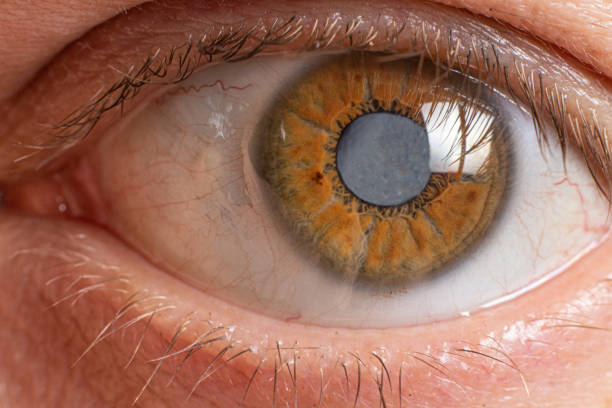
Imagine waking up one morning to find that your vision in one eye has dimmed, colors seem duller, and every movement of your eye brings a sharp, unfamiliar pain. This is the terrifying reality for those who experience optic neuritis, an inflammatory condition that strikes the optic nerve—the cable connecting the eye to the brain. Often sudden and deeply unsettling, optic neuritis can blur or even temporarily erase sight, leaving behind a haunting question: why does the immune system attack something as vital as vision?
For decades, scientists have known that optic neuritis is an autoimmune-mediated demyelinating disorder, meaning the immune system mistakenly attacks the protective sheath (myelin) surrounding nerve fibers. The result is inflammation, nerve damage, and impaired signal transmission between the eye and brain. The condition is often associated with multiple sclerosis but can also appear on its own or in connection with other immune-driven diseases.
Now, new research from Sungkyunkwan University in Korea adds an unexpected layer to this story—suggesting that common allergic conditions like hay fever may play a role in raising the risk of optic neuritis.
The Study That Sparked New Questions
In the groundbreaking study, “Analysis of optic neuritis risk in patients with allergic diseases,” published in Scientific Reports, a team of Korean researchers sought to explore a link that had long been suspected but never confirmed at a national level: could chronic allergic diseases predispose individuals to autoimmune inflammation in the eye?
To answer this, the researchers turned to one of the world’s most comprehensive health databases—the Korean National Health Insurance Service (NHIS). From it, they analyzed data from over 4 million adults who underwent health screenings in 2009. Each participant was tracked for nearly a decade, through December 2018, or until a diagnosis of optic neuritis was made.
During this extensive 8.2-year median follow-up, 3,640 individuals developed optic neuritis—roughly 3.7 cases per 100,000 person-years, aligning with known global incidence rates. But the researchers were less interested in raw numbers and more in patterns: Who was more likely to develop the disease, and why?
Allergic Diseases Under the Microscope
The study focused on three of the most prevalent allergic conditions—atopic dermatitis (eczema), asthma, and allergic rhinitis (commonly known as hay fever). These are not minor irritations; they are chronic inflammatory disorders that affect millions of people worldwide and often persist for life.
Each of these conditions stems from an overactive type 2 immune response, where the body reacts strongly to normally harmless environmental substances such as pollen, dust, or food proteins. While these reactions primarily affect the skin, lungs, or nasal passages, they also reflect a broader state of systemic inflammation—an immune system constantly on alert.
The researchers wondered whether this state of chronic inflammation might create fertile ground for other immune-mediated diseases to emerge—such as optic neuritis, where inflammation turns against nerve tissue itself.
What the Researchers Found
When the data were analyzed, a clear trend emerged. Individuals with any allergic disease showed a 31.7% higher risk of developing optic neuritis compared with those without allergies. This relationship held true even after adjusting for a long list of potential confounders, including age, sex, smoking habits, alcohol consumption, exercise frequency, income level, body mass index, diabetes, hypertension, and dyslipidemia.
But the most striking finding was tied to allergic rhinitis. Among the three conditions, hay fever stood out as the strongest predictor, with an adjusted hazard ratio (HR) of 1.335—meaning those with allergic rhinitis were about 33% more likely to develop optic neuritis during the follow-up period.
By contrast, asthma and atopic dermatitis did not maintain statistically significant associations once adjustments were made for lifestyle and metabolic factors. Moreover, the relationship between allergies and optic neuritis did not differ significantly by age or sex, suggesting the connection transcends demographic boundaries.
Connecting the Dots: The Biology Behind the Link
What might explain this curious overlap between allergies and autoimmunity? At first glance, they seem like opposite ends of the immune spectrum—one overreacting to external substances, the other misfiring internally. Yet modern immunology tells a more nuanced story.
