For over a century, scientists have dreamed of using bacteria to fight cancer. The dream began in the 19th century when German physician Dr. Wilhelm Busch noticed that infecting cancer patients with bacteria could sometimes shrink tumors. Dr. William Coley later tried to turn that observation into a treatment, injecting bacterial toxins into cancer patients in hopes of triggering an immune response. These early efforts inspired the long journey that led to today’s powerful cancer immunotherapies—like checkpoint inhibitors and CAR-T cell therapy—that harness the body’s immune system to destroy tumors.
But there’s a catch: these therapies only work if the immune system is healthy. For many cancer patients, especially those weakened by chemotherapy or radiation, the immune system is compromised. For them, immunotherapy often fails.
Now, that may be about to change.
A joint team of scientists from the Japan Advanced Institute of Science and Technology (JAIST), Daiichi Sankyo Co., Ltd., and the University of Tsukuba has developed a completely new type of cancer treatment. Published in Nature Biomedical Engineering, their study reveals a bacterial therapy that works without any help from the immune system at all.
This breakthrough could change the landscape of cancer treatment—especially for patients who’ve run out of options.
Meet AUN: A Microbial Duo That Destroys Cancer in Harmony
The therapy, called AUN, is named after a Japanese concept that refers to perfect balance and cooperation between opposites. And that’s exactly what this therapy represents—a harmony between two very different bacteria working together to destroy cancer.
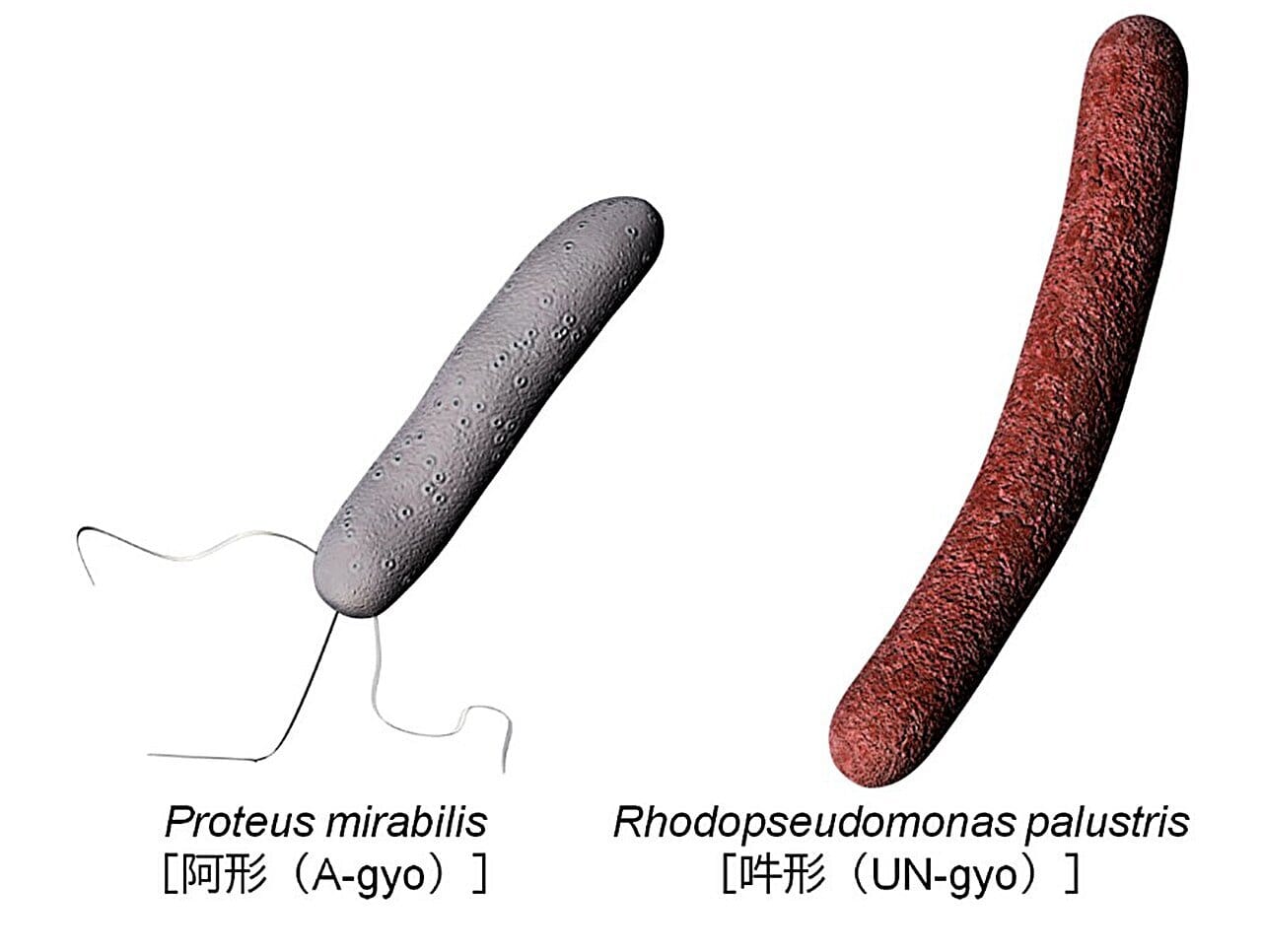
AUN is made of two naturally occurring microbial strains:
- Proteus mirabilis, known here as A-gyo, which is a type of bacterium that naturally prefers to live inside tumors.
- Rhodopseudomonas palustris, referred to as UN-gyo, a photosynthetic bacterium usually found in nature but repurposed here to regulate and enhance A-gyo’s cancer-fighting behavior.
On their own, neither of these microbes is effective. But when combined, they create a dynamic duo capable of attacking tumors in a completely new way.
How AUN Works Without the Immune System
Unlike traditional immunotherapy, which relies on T-cells or other immune agents to attack tumors, AUN works by directly disrupting the tumor from within. In tests on both mouse and human cancer models, the bacteria successfully eradicated tumors even in immunocompromised environments.
That means AUN worked even when the immune system was offline—a major breakthrough for patients who can’t benefit from standard treatments.
Here’s how the process unfolds:
- Once injected into the body, A-gyo homes in on tumors, where it begins to multiply.
- Inside the tumor, the cancer’s own unique metabolic environment triggers a transformation: A-gyo changes shape, becoming long and filament-like. This change increases its ability to disrupt tumor cells and blood vessels.
- Meanwhile, UN-gyo acts as a regulatory partner. Though it makes up only about 3% of the initial bacterial mixture, it helps control A-gyo’s growth, preventing it from becoming harmful to the rest of the body.
- Once inside the tumor, the ratio dramatically shifts: A-gyo dominates, rising to 99% of the bacterial population, targeting the tumor with surgical precision.
- Throughout this process, pathogenicity is suppressed, