Imagine waking up in the middle of the night, jolted by a searing, almost unbearable pain in your big toe. The joint is red, swollen, and so tender that even the lightest touch—a sheet brushing against it—feels like fire. This is not just ordinary discomfort. This is gout, one of the most ancient and notorious diseases known to humankind.
For centuries, gout has been called the “disease of kings” and the “rich man’s arthritis,” linked to feasts of red meat, rich sauces, and overflowing goblets of wine. Today, we know that gout is not limited to monarchs and nobles; it can affect anyone, regardless of social class. It is a condition that strikes suddenly, often without warning, and can return again and again, leaving behind lasting damage if untreated.
Gout is more than just a painful foot problem. It is a metabolic disorder, an inflammatory disease, and a condition that reveals much about how our lifestyle and biology intersect. To truly understand it, we must explore its causes, symptoms, diagnosis, and treatments—not in isolation but as part of the human story of health and disease.
What Exactly Is Gout?
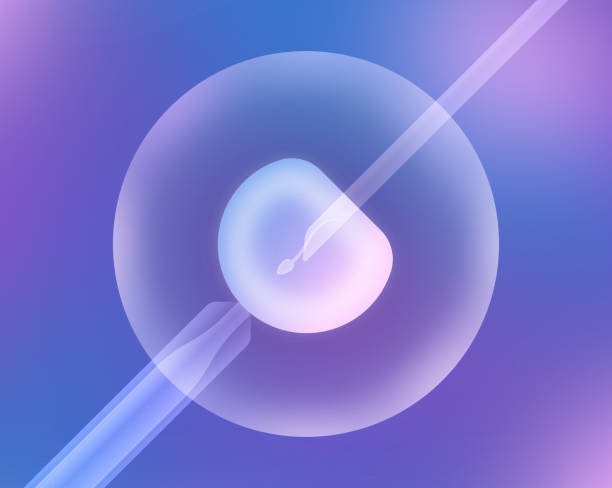
At its core, gout is a form of arthritis caused by excess uric acid in the body. Uric acid is a natural waste product created when our bodies break down purines—chemical compounds found in certain foods and also produced naturally by the body. Normally, uric acid dissolves in the blood, passes through the kidneys, and exits the body in urine.
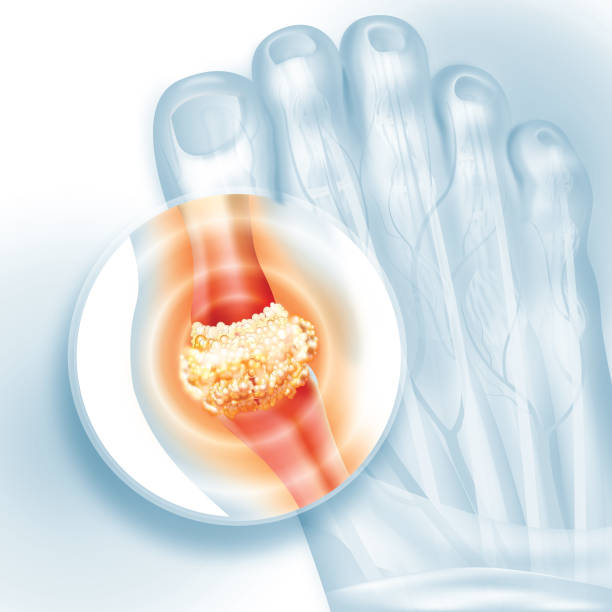
But when uric acid levels rise too high, either because the body produces too much or the kidneys cannot eliminate enough, it can form sharp, needle-like crystals. These crystals settle in the joints, particularly in cooler parts of the body such as the toes, ankles, or knees. The immune system sees these crystals as foreign invaders and mounts an inflammatory response. The result is a gout attack: intense pain, swelling, redness, and heat in the affected joint.
Gout is not just about occasional flare-ups. Over time, if left untreated, it can lead to chronic arthritis, permanent joint damage, and the formation of tophi—lumps of uric acid crystals under the skin. It can also be associated with other serious health conditions, including kidney disease, diabetes, and heart disease.
