The human body is a marvel of adaptation, resilience, and beauty—but it is also incredibly vulnerable. Nowhere is that vulnerability more literal than in the skin, the body’s largest and most exposed organ. It wraps around us like armor, regulating temperature, fighting infections, and forming the frontline barrier between our inner lives and the outer world. Yet this very exposure makes it a battleground. And increasingly, that battlefield is scarred by a disease that too many dismiss as “just skin deep”: skin cancer.
Across sun-drenched beaches, city streets, rural farmlands, and suburban backyards, a silent crisis is spreading. Skin cancer is the most common cancer in the world, with millions of new cases diagnosed each year. It affects people of all backgrounds, ages, and skin tones. It doesn’t care whether you’re sunbathing or walking to work. And it’s far more serious than many assume. Though often treatable when caught early, skin cancer can be disfiguring, recurrent, and—when ignored or misunderstood—deadly.
To understand skin cancer is not just to understand a disease. It’s to confront how the modern world, our cultural values, and even our desire to feel beautiful or free can clash with biology. But more importantly, it’s to realize that we have the power to prevent it—and that power begins with knowledge, vigilance, and compassion.
Beneath the Surface: What Skin Cancer Really Is
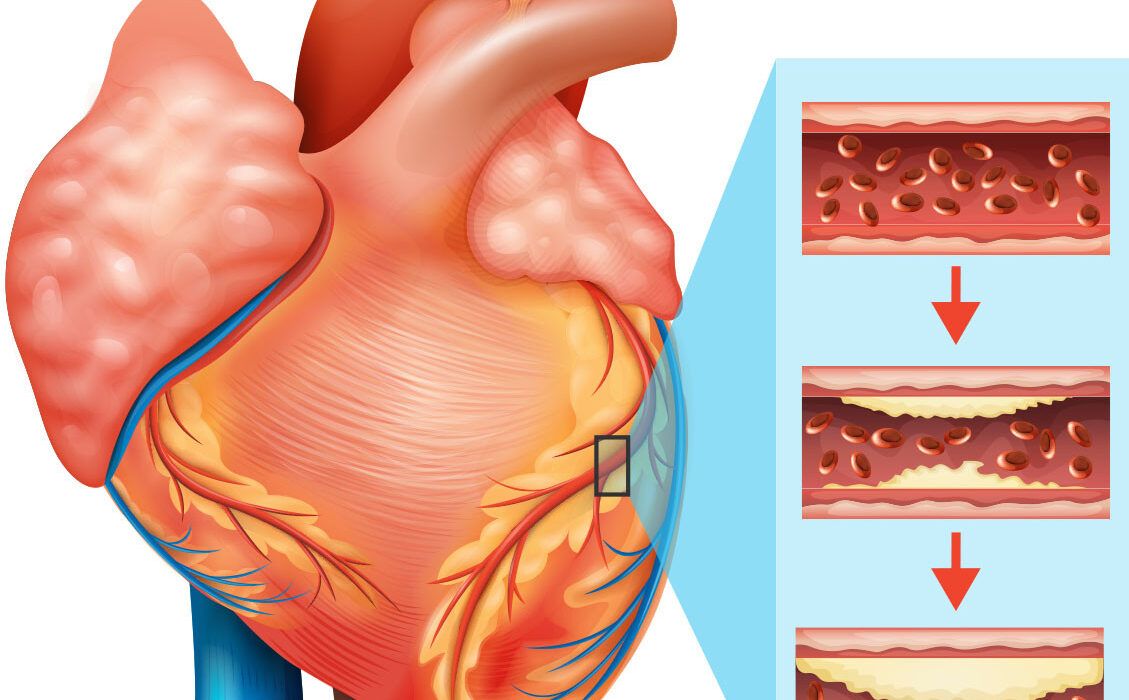
Skin cancer begins when abnormal cells in the skin grow uncontrollably. Normally, skin cells grow, divide, and die in a well-regulated cycle. But when the DNA inside a skin cell becomes damaged—often by ultraviolet (UV) radiation from the sun or artificial sources like tanning beds—that delicate system can break down. Damaged DNA can cause cells to mutate and multiply rapidly, forming tumors that may remain localized or invade deeper tissues and spread to other parts of the body.