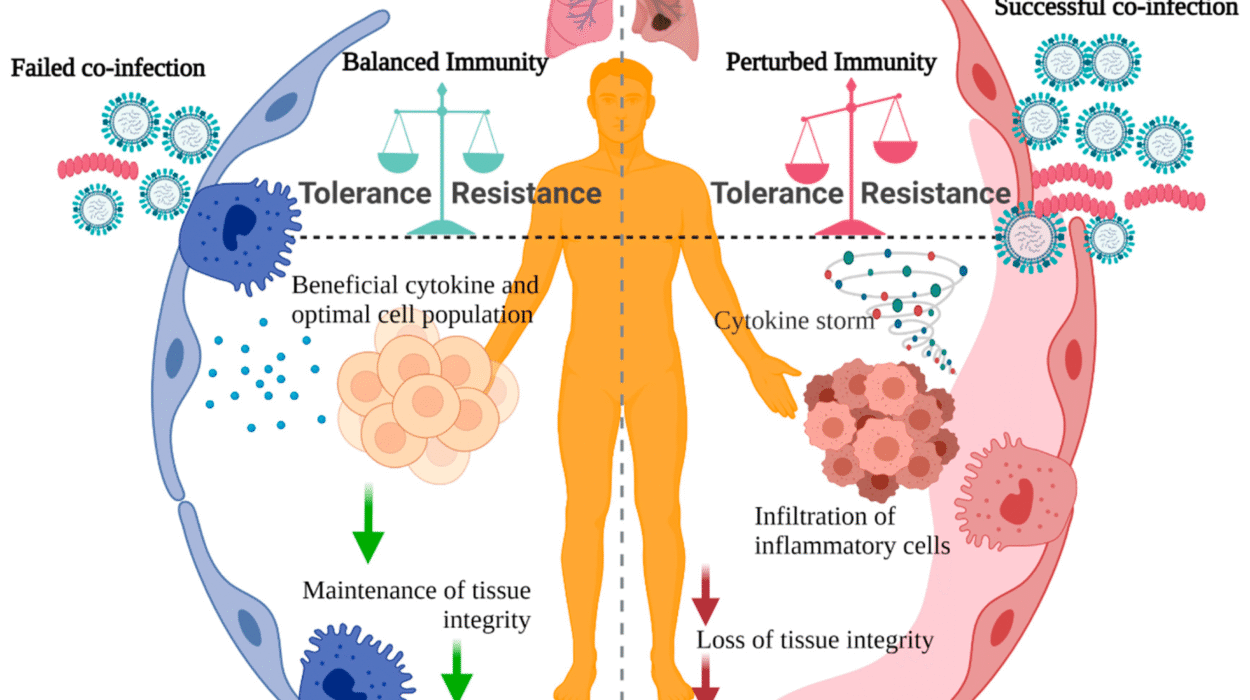
Both allergies and autoimmune diseases share a common thread: immune dysregulation. In allergic diseases, the immune system skews toward type 2 helper T-cell (Th2) responses, releasing cytokines like IL-4, IL-5, and IL-13, which promote inflammation and antibody production. In autoimmune diseases, type 1 (Th1) and Th17 pathways often dominate, attacking the body’s own tissues.
However, emerging evidence suggests that these immune pathways can influence each other. Chronic allergic inflammation can alter the immune system’s balance, making it more prone to misidentifying self-antigens as threats. This breakdown of immune tolerance could, in some individuals, open the door to autoimmune reactions such as those seen in optic neuritis.
Another possible mechanism lies in the blood–brain barrier, a protective shield that separates the brain and spinal cord from circulating immune cells. Inflammation from chronic allergies may subtly weaken this barrier, allowing immune mediators to access the central nervous system and trigger neuroinflammation.
A Korean Perspective with Global Implications
Korea’s universal healthcare system and comprehensive national database offer a unique window into long-term population health trends. By leveraging data from over four million people, the Sungkyunkwan University team achieved a level of statistical power rarely possible in smaller studies.
Still, the authors were careful to note that their findings do not prove causation. The study shows an association—a compelling one—but it cannot yet explain precisely how or why allergic rhinitis increases optic neuritis risk. Additional experimental and longitudinal studies will be needed to confirm whether shared inflammatory pathways truly drive both conditions.
Nevertheless, the implications are profound. If chronic allergic inflammation does predispose individuals to optic neuritis, it could reshape how clinicians approach both diseases. Routine management of allergies might not only improve comfort and quality of life—it could potentially help protect vision.
Seeing the Immune System in a New Light
The eyes, long celebrated as “windows to the soul,” may also be mirrors of the immune system’s inner workings. Optic neuritis, while rare, serves as a vivid reminder of how intimately the immune system and nervous system are intertwined.
This study encourages a shift in how we view allergic diseases—not merely as isolated, localized irritations, but as signals of broader immune imbalances that may ripple through the body. It reminds us that health is a delicate equilibrium: when inflammation becomes chronic, it can blur the line between defense and destruction.
For patients, these findings underscore the importance of early and consistent management of allergic conditions. For researchers, they open new avenues for exploring the molecular bridges between allergy and autoimmunity. And for the medical community, they highlight the need to see beyond individual symptoms—to treat the immune system as an integrated whole.
Toward a Future of Integrated Immunology
As medicine moves deeper into the age of precision health, the Sungkyunkwan study exemplifies how large-scale data and deep biological insight can work together. Understanding the immune system no longer means studying diseases in isolation; it means recognizing the common threads that connect them.
Future research may identify specific genetic or environmental factors that make some allergy sufferers more vulnerable to autoimmune complications. It may even reveal biomarkers that predict who is at risk before symptoms arise—offering a chance for prevention instead of reaction.
If such discoveries emerge, they will not only protect sight but illuminate how the immune system’s vast and complex network can sometimes turn from guardian to aggressor.
More information: Jaeryung Kim et al, Analysis of optic neuritis risk in patients with allergic diseases, Scientific Reports (2025). DOI: 10.1038/s41598-025-18088-6