic disorders (like hypercalcemia) can also lead to pancreatitis. In some cases, no clear cause is ever found, and the condition is labeled idiopathic pancreatitis.
Symptoms of Pancreatitis
The symptoms of pancreatitis depend on whether the condition is acute or chronic, but abdominal pain is the hallmark in both.
Acute Pancreatitis
The pain of acute pancreatitis is often sudden, severe, and felt in the upper abdomen. It may radiate to the back and worsen after eating, especially fatty meals. Alongside pain, patients may experience:
- Nausea and vomiting
- Fever and chills
- A swollen or tender abdomen
- Rapid pulse
- Low blood pressure in severe cases
The pain can be so intense that patients cannot sit still or lie comfortably, often curling forward to try to find relief.
Chronic Pancreatitis
Chronic pancreatitis produces a different pattern. Pain may be persistent but less severe than in acute cases, sometimes becoming dull over time. More concerning are the long-term consequences:
- Malabsorption of nutrients, leading to weight loss
- Greasy, foul-smelling stools (steatorrhea) due to undigested fat
- Diabetes, as insulin-producing cells become damaged
- Fatigue, weakness, and malnutrition
The chronic form slowly erodes health, not always through excruciating pain, but through the gradual loss of pancreatic function.
Complications of Pancreatitis
Pancreatitis is not just an isolated inflammation—it can spark a cascade of complications, some immediate and life-threatening, others long-term and debilitating.
- Pseudocysts: Fluid-filled sacs that can rupture or become infected.
- Necrosis: Death of pancreatic tissue, sometimes requiring surgery.
- Infections: Pancreatic infection can be fatal if untreated.
- Systemic inflammation: Severe pancreatitis can trigger widespread organ failure, including lungs, kidneys, and heart.
- Diabetes: Long-term damage often impairs insulin production.
- Malnutrition: With enzyme loss, the body struggles to absorb nutrients even if food intake is adequate.
Diagnosis of Pancreatitis
Diagnosing pancreatitis requires a combination of clinical evaluation, laboratory tests, and imaging.
Blood Tests
The two hallmark blood markers are amylase and lipase, enzymes produced by the pancreas. In acute pancreatitis, these levels rise dramatically—lipase being more specific to pancreatic injury. Additional tests may check liver function, blood sugar, triglycerides, and calcium.
Imaging
- Ultrasound is often the first imaging test to detect gallstones or blockages.
- CT scans provide detailed views of pancreatic inflammation, necrosis, or complications.
- MRI and MRCP (Magnetic Resonance Cholangiopancreatography) can reveal ductal blockages or subtle changes.
- Endoscopic ultrasound (EUS) offers high-resolution imaging and sometimes guided biopsies.
Diagnostic Criteria
Doctors typically confirm acute pancreatitis if two of three criteria are met:
- Characteristic abdominal pain.
- Elevated serum amylase or lipase levels (typically three times above normal).
- Imaging evidence of pancreatic inflammation.
Chronic pancreatitis is diagnosed through a combination of symptoms, imaging (showing scarring, calcifications, or duct changes), and functional testing of pancreatic enzymes.
Treatment of Pancreatitis
Treating pancreatitis depends on whether it is acute or chronic, but the goals remain the same: relieve pain, reduce inflammation, address underlying causes, and prevent complications.
Treatment of Acute Pancreatitis
Most cases require hospitalization. Initial management often involves:
- Fasting (NPO status): Patients avoid eating or drinking to rest the pancreas. Nutrition may be provided intravenously.
- IV fluids: Aggressive hydration helps prevent complications like kidney failure.
- Pain management: Strong pain relievers are often required.
- Monitoring: Close observation for organ failure, infection, or necrosis.
If gallstones are the cause, procedures like ERCP (Endoscopic Retrograde Cholangiopancreatography) may remove the obstruction. In some cases, gallbladder removal surgery follows to prevent recurrence.
