In the hushed silence of a high-tech operating room, a patient lies peacefully anesthetized while a surgeon, seated at a nearby console, maneuvers robotic arms with precision that human hands could never achieve alone. The surgical instruments are nimble, steady, and microscopically accurate, moving in perfect synchronization with the surgeon’s commands—like an orchestra obeying its conductor. Welcome to the future of surgery. This is not science fiction. This is robotic surgery.
Robotic-assisted surgery is transforming the field of medicine, redefining what is possible inside the human body. It blends the intelligence, decision-making, and experience of a human surgeon with the precision, flexibility, and control of advanced robotic systems. In this article, we will dive deep into the fascinating world of robotic surgery: how it works, why it matters, where it’s headed, and how it’s reshaping the future of healthcare as we know it.
Understanding Robotic Surgery: Not Robots Doing Surgery Alone
One of the biggest misconceptions about robotic surgery is that autonomous machines are performing operations while doctors watch from the sidelines. This could not be further from the truth. Robotic surgery is surgeon-led from start to finish.
The term “robotic surgery” refers to procedures performed using robotic systems that extend the surgeon’s capabilities. These systems allow for finer control, better visualization, and minimally invasive techniques that traditional methods simply cannot match.
In most cases, the robot doesn’t make any decisions or perform any independent movements. Every motion is guided, directed, and executed by a human surgeon. The robot is an extension—a powerful, finely tuned instrument that enhances the surgeon’s skillset.
The most well-known and widely used robotic system today is the da Vinci Surgical System, which first gained FDA approval in the early 2000s. With it, surgeons perform complex operations through tiny incisions using robotic arms equipped with miniature surgical tools. Meanwhile, the surgeon sits at a console, peering into a high-definition, 3D visualization of the surgical field, and directing each robotic movement with master controls that mimic their hand motions.
The Anatomy of a Robotic Surgery System
To truly understand how robotic surgery works, let’s break down the major components of a typical robotic surgical system like da Vinci:
1. The Surgeon Console: This is the command center where the surgeon sits during the procedure. It features a stereoscopic 3D viewer and highly sensitive hand and foot controls. From here, the surgeon controls the robotic arms with natural finger movements.
2. The Patient-Side Cart: This is where the robotic arms are positioned. These arms hold the surgical instruments and camera. They are designed for maximum dexterity and can rotate in ways the human wrist cannot.
3. The Vision System: This includes a high-definition 3D camera that provides a magnified view of the surgical site. It allows the surgeon to see inside the body with extraordinary clarity—up to 10 times magnification—offering a level of detail previously unseen.
4. The Instruments: The tools attached to the robotic arms are incredibly precise. Known as “EndoWrist” instruments, they are designed to mimic the movement of a human wrist but with far greater flexibility and accuracy.
Together, these components form an integrated system that allows surgeons to operate with enhanced precision, vision, and control—enabling procedures that would be impossible or highly risky using conventional methods.