There are three major types of skin cancer: basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. BCC and SCC are known as non-melanoma skin cancers and are the most common. Though rarely fatal, they can still be serious if left untreated. Melanoma, on the other hand, is far less common but dramatically more dangerous. It arises in melanocytes—the cells that produce pigment—and can spread rapidly if not caught early.
Each type behaves differently. Some grow slowly, others spread like wildfire. Some are clearly visible, while others lurk beneath the surface, masked by freckles or moles. And all of them begin the same way: with DNA damage.
The Sun’s Double-Edged Sword
The sun is both giver and taker of life. Its light nourishes the planet, boosts our mood, and helps our bodies produce vitamin D. But its rays also carry a hidden cost. Invisible to the eye but potent in effect, ultraviolet (UV) radiation is the single most significant risk factor for skin cancer.
UV radiation is divided into three types: UVA, UVB, and UVC. UVC is filtered by the Earth’s atmosphere and doesn’t reach us. But UVA and UVB reach the surface—and our skin. UVA rays penetrate deep into the dermis, aging the skin and contributing to wrinkles and DNA damage. UVB rays, while not as deep-reaching, are more energetic and responsible for sunburns. Both types of radiation can damage cellular DNA directly or generate reactive oxygen species that cause oxidative stress and genetic mutations.
The result? Over time, sun exposure creates a kind of molecular erosion. Cells accumulate mutations that may not be immediately obvious. Damage may linger silently for decades before a single cell crosses the tipping point and becomes cancerous.
This is why sun damage from youth often manifests in later years—and why childhood sunburns are especially dangerous. One blistering sunburn in adolescence can double your risk of developing melanoma later in life. It’s not just about today’s tan. It’s about a cellular debt that may one day come due.
Tanning Beds and the Business of Beauty
If UV exposure from the sun weren’t risky enough, the 20th century introduced a manufactured menace: tanning beds. Marketed as a safe and controlled way to bronze the skin, these devices use concentrated UVA and UVB radiation to simulate sun exposure. But far from being harmless, tanning beds are classified by the World Health Organization as Group 1 carcinogens—the same category as tobacco and asbestos.
Frequent tanning bed use before the age of 35 increases the risk of melanoma by up to 75%. And yet, millions of people, particularly teens and young adults, continue to use them. The reasons are complex. Western culture often associates tanned skin with beauty, health, and vitality. This aesthetic ideal, reinforced by media and fashion industries, creates pressure to seek a sun-kissed glow—regardless of the risks.
But beauty achieved through radiation is a dangerous illusion. While the tan may fade, the cellular damage it leaves behind does not. And unlike clothing or makeup, there’s no undoing the mutations once they take root in your DNA.
Genetics and the Uneven Lottery of Risk
Though UV exposure is the primary cause of skin cancer, not all skin is created equal when it comes to risk. Genetics play a significant role in determining vulnerability. People with fair skin, light hair, and light eyes produce less melanin—the pigment that provides some natural protection against UV damage. As a result, they burn more easily and are more prone to skin cancer.
But darker-skinned individuals are not immune. While melanin offers greater protection, it does not eliminate risk. In fact, when skin cancer occurs in people with darker skin tones, it is often diagnosed at later stages and can be more deadly. This is partly due to the misconception that darker skin cannot develop cancer, leading to delayed diagnosis and a lack of public awareness.
Family history also matters. People with a close relative who has had skin cancer are at higher risk, especially if they’ve inherited genetic mutations like those found in the CDKN2A or BRAF genes, both of which are associated with melanoma. Additionally, certain hereditary conditions like xeroderma pigmentosum, which impairs the body’s ability to repair UV-induced DNA damage, make sun exposure life-threatening.
Skin cancer is not an equal-opportunity disease. It is a lottery weighted by heritage, environment, and lifestyle—but it is never a fate sealed in stone. Knowledge and vigilance can tip the balance.
The Slow March of Symptoms
One of the most insidious aspects of skin cancer is its subtlety. It often begins not with pain or dramatic symptoms, but with a freckle that changes shape, a sore that won’t heal, or a rough patch mistaken for dry skin. Many people delay seeking help because the signs seem so minor—or because they’ve seen them on their skin for years.
Basal cell carcinoma often appears as a pearly bump, a reddish patch, or a flat lesion with a central indentation. Squamous cell carcinoma may manifest as a crusted or scaly area, sometimes mistaken for eczema or a wart. Melanoma, however, is the most visually deceptive. It can look like a mole, but with irregular borders, asymmetry, multiple colors, or a diameter larger than a pencil eraser. In some cases, it arises in parts of the body that rarely see the sun—under nails, in the eyes, or on the soles of the feet.