Treatment of Chronic Pancreatitis
Chronic cases focus on managing symptoms and preserving function:
- Pancreatic enzyme supplements: To aid digestion and reduce malabsorption.
- Dietary modifications: Low-fat meals, smaller portions, and avoidance of alcohol.
- Pain management: Medications, nerve blocks, or surgical options may be used.
- Insulin therapy: For those who develop diabetes.
- Lifestyle interventions: Complete abstinence from alcohol and smoking cessation are crucial.
In severe cases, surgery may be necessary to drain pseudocysts, remove diseased tissue, or relieve ductal blockages.
Living with Pancreatitis
For many, pancreatitis is not just a medical condition but a life-changing experience. Acute attacks can be frightening and debilitating, while chronic pancreatitis can transform eating and living into constant challenges. Emotional support, counseling, and patient education are as important as medical treatment.
Patients often describe the loss of freedom to eat without fear, the struggle of constant fatigue, or the frustration of pain management. Yet many also find resilience, adopting healthier lifestyles, relying on support networks, and learning to listen to their bodies in ways they never had before.
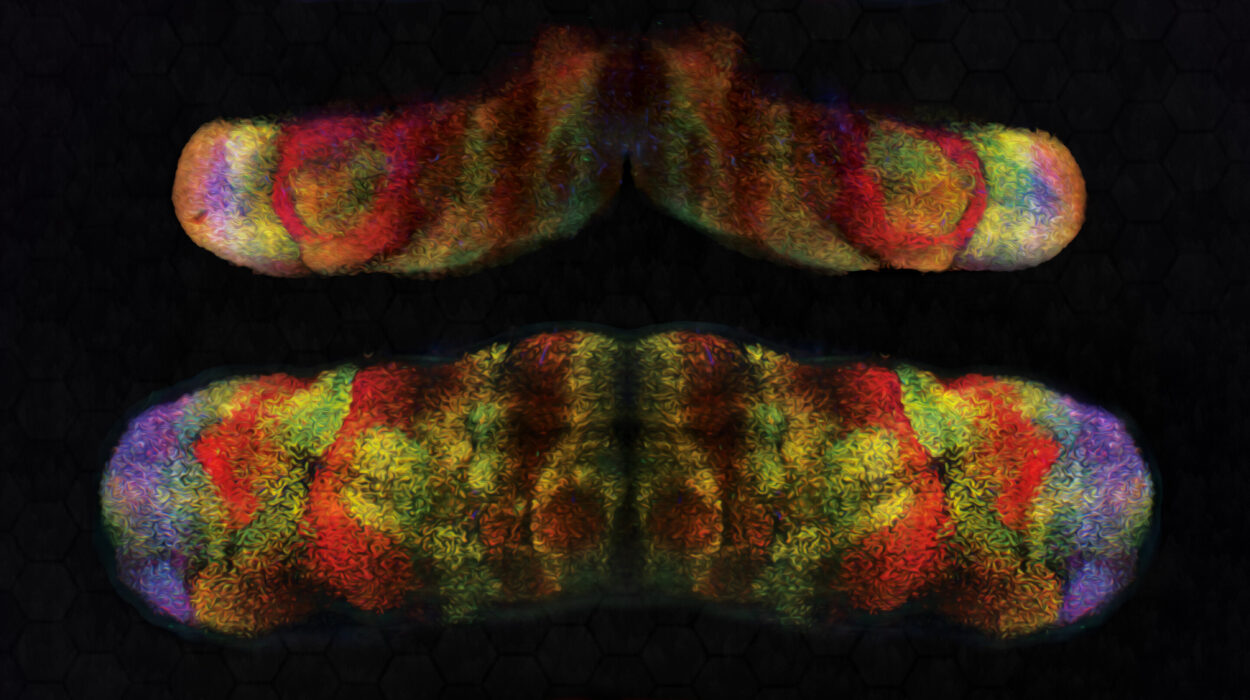
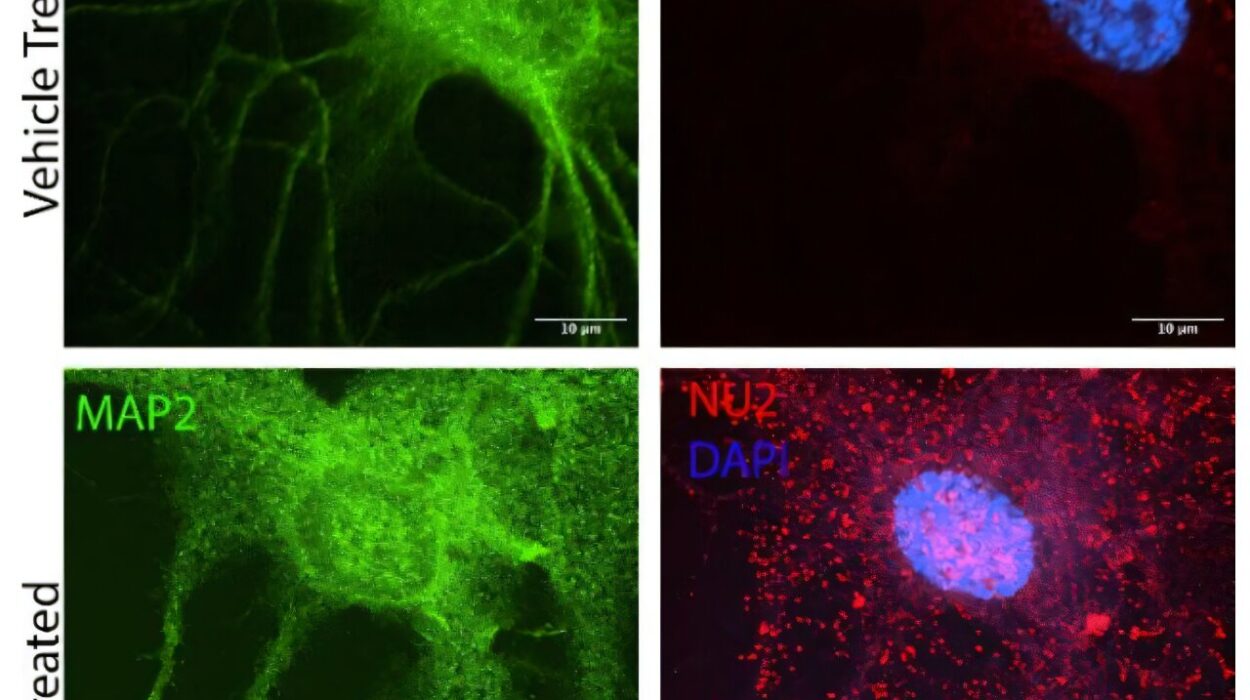
Research and Future Directions
Ongoing research continues to uncover new insights into pancreatitis. Advances in genetics are helping identify individuals at higher risk, while new imaging and biomarker tools aim to detect inflammation earlier. Experimental therapies are exploring how to block premature enzyme activation or reduce pancreatic scarring.
Stem cell research and regenerative medicine may one day offer hope for repairing damaged pancreatic tissue. Meanwhile, public health efforts target prevention by addressing alcohol abuse, obesity, and metabolic disorders that fuel the condition.
Conclusion: Reclaiming Balance
The pancreas may be hidden, but its importance is undeniable. Pancreatitis, whether sudden or chronic, is a reminder of how fragile this balance can be. Understanding its causes, recognizing its symptoms, and seeking timely diagnosis and treatment are essential for survival and recovery.
But beyond the science, pancreatitis teaches us about resilience. It calls for patience, discipline, and adaptation. It asks us to treat our bodies with care—through mindful eating, moderation, and respect for the hidden organs that sustain us.
Health is never guaranteed, but with awareness and proper medical care, even a condition as daunting as pancreatitis can be managed, and life, though altered, can still be lived with strength and hope.