The Rise of Minimally Invasive Surgery
One of the primary benefits of robotic surgery is that it allows surgeons to perform minimally invasive procedures—operations done through small incisions rather than large openings. This shift has enormous benefits for patients, including:
- Reduced blood loss
- Shorter hospital stays
- Less postoperative pain
- Smaller scars
- Faster recovery times
- Lower risk of infection
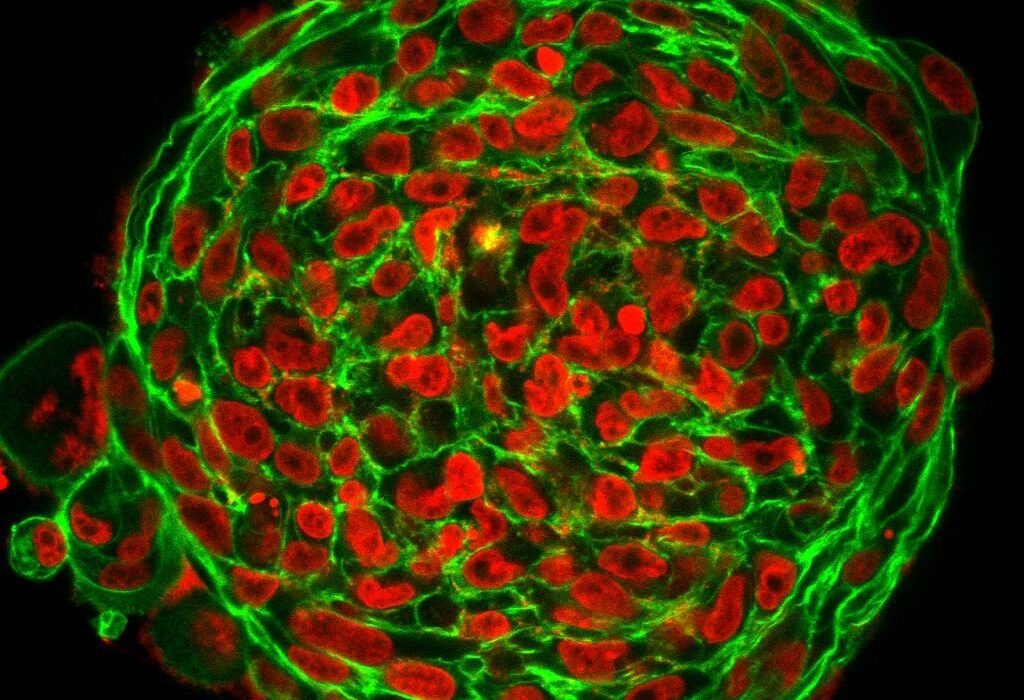
With robotic systems, even intricate and delicate surgeries—such as prostatectomy, hysterectomy, cardiac valve repair, or colorectal resections—can be done through tiny incisions. The robot’s precise movement eliminates the small tremors of the human hand, while its flexible instruments can navigate tight spaces within the body.
The result? Safer surgeries, more consistent outcomes, and a smoother path to healing.
From Prostate to Heart: What Surgeries Are Performed Robotically?
Today, robotic surgery is being used across a broad range of specialties. Let’s explore some of the most common and emerging applications:
Urology: Robotic-assisted prostatectomy (removal of the prostate) is one of the most well-established robotic procedures. It allows for precise removal of the gland while minimizing nerve damage, preserving continence and sexual function.
Gynecology: Robotic systems are increasingly used for hysterectomies, myomectomies (fibroid removal), and endometriosis surgery. The enhanced precision helps surgeons operate around sensitive reproductive organs with great care.
Cardiothoracic Surgery: In the realm of heart surgery, robotic systems allow surgeons to repair heart valves and perform coronary artery bypasses through small incisions between the ribs—avoiding the need to split the breastbone.
General Surgery: Gallbladder removal, hernia repair, colorectal surgery, and bariatric (weight-loss) procedures are increasingly being done with robotic assistance, particularly for complex cases.
Head and Neck Surgery: Transoral robotic surgery (TORS) enables surgeons to access and remove tumors from the throat and base of the tongue without external incisions.
Orthopedics: While not as widespread yet, robotic arms are being used in joint replacements to ensure precise alignment of prosthetics.