Doctors use the ABCDE rule—Asymmetry, Border irregularity, Color variation, Diameter, and Evolution—to help people spot potentially dangerous lesions. But the truth is, anything new, changing, or unusual on your skin warrants attention. When it comes to cancer, early detection is everything.
Diagnosis, Biopsy, and the Emotional Toll
When a suspicious lesion is found, a dermatologist will typically perform a biopsy, removing a small sample of tissue for microscopic analysis. For the patient, this moment is emotionally charged. Fear, denial, anxiety, and shame often swirl together. Many people blame themselves, wondering if they should have used more sunscreen or avoided that tanning salon in high school.
But blame is not helpful. Cancer doesn’t care about guilt. It requires action.
If cancer is confirmed, treatment options vary depending on the type, location, and stage. Surgery is the most common and effective approach for most skin cancers. In cases of melanoma that have spread, additional treatments like immunotherapy, targeted therapy, or radiation may be required.
Beyond the physical burden, there is the psychological impact. The visible nature of skin cancer means that scars, disfigurement, and changes in appearance are common. For many patients, especially those with facial lesions, the emotional recovery is as complex as the medical one. Support groups, counseling, and compassionate care are crucial parts of healing.
Protecting Yourself: Knowledge is Your Shield
Skin cancer is not an inevitable fate. It is largely preventable. The key lies not in paranoia, but in protection—habitual, thoughtful, daily protection. Avoiding peak sun hours, seeking shade, and wearing wide-brimmed hats, sunglasses, and protective clothing all help minimize risk. Sunscreen is essential. Dermatologists recommend a broad-spectrum (UVA/UVB) sunscreen with SPF 30 or higher, applied generously and frequently—especially after swimming or sweating.
But more than any product, the greatest tool is self-awareness. Monthly skin checks at home and annual full-body exams by a dermatologist can catch problems early. Photographing moles and spots over time can help track changes. And teaching children sun safety early can set them on a path to lifelong protection.
Technology is also lending a hand. Mobile apps and AI tools can now analyze skin lesions for potential abnormalities, aiding early detection—though nothing replaces the trained eye of a dermatologist.
Myths, Misconceptions, and the Danger of Complacency
Despite the science, myths persist. Some believe that tanning is healthy, or that sunscreen causes cancer, or that only old people need to worry. These misconceptions are not just wrong—they are dangerous. Tanning is never safe. Sunscreen has been rigorously tested and saves lives. And skin cancer does not discriminate by age.
Social media and misinformation have created echo chambers where fear of chemicals overrides the need for sun protection, and where anecdotes outweigh evidence. Fighting skin cancer means fighting misinformation too—through education, science, and empathy.
The Human Cost and the Stories Behind the Statistics
Every statistic hides a story. A young woman who loved the beach and ignored a growing mole. A construction worker who never wore a hat. A teenager who tanned before prom. A grandfather whose lesion was dismissed as a “liver spot.” These are not abstract numbers. They are lives upended, families shaken, futures rewritten.
Yet for all the tragedy, there is hope. Millions of survivors walk among us. Advances in early detection, surgical techniques, and immunotherapy have turned the tide. Melanoma, once a death sentence, is now treatable in many advanced cases. But prevention will always be the first and best line of defense.
A Future in the Shade
The future of skin cancer prevention lies not in hiding from the sun, but in learning to live with it wisely. Urban planning that includes shaded public spaces, school policies that encourage sun safety, and fashion that makes protective clothing stylish are all part of the solution. So is legislation. Many countries and states have begun banning tanning beds for minors, and some have instituted public health campaigns as robust as those against smoking.
Education will be key. The more we understand the invisible threat of UV radiation, the more we can protect future generations from the pain of unnecessary illness.
Conclusion: The Skin We’re In
Skin cancer is a disease of exposure—not just to sunlight, but to culture, choices, and chance. It teaches us that beauty can be a trap, that health is a daily act, and that our bodies remember more than we think. But it also shows us how resilient we are. With knowledge, care, and vigilance, we can protect ourselves and each other.
Your skin tells the story of your life. Protect it. Respect it. And never forget that behind every freckle, every scar, every mole is a human being—hoping not just to survive, but to live fully and freely in the skin they’re in.