For generations, hydralazine has been one of medicine’s quiet workhorses. Doctors reached for it during emergencies, pregnant patients relied on it as a lifeline, and hospitals stocked it as a dependable shield against dangerously high blood pressure. Yet even as it saved lives, one unsettling truth lingered just beneath the surface: no one actually knew how it worked.
This strange gap in understanding trailed the drug through decades of clinical use. Hydralazine came from what scientists now call the “pre-target” era, a time when drugs were discovered by watching what they did to patients long before anyone knew what molecules they touched or what biological switches they flipped. As Kyosuke Shishikura of the University of Pennsylvania explains, “Hydralazine is one of the earliest vasodilators ever developed, and it’s still a first-line treatment for preeclampsia—a hypertensive disorder that accounts for 5%–15% of maternal deaths worldwide. It came from a ‘pre-target’ era of drug discovery, when researchers relied on what they saw in patients first and only later tried to explain the biology behind it.”
That missing explanation has finally arrived, and with it came a discovery so unexpected it reaches far beyond blood pressure. A Penn-led research team has uncovered hydralazine’s molecular mechanism, and in the process, stumbled onto a potential new strategy for halting the growth of aggressive brain tumors.
The Moment the Puzzle Locks Into Place
Shishikura, working with his postdoctoral adviser Megan Matthews and a network of collaborators across the United States, set out to answer a deceptively simple question: what exactly does hydralazine do at the molecular level?
Their findings, published in Science Advances, revealed that hydralazine homes in on a tiny but powerful target inside blood vessel cells—an oxygen-sensing enzyme called ADO, short for 2-aminoethanethiol dioxygenase. This enzyme functions as an early warning system. As Matthews describes it, “ADO is like an alarm bell that rings the moment oxygen starts to fall. Most systems in the body take time; they have to copy DNA, make RNA, and build new proteins. ADO skips all that. It flips a biochemical switch in seconds.”
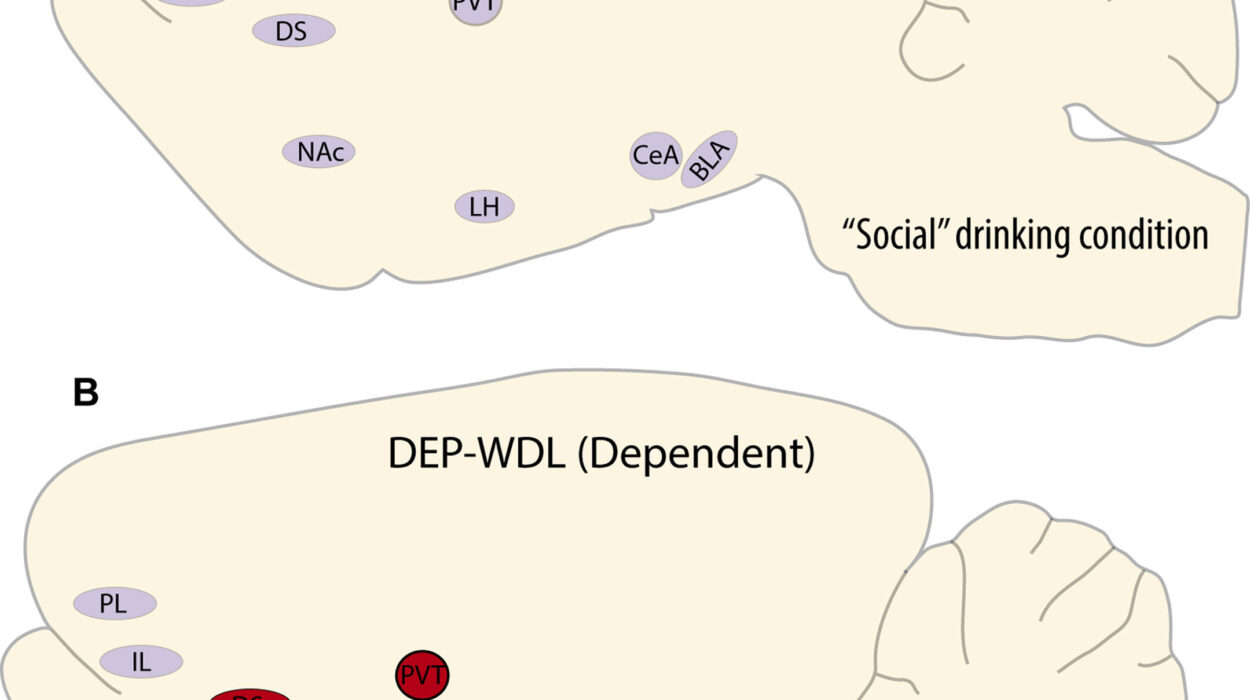
In healthy tissue, that alarm prompts blood vessels to constrict, raising blood pressure to maintain oxygen flow. Hydralazine, however, slips into the enzyme’s metal center and blocks it, silencing the alarm before it can sound. Once ADO is muted, the proteins it normally destroys—regulators of G-protein signaling, or RGS—begin to accumulate. Their presence signals blood vessels to stop tightening.