The Causes of Gout: Why Does It Happen?
The central cause of gout is hyperuricemia, a condition in which uric acid levels in the blood are abnormally high. But why does hyperuricemia occur? The answer lies in a combination of biology, lifestyle, and environment.
Purines and Uric Acid
Purines are found in many foods, especially organ meats, shellfish, red meat, and alcohol. When purines break down, uric acid is produced. If the balance tips toward excessive purine intake, uric acid can build up faster than the body can excrete it.
Genetic Factors
Some people are genetically predisposed to gout. If your parents or grandparents had it, your risk is higher. Genetics can affect how efficiently your kidneys process uric acid or how much uric acid your body produces.
Kidney Function
The kidneys play a crucial role in uric acid elimination. If they are impaired—whether due to chronic kidney disease, dehydration, or other medical issues—uric acid can accumulate in the bloodstream.
Diet and Lifestyle
While not the sole cause, diet plays a major role in gout flare-ups. Foods and drinks that are particularly gout-triggering include:
- Red meat and organ meats (liver, kidneys, sweetbreads)
- Shellfish and oily fish (anchovies, sardines, mussels)
- Alcohol, especially beer and spirits
- Sugary beverages, particularly those sweetened with fructose
Medical Conditions and Medications
Certain health conditions, such as obesity, diabetes, high blood pressure, and metabolic syndrome, increase the risk of gout. Medications such as diuretics, aspirin, and some chemotherapy drugs can also raise uric acid levels.
Environmental and Lifestyle Triggers
Stress, dehydration, sudden changes in diet, crash dieting, and even vigorous exercise can sometimes precipitate an attack. Gout often strikes when the body is slightly “off balance,” tipping the scales toward crystal formation.
Symptoms of Gout: More Than Just a Sore Joint
The hallmark of gout is the sudden onset of intense joint pain, often in the middle of the night or early morning. But the symptoms go beyond pain, and they unfold in distinct phases.
Acute Gout Attacks
During an attack, the affected joint—most commonly the big toe but sometimes the ankle, knee, wrist, or elbow—becomes:
- Excruciatingly painful, often described as throbbing, crushing, or burning
- Red or purplish, mimicking an infection
- Swollen, with skin stretched tight and shiny
- Hot to the touch, with inflammation radiating outward
An attack usually peaks within 24 hours and can last from a few days to a week. Without treatment, attacks may recur more frequently and affect more joints over time.
Intercritical Periods
Between attacks, there may be weeks, months, or even years of complete relief. However, crystals remain silently in the joints, and the disease is not gone—it is only resting.
Chronic Gout and Tophi
If gout is untreated, repeated attacks lead to chronic gout. The inflammation becomes persistent, causing joint stiffness, reduced mobility, and erosion of cartilage and bone. Tophi, which are visible deposits of uric acid crystals, can form under the skin on fingers, elbows, or toes, sometimes disfiguring the hands and feet.
Systemic Symptoms
In some cases, gout is accompanied by fever, chills, or malaise. Severe inflammation can trick the body into feeling like it is fighting an infection, adding to the distress of an attack.
Diagnosis: How Do Doctors Identify Gout?
Diagnosing gout requires more than just observing a painful joint. Many conditions, such as septic arthritis or pseudogout, can mimic its symptoms. A careful evaluation is essential.
Medical History and Physical Examination
Doctors first review symptoms, family history, and lifestyle factors. The classic description of a sudden attack of pain in the big toe is highly suggestive of gout, but further tests are needed for confirmation.
Laboratory Tests
The most definitive test is joint fluid analysis. A needle is inserted into the swollen joint to withdraw fluid, which is examined under a microscope. The presence of needle-shaped uric acid crystals confirms gout.
Blood tests can measure uric acid levels, but these are not always reliable, as levels may be normal during an attack. Still, persistently high uric acid supports the diagnosis.