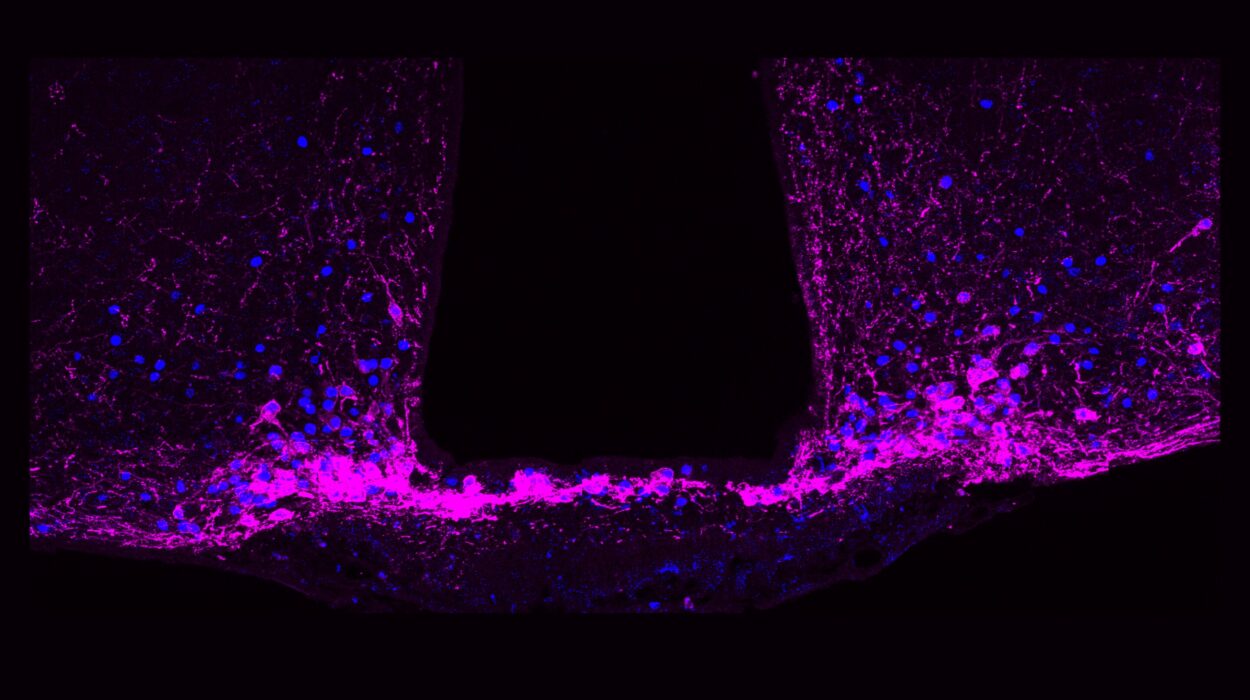
As technology advances, the list continues to grow. Even neurosurgery—perhaps the most delicate of all fields—is exploring robotic tools for improved accuracy in brain and spinal procedures.
Training the Surgeon of Tomorrow
A robot is only as good as the person operating it. Robotic surgery requires extensive training, and mastering the system is no small feat.
Surgeons must undergo rigorous training programs that include simulations, mentorship, and supervised procedures before being certified to operate independently. Even experienced traditional surgeons must relearn many aspects of their craft—adapting to a new physical posture, different visual feedback, and a different sense of “touch,” known as haptic feedback.
Medical schools and residency programs are now integrating robotic training into their curricula, ensuring that future generations of surgeons are comfortable and skilled in using these systems from the start.
Moreover, continuous learning is crucial. Surgeons regularly update their skills as new tools, software upgrades, and best practices emerge.
Beyond the OR: The Patient Experience
From the patient’s perspective, robotic surgery often feels almost magical. Tiny incisions. Minimal pain. Going home in a day or two. Sometimes walking around the same afternoon. It’s a radical departure from the long, painful recoveries of traditional open surgery.
Many patients report feeling anxious about the idea of robots being involved in their surgery, but once they understand that a skilled human is guiding every movement, those fears often subside. In fact, patients are increasingly requesting robotic options—particularly when presented with data showing faster recovery times and lower complication rates.
Hospitals, too, are embracing robotic surgery as a key selling point, marketing their advanced technology to attract patients and top-tier surgical talent.
Challenges and Controversies
Despite its advantages, robotic surgery is not without controversy.
1. Cost: Robotic systems are expensive. A da Vinci robot can cost $1.5 to $2 million, with additional maintenance and instrument costs. This can strain hospital budgets and contribute to higher healthcare costs overall.
2. Access and Equity: Smaller hospitals and low-income regions may not have access to this technology, creating disparities in care. Ensuring equitable distribution of surgical advances is a major ethical concern.
3. Learning Curve: As with any new technology, there is a learning curve. In inexperienced hands, robotic surgery can lead to longer operative times and potentially worse outcomes. Ensuring consistent training and credentialing is essential.