Shishikura explains that this shift lowers intracellular calcium levels, what he calls the “master regulator of vascular tension.” As calcium levels fall, the muscles lining the vessels relax. Blood pressure drops. The long-standing mystery is solved.
For Matthews, the discovery is also personal. “Preeclampsia has affected generations of women in my own family and continues to disproportionately impact Black mothers in the United States,” she says. “Understanding how hydralazine works at the molecular level offers a path toward safer, more selective treatments for pregnancy-related hypertension—potentially improving outcomes for patients who are at greatest risk.”
A Stunning Connection Emerges in the Darkest Parts of the Brain
Just as the team uncovered hydralazine’s vascular mechanism, another trail of clues emerged from the world of brain cancer research. Many scientists studying glioblastoma had begun to suspect that the same enzyme hydralazine blocks—ADO—plays a critical role in helping tumors survive in pockets of extremely low oxygen. More ADO, they found, often meant more aggressive disease.
But they lacked a reliable way to test what would happen if the enzyme was shut down.
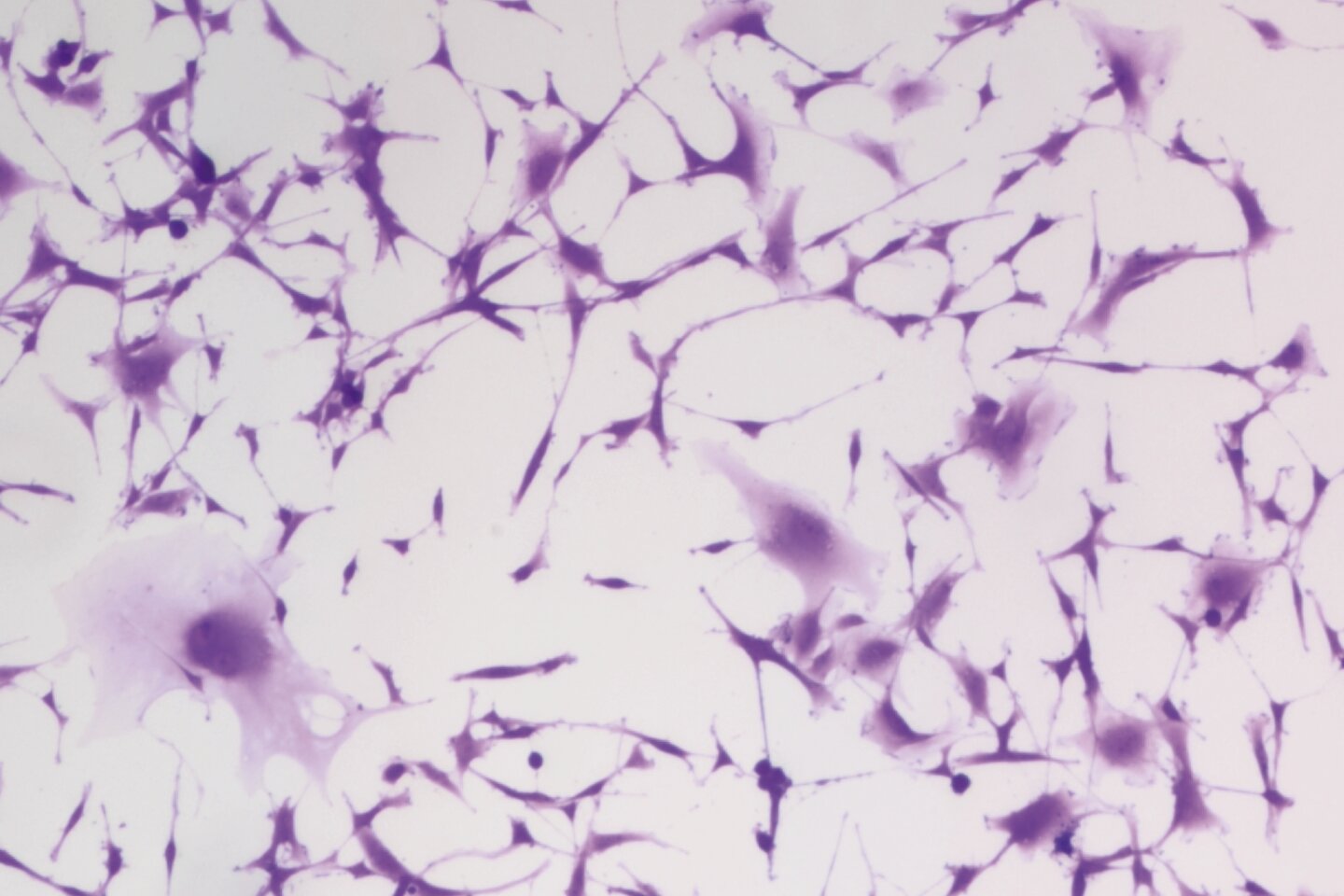
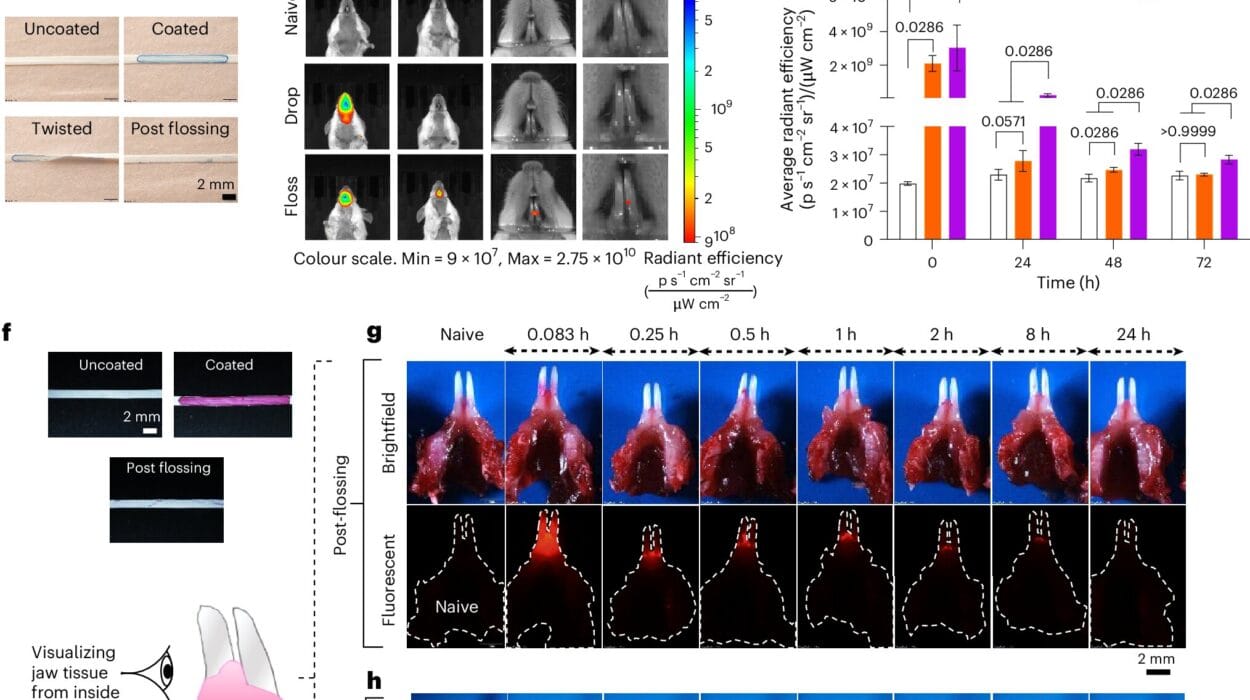
Shishikura and his collaborators stepped into that gap. Structural biochemists at the University of Texas used X-ray crystallography to capture a striking image of hydralazine bound directly to ADO’s metal center. Meanwhile, neuroscientists at the University of Florida tested the drug on glioblastoma cells.
What they observed surprised everyone.
The same biological pathway that controls vascular tension also helps tumor cells endure hostile, oxygen-starved environments. Blocking ADO disrupted this survival loop. Instead of killing the tumor cells outright—which often triggers inflammation, resistance, or relapse—hydralazine pushed them into senescence, a dormant state where they simply stopped dividing.
A seventy-year-old blood pressure drug had paused the growth of one of the deadliest brain tumors known to medicine.