Imaging
Ultrasound can detect uric acid crystal deposits in joints and soft tissues, while dual-energy CT scans provide even more precise visualization. X-rays may reveal joint damage in advanced gout but are less useful in early stages.
Treatment: Relieving Pain and Preventing Future Attacks
The treatment of gout focuses on two main goals:
- Relieving the immediate pain and inflammation of acute attacks.
- Preventing future attacks and complications by lowering uric acid levels.
Managing Acute Attacks
When a gout flare strikes, fast treatment is crucial to reduce suffering. Common approaches include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen, naproxen, or indomethacin are often the first line of defense, quickly reducing pain and swelling.
- Colchicine: An ancient drug derived from the autumn crocus, colchicine interrupts the inflammatory process triggered by crystals. It works best if taken soon after symptoms begin.
- Corticosteroids: If NSAIDs or colchicine are not suitable, steroids (oral or injected into the joint) can rapidly calm inflammation.
Long-Term Management: Lowering Uric Acid
Once the immediate crisis passes, the focus shifts to preventing future attacks by controlling uric acid.
- Lifestyle Changes: Adopting a balanced diet, reducing alcohol intake, drinking more water, and maintaining a healthy weight are foundational.
- Urate-Lowering Medications: Drugs such as allopurinol or febuxostat reduce uric acid production, while others like probenecid help the kidneys excrete more uric acid. These medications are usually taken for life, as stopping them often leads to relapse.
- Monitoring: Regular blood tests track uric acid levels, with the goal of keeping them low enough to prevent crystal formation.
Treating Complications
In advanced cases, tophi may need surgical removal if they impair joint function or cause infections. Kidney stones resulting from uric acid buildup may also require intervention.
Living With Gout: More Than Just Medication
Managing gout is not only about pills and prescriptions. It requires an active partnership between patient and healthcare provider, as well as thoughtful daily choices.
Dietary adjustments—favoring vegetables, whole grains, lean proteins, and low-fat dairy—can make a real difference. Hydration is vital, as water helps flush uric acid from the body. Gentle exercise strengthens joints and improves overall health, while avoiding overexertion during flares.
Emotional well-being is equally important. The sudden, unpredictable nature of gout attacks can cause anxiety and frustration. Support groups, counseling, and mindfulness practices may help patients cope with the emotional toll.
Gout and the Bigger Picture of Health
Gout does not exist in isolation. It often accompanies other serious conditions, including obesity, hypertension, kidney disease, and cardiovascular problems. For this reason, doctors view gout not just as a joint disease but as a marker of broader metabolic imbalance.
Treating gout, therefore, is also about treating the whole person—addressing lifestyle, managing coexisting conditions, and reducing overall risk of complications. In this way, gout can serve as a warning sign, prompting individuals to make changes that improve not only their joints but their entire health.
The Future of Gout Care
Research into gout is ongoing, aiming for better treatments and possibly even cures. Advances in genetics are shedding light on why some people are more prone to hyperuricemia, while new drugs are being developed to target uric acid metabolism with greater precision. Personalized medicine may one day allow doctors to tailor treatments based on an individual’s genetic profile and lifestyle.
At the same time, public health efforts are needed to raise awareness, reduce stigma, and ensure that effective treatments are accessible to all. Too often, gout is trivialized as merely a painful nuisance, when in fact it is a serious condition with life-altering consequences if ignored.
Conclusion: Gout as a Teacher
Gout may be an ancient disease, but it continues to teach us valuable lessons about the human body, lifestyle, and the importance of balance. It reminds us that what we eat and drink matters, that our genetic inheritance shapes our risks, and that health requires both personal responsibility and medical care.
For those who suffer from it, gout is more than a diagnosis—it is a challenge to live fully despite sudden and severe pain. Yet with proper treatment, lifestyle changes, and awareness, gout can be controlled, its attacks minimized, and its long-term damage prevented.
To understand gout is to understand not only a disease but also the delicate interplay of biology, environment, and choice that defines human health itself.