4. Overuse: Some critics argue that robotic systems are being used in cases where traditional laparoscopic methods would suffice. The pressure to recoup costs can drive overutilization, raising questions about clinical necessity.
5. Lack of Haptic Feedback: Many robotic systems lack true tactile feedback, which surgeons rely on during manual procedures. While visual cues often suffice, some experts believe this is a limitation yet to be fully solved.
These challenges highlight the importance of thoughtful, data-driven integration of robotic surgery into healthcare systems.
The Next Frontier: AI, Automation, and Remote Surgery
Where is robotic surgery headed next? The answer lies in three exciting directions: artificial intelligence (AI), automation, and remote surgery.
AI in Surgery: AI algorithms are being developed to assist in real-time decision-making during surgery. These systems can analyze video feeds, detect critical anatomy, warn of potential errors, and even suggest optimal movements. Over time, AI could become a kind of surgical co-pilot, enhancing safety and consistency.
Automation: Fully autonomous surgery—where robots perform operations without human input—is still far off. However, partial automation is already happening. Tasks like suturing, tissue dissection, or targeting specific areas are being tested with promising results. Eventually, routine procedures could become faster, cheaper, and safer through automation.
Remote Surgery: Also known as telesurgery, this involves a surgeon operating a robot from miles—or even continents—away. This concept was demonstrated as early as 2001 in the “Lindbergh Operation,” when a surgeon in New York performed gallbladder surgery on a patient in France. With modern 5G networks and ultra-low latency, remote surgery could one day allow experts to operate on patients in disaster zones, war zones, or rural areas without ever leaving their base hospital.
These developments raise critical questions: Who is liable if a robot malfunctions mid-procedure? Can an AI-assisted surgery be considered malpractice if the AI gives a bad suggestion? How do we regulate a technology that moves faster than policy?
The road ahead is exciting—but requires careful navigation.
Will Robots Replace Surgeons?
This is the question that keeps coming up: Will robots eventually replace human surgeons?
The short answer is no—at least not for the foreseeable future.
Surgery is not just about cutting and sewing. It involves judgment, adaptability, intuition, and empathy. Every patient is different, and unexpected complications can arise at any moment. Human surgeons bring a depth of experience and emotional intelligence that machines have yet to replicate.
What robots will do—and are already doing—is augmenting the surgeon’s capabilities. They are tools, not replacements. They allow the surgeon to be more precise, more confident, and more effective.
In the future, the most successful surgeons will be those who can combine traditional skills with technological fluency—merging the art of medicine with the science of machines.
A Glimpse into Tomorrow’s Operating Room
So, what might the operating room of 2050 look like?
You walk into a surgical suite that feels more like a spaceship than a hospital room. Robots stand ready, sterilized and waiting. The patient lies on a platform that automatically adjusts posture and pressure points in real-time using AI algorithms to minimize complications.
The surgeon, seated at a futuristic console, speaks to a voice-activated assistant that brings up diagnostic data, scans, and surgical blueprints. Augmented reality overlays guide the incision. A robotic arm begins to suture as another retracts tissue. The surgeon, like a conductor, orchestrates the entire performance with calm authority and surgical artistry.
Outside, a patient’s family watches a real-time 3D model of the surgery on a screen, with simple explanations provided by an AI interface. No fear. No mystery. Just clarity, confidence, and care.
Conclusion: The Scalpel Meets the Silicon Age
Robotic surgery is more than a technological breakthrough—it’s a paradigm shift. It represents the merging of human expertise with machine precision. It offers the promise of safer, faster, and less painful surgery. And it opens the door to possibilities we’ve only begun to imagine: AI-assisted diagnostics, fully remote procedures, even space-based surgeries for astronauts on Mars.
But with great power comes great responsibility. As we move into this brave new era, we must ensure that innovation serves humanity—not the other way around. Robotic surgery should be a tool for healing, not profit; a bridge to better care, not a divide that leaves the underserved behind.
The future of the operating room is already here. And it’s robotic, intelligent, and deeply human.