Where Old Drugs Become New Possibilities
The discovery opens more doors than it closes. For Shishikura, the next frontier lies in designing new ADO inhibitors, molecules that build on hydralazine’s chemistry but are tuned specifically for the brain. These future drugs will need to slip past—or strategically exploit—vulnerabilities in the blood-brain barrier, striking tumor tissue while leaving the rest of the body untouched.
Matthews, too, sees vast potential in revisiting long-established medicines with fresh biochemical tools. “It’s rare that an old cardiovascular drug ends up teaching us something new about the brain,” she says, “but that’s exactly what we’re hoping to find more of—unusual links that could spell new solutions.”
Their work stands as a reminder that even in the age of high-tech drug design, some of the most transformative discoveries can still come from the familiar and the overlooked.
Why This Research Matters
Understanding hydralazine’s mechanism is far more than a scientific curiosity. It illuminates the biology behind a drug relied on by pregnant patients around the world. It clarifies how to design safer treatments for conditions like preeclampsia, which continues to claim the lives of mothers at alarming rates. And in an unanticipated twist, it brings hope to a completely different realm of medicine—the fight against glioblastoma, a cancer notorious for resisting nearly every therapy thrown at it.
By revealing the hidden workings of a decades-old drug, the Penn-led team has opened a pathway toward treatments that are not only more effective but more humane, capable of easing the burden of hypertension during pregnancy while also offering a new strategy to slow one of the deadliest brain tumors known. This research shows that sometimes the future of medicine begins by looking again at what we thought we already understood, and discovering that within the familiar lies something profoundly new.
More information: Kyosuke Shishikura et al, Hydralazine inhibits cysteamine dioxygenase to treat preeclampsia and senesce glioblastoma, Science Advances (2025). DOI: 10.1126/sciadv.adx7687