Leukemia is not just a disease of the blood; it is a story of how the body’s most vital system for carrying life-giving oxygen, fighting infections, and sustaining balance becomes disrupted at its very core. To the person receiving the diagnosis, the word “leukemia” often strikes like thunder—sudden, overwhelming, and frightening. But behind the fear lies a deep scientific truth: leukemia is both one of the most studied cancers and one where remarkable progress has been made in understanding, treatment, and survival.
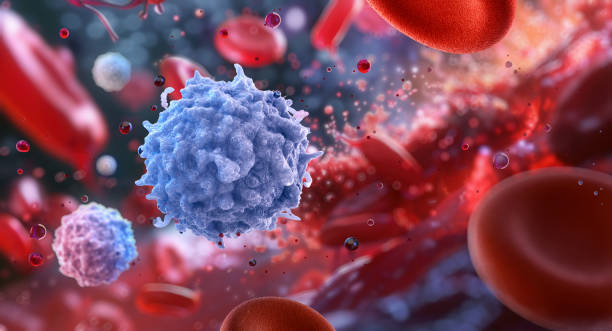
Health is built on balance, and nowhere is this more apparent than in the blood. The blood is not just a red liquid flowing through our veins; it is a living tissue, composed of billions of specialized cells, each performing unique and essential roles. When the balance of these cells is disturbed—when immature, abnormal white blood cells grow uncontrollably—it leads to leukemia.
To understand leukemia fully, we must explore its causes, recognize its symptoms, learn how doctors diagnose it, and uncover the modern therapies that give hope to millions worldwide.
What is Leukemia?
Leukemia is a type of cancer that originates in the bone marrow, the soft, spongy tissue inside bones where blood cells are produced. In healthy individuals, bone marrow produces three major types of blood cells:
- Red blood cells, which carry oxygen.
- White blood cells, which fight infections.
- Platelets, which help blood clot and prevent excessive bleeding.
In leukemia, something goes wrong in the production of white blood cells. Instead of producing mature, functional cells, the bone marrow churns out large numbers of abnormal, immature white blood cells known as blasts. These abnormal cells do not fight infection properly, yet they multiply rapidly and crowd out healthy blood cells.
This imbalance has devastating consequences: oxygen delivery falters, clotting mechanisms fail, and the immune system becomes both overactive and ineffective. The body becomes weak, prone to infections, and vulnerable to bleeding.
Leukemia is not a single disease but a group of related cancers. Its subtypes vary by speed of progression (acute or chronic) and by the type of blood cell affected (lymphoid or myeloid). These categories lead to the four major types:
- Acute lymphoblastic leukemia (ALL)
- Acute myeloid leukemia (AML)
- Chronic lymphocytic leukemia (CLL)
- Chronic myeloid leukemia (CML)
Each form has its own story—different causes, age groups, progression patterns, and treatment strategies.
Causes of Leukemia: Why Does It Happen?
The question at the heart of leukemia is simple yet profound: why do normal cells suddenly become cancerous? Science has provided many answers, but not yet the complete picture.
At the cellular level, leukemia begins with genetic mutations—changes in DNA that alter how blood cells grow and divide. These mutations can activate oncogenes (genes that drive cell growth) or deactivate tumor suppressor genes (which normally keep cell division under control). The result is uncontrolled proliferation.
But what triggers these genetic mistakes? Research suggests a complex interplay of factors:
Genetic Predisposition
Some people are born with an inherited risk. Genetic syndromes like Down syndrome or Li-Fraumeni syndrome increase susceptibility to leukemia. Similarly, having close relatives with leukemia slightly raises one’s risk, although most cases do not have a strong hereditary link.
Environmental Exposures
Certain chemicals and radiation exposures are known contributors. For instance, long-term exposure to benzene (found in cigarette smoke, gasoline, and some industrial settings) significantly raises leukemia risk. Survivors of atomic bomb radiation or patients treated with high-dose radiation therapy also face higher risks.
Prior Cancer Treatment
Ironically, treatments designed to cure other cancers—like chemotherapy and radiation—can sometimes damage DNA in healthy bone marrow cells, leading to secondary leukemia years later.
Viral Infections
Certain viruses, such as the human T-cell leukemia virus type 1 (HTLV-1), are linked to rare forms of leukemia. While not common globally, these connections highlight the role of infectious agents in altering immune and genetic functions.
Lifestyle and Unknown Factors
Unlike lung cancer or heart disease, lifestyle choices like diet and exercise play less direct roles in leukemia risk. However, smoking is known to increase the likelihood of certain types, particularly AML. For many cases, the exact trigger remains elusive—leukemia often arises from a mosaic of chance mutations, inherited tendencies, and environmental influences.
Symptoms of Leukemia: The Body’s Distress Signals
Leukemia symptoms often appear subtly at first, easily mistaken for common illnesses like the flu. This is because many symptoms result from the lack of healthy blood cells rather than the presence of abnormal ones.
The most common early signs include:
- Fatigue and weakness due to anemia (low red blood cell count).
- Frequent infections because abnormal white blood cells cannot protect the body.
- Unexplained bruising or bleeding, such as nosebleeds, bleeding gums, or tiny red spots on the skin (petechiae), caused by low platelets.
- Fever and night sweats, reflecting the body’s immune and inflammatory response.
- Bone or joint pain, as overcrowded bone marrow becomes pressured.
- Swollen lymph nodes, liver, or spleen, from the spread of abnormal cells.
- Unintentional weight loss and loss of appetite, common in many cancers.
The intensity and speed of symptom development vary depending on the type of leukemia.
- In acute leukemia, symptoms appear suddenly and worsen within weeks. Immediate medical attention is required.
- In chronic leukemia, symptoms may be absent for months or even years, with diagnosis often occurring during routine blood tests.
