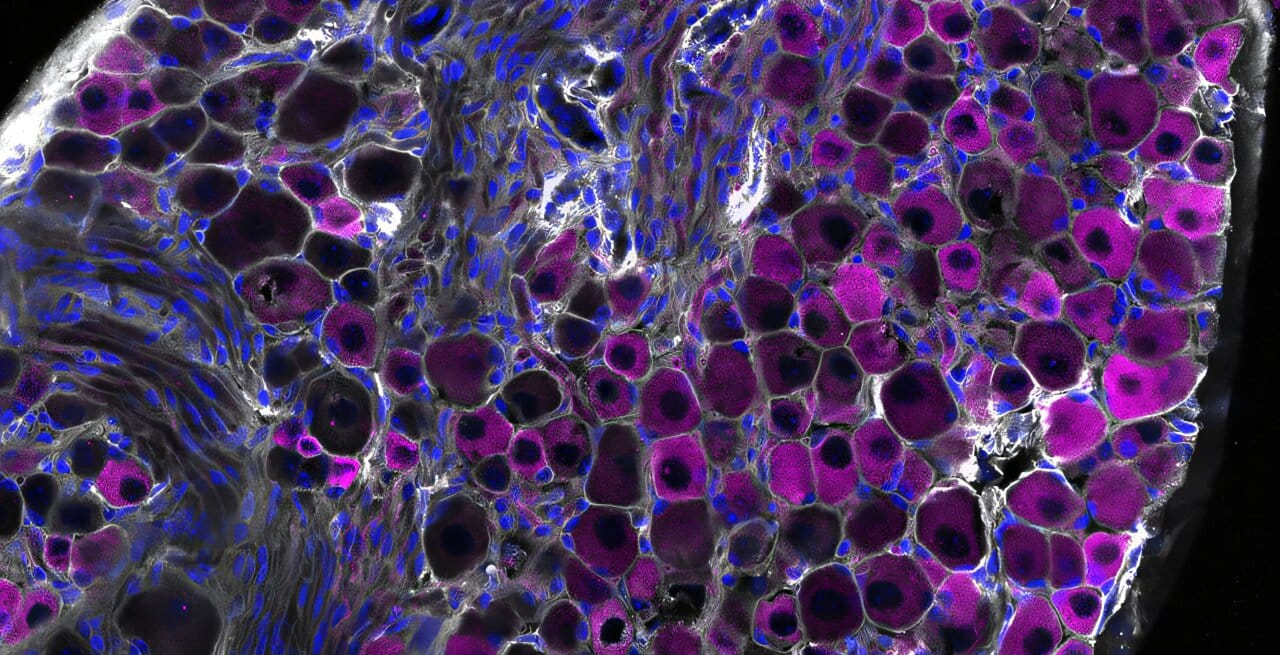
For decades, scientists have known that a special group of nerve cells, called TRPV1 vagal nociceptors, live inside the vagus nerve and serve as sentinels of the body. They detect heat, chemical irritation, tissue injury, and pressure—alerting the brain and triggering protective reflexes such as coughing. If you’ve ever had a persistent cough during a cold, it’s thanks to these tiny nerve cells working to clear your airways.
But a new study from Harvard Medical School and the Harvard T.H. Chan School of Public Health reveals something surprising: these same nerve cells do more than clear irritants from the lungs. They act as guardians against one of the deadliest aspects of influenza—the body’s own overactive immune response.
In a groundbreaking discovery published in Science Immunology, researchers showed that TRPV1 vagal nociceptors can calm the immune system during flu infections, preventing runaway inflammation that damages lung tissue. In other words, the nerves are not just alarm bells; they are also peacemakers, making sure the body’s defenses don’t become its greatest threat.
The Hidden Danger of the Flu
Every year, influenza sickens millions worldwide and kills up to 650,000 people, according to the World Health Organization. While the virus itself causes harm, much of the severe damage comes from the body’s own reaction to it. The immune system, in its urgency to kill the virus, often overshoots—flooding the lungs with immune cells that attack infected tissue but also injure healthy cells in the process.
This phenomenon, known as immune-driven lung damage, can turn a mild infection into a life-threatening illness. It’s the same type of runaway immune response that contributed to the devastating effects of COVID-19, where inflammation sometimes caused more damage than the virus itself.
The new research highlights that the lungs are not only a battleground between virus and immune system—they are also the stage for an intricate dance between nerves and immunity.
“Our research shows that the infected lung is a battleground where nerves and immune cells engage in a delicate dance to safeguard our health,” explained Isaac Chiu, professor of immunology at Harvard Medical School and co-senior author of the study.
What the Experiments Revealed
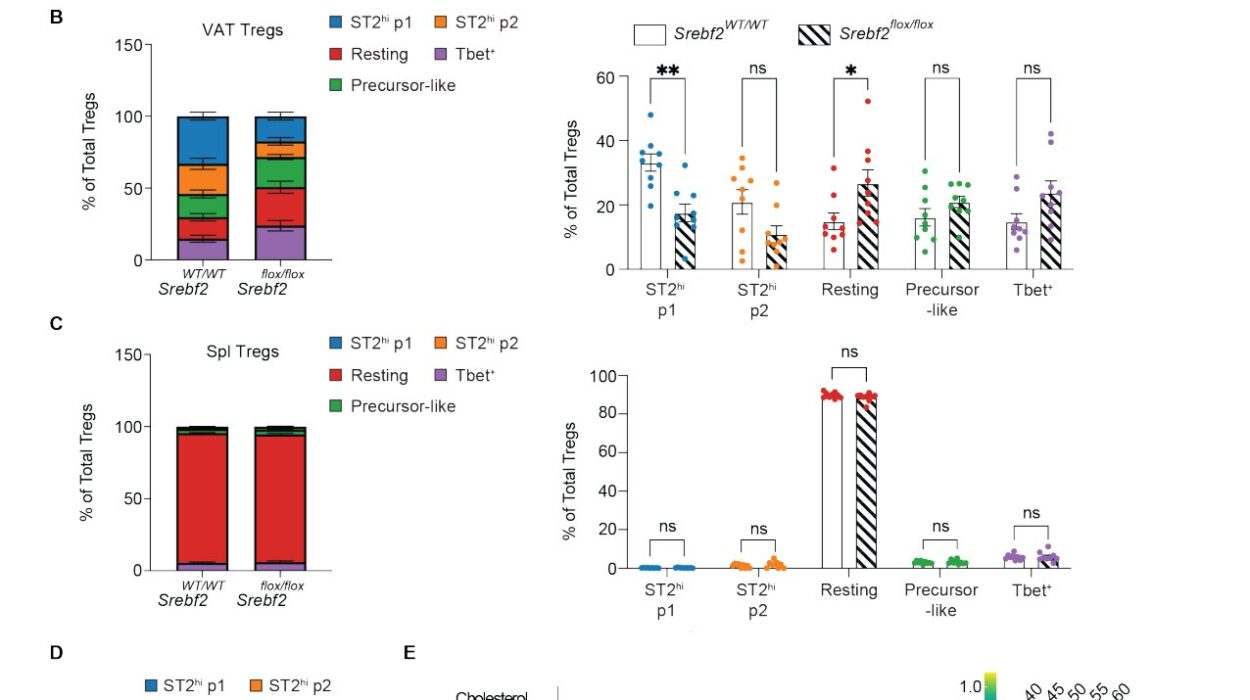
To test how these nerve cells influence flu infections, the researchers used mice infected with the influenza A virus. Some mice had fully functioning TRPV1 neurons, while in others these neurons were chemically silenced or genetically disabled.
The results were striking. Mice without TRPV1 neurons did not have more virus in their lungs—the viral load was nearly identical to mice with functioning neurons. But the outcome of the infection was dramatically different.
- Mice without these neurons developed worse lung damage.