These symptoms reflect the silent struggle happening inside: the marrow crowded with malignant cells, the bloodstream unable to carry oxygen efficiently, and the immune system failing to protect its host.
Diagnosis: Uncovering the Hidden Disease
Diagnosing leukemia requires a careful combination of clinical evaluation, laboratory testing, and imaging studies. The process is both scientific and deeply human, as doctors work to uncover the cause of a patient’s suffering while guiding them through uncertainty.
Medical History and Physical Exam
The journey begins with a detailed history—recording symptoms, exposures, family history, and overall health. A physical exam may reveal swollen lymph nodes, an enlarged spleen, or signs of anemia and bleeding.
Blood Tests
A complete blood count (CBC) often provides the first clue. Abnormal numbers of white blood cells, red blood cells, or platelets point toward leukemia. The presence of immature blasts in the blood is particularly telling.
Bone Marrow Examination
The definitive test for leukemia is a bone marrow aspiration and biopsy. Doctors insert a needle into the hip bone to collect marrow samples, which are then analyzed under a microscope. This reveals the proportion of abnormal blasts and their specific characteristics.
Cytogenetic and Molecular Testing
Modern medicine dives deeper into the DNA of cancer cells. Chromosomal abnormalities, such as the Philadelphia chromosome in chronic myeloid leukemia, provide not only diagnostic confirmation but also guidance for targeted treatments.
Imaging Studies
X-rays, CT scans, or ultrasounds may be used to check for organ involvement. While not always necessary for diagnosis, they help assess the disease’s spread and complications.
Diagnosis is both a science and an emotional experience. For patients, hearing the words “you have leukemia” is life-changing. But with diagnosis comes clarity, and clarity is the first step toward treatment.
Treatment of Leukemia: Fighting Back
The treatment of leukemia has evolved dramatically over the past century. Once considered almost uniformly fatal, many forms of leukemia are now highly treatable—and in some cases, curable. Treatment strategies depend on the type of leukemia, the patient’s age and health, and genetic features of the cancer cells.
Chemotherapy
Chemotherapy remains the cornerstone for many leukemias, particularly acute forms. These drugs target rapidly dividing cells, killing leukemia blasts while also affecting normal cells. Treatment often occurs in phases: induction (to achieve remission), consolidation (to destroy hidden cells), and maintenance (to prevent relapse).
Targeted Therapy
One of the greatest revolutions in cancer treatment has been targeted therapy. Unlike traditional chemotherapy, these drugs specifically attack cancer cells based on their genetic or molecular features.
- Imatinib (Gleevec), a tyrosine kinase inhibitor, transformed chronic myeloid leukemia from a fatal disease into a manageable condition for many patients.
- Other targeted drugs now exist for specific mutations, expanding hope for personalized treatment.
Immunotherapy
Harnessing the immune system has opened new frontiers. Immunotherapies include:
- Monoclonal antibodies, which mark leukemia cells for destruction.
- CAR T-cell therapy, where a patient’s own T-cells are genetically engineered to recognize and kill leukemia cells. This therapy has shown remarkable success in relapsed ALL, particularly in children.
Radiation Therapy
Though less commonly used than in solid tumors, radiation can target leukemia cells in specific areas, such as the brain or spleen.
Stem Cell Transplantation
For certain aggressive or relapsed leukemias, hematopoietic stem cell transplantation (also known as bone marrow transplant) offers the possibility of cure. In this procedure, diseased marrow is destroyed with high-dose therapy, and healthy donor stem cells are infused to rebuild the blood system.
Supportive Care
Beyond directly targeting leukemia, supportive care is vital. This includes antibiotics to prevent infection, transfusions for anemia or low platelets, and nutritional and psychological support to help patients withstand treatment.
The Human Side of Leukemia
While science focuses on cells, mutations, and treatments, leukemia is also a profoundly human experience. Patients and families face fear, uncertainty, and disruption of normal life. Fatigue, hospital stays, and side effects are not just medical issues—they are emotional and social challenges.
Psychological support, counseling, and community networks play essential roles in holistic treatment. Survivors often speak of the resilience they discover, the deeper appreciation of life, and the bonds formed with caregivers and loved ones. These stories remind us that health is more than a laboratory result; it is a lived experience.
Progress and Hope
The story of leukemia is also a story of medical triumph. In the 1960s, childhood acute lymphoblastic leukemia was almost universally fatal. Today, thanks to decades of research, the survival rate for children with ALL exceeds 85% in many countries. Drugs like imatinib have turned once-deadly diseases into chronic, manageable conditions.
Ongoing research continues to unlock new possibilities—genome sequencing to predict outcomes, new immunotherapies, and strategies to reduce side effects while increasing survival. The horizon of leukemia treatment is filled with promise.
Living with Leukemia
For many, living with leukemia does not end with treatment. Survivors may face long-term side effects, such as fatigue, fertility issues, or increased risks of other cancers. Regular follow-up care is essential. Yet many people go on to live full, active lives, pursuing careers, raising families, and even running marathons after leukemia.
The key is ongoing vigilance combined with a commitment to well-being—healthy lifestyle choices, emotional resilience, and strong medical partnerships.
Conclusion: From Darkness to Light
Leukemia is a disease born in the blood, but its impact radiates through the whole person—body, mind, and spirit. Its causes are complex, its symptoms subtle but devastating, its diagnosis intricate, and its treatments challenging yet increasingly effective.
It is also a disease that reflects the very best of human progress. From despair to hope, from inevitable death to remarkable survival, the journey of leukemia research and treatment showcases how science, compassion, and perseverance can change lives.
To ask about leukemia is to ask about the fragility and strength of life itself. It reminds us that health is precious, that science is powerful, and that even in the darkest times, light can emerge.