- They experienced higher levels of inflammation.
- Their survival rates dropped significantly.
Even more telling, when researchers analyzed the immune cells in the lungs, they found a dangerous imbalance. Mice without TRPV1 neurons had an excess of neutrophils and macrophages—cells that, in moderation, help clear infection but, in excess, wreak havoc on tissue. At the same time, these mice showed weaker interferon signaling, an antiviral defense pathway critical for containing viral spread.
Nicole Almanzar, the study’s first author and a doctoral student in the Chiu Lab, explained:
“Our study demonstrates that the nervous system is actively involved in regulating the response of the lungs to infection, offering a new perspective on viral infections that could help explain why particular factors increase the risk of severe infections.”
A Tale of Two Outcomes
What makes the finding so fascinating is that the virus itself was not more aggressive in mice lacking TRPV1 neurons—their viral load was the same. The difference lay entirely in how their bodies responded to infection.
In healthy mice, TRPV1 neurons acted like a brake, slowing down the immune system at just the right moment. In the absence of that brake, the immune system ran wild, damaging the very lungs it was trying to protect.
This discovery adds a new dimension to our understanding of why flu outcomes vary so much between people. Some individuals recover relatively easily, while others—particularly the elderly or those with underlying conditions—develop devastating, long-lasting damage. The balance of neuro-immune communication may be one of the hidden factors that explains this variability.
The Mystery of How Nerves Restrain Immunity
Although the experiments clearly showed that TRPV1 neurons restrain inflammation, the exact molecular mechanisms remain unknown. How do these nerve cells signal to immune cells to hold back? What neurotransmitters or signaling molecules are involved?
“The vagus nerve is powerfully controlling inflammation, but how it does so remains a mystery to be solved,” Chiu said.
What scientists do know is that this is not the first time nerves have been found to influence immunity. Chiu’s earlier research showed similar crosstalk between nerves and immune cells in conditions such as bacterial pneumonia, meningitis, flesh-eating disease, pain, and itch. In bacterial infections of the lung, vagal neurons suppressed immune defenses in a way that was harmful. But in viral infections like the flu, the same neurons shift roles, shielding the lung from overactive immunity.
The Future: Could We Harness This Natural Brake?
The discovery opens up exciting possibilities for new treatments. Traditionally, antiviral therapies have aimed either to attack the virus directly or to dampen the immune system when it becomes too destructive. Both strategies have limits: antivirals can struggle against rapidly mutating viruses, and suppressing immunity can leave the body vulnerable to infection.
What if, instead, medicine could mimic the body’s own neural brake? By stimulating or enhancing the protective function of TRPV1 neurons, therapies could prevent immune overreaction without shutting down the body’s ability to fight the virus.
This idea is not science fiction. The U.S. FDA recently approved a treatment for rheumatoid arthritis that uses vagus nerve stimulation to control immune activity. If similar techniques could be refined for the lungs, they might one day prevent the worst complications of flu, COVID-19, and other viral infections.
“Imagine if you could harness this brake to control inflammation in the lungs and beyond,” Chiu said. “By stimulating related circuits where the vagus nerve shuts down immune cells, one could envision treating immune-mediated dysfunction of many kinds, including that caused by viral infections.”
Why This Discovery Matters Now
The COVID-19 pandemic showed the world just how dangerous uncontrolled immune responses can be. Patients who developed severe disease often suffered not from the virus itself but from cytokine storms—runaway inflammation that damaged lungs, heart, and other organs.
The new findings underscore that our nervous system is not just a bystander during infection—it is an active partner, shaping the immune response in ways that can mean the difference between life and death.
They also remind us that healing is not always about fighting harder but about fighting smarter—finding balance between defense and restraint, between attack and protection.
More information: Nicole Almanzar et al, Vagal TRPV1 + sensory neurons protect against influenza virus infection by regulating lung myeloid cell dynamics, Science Immunology (2025). DOI: 10.1126/sciimmunol.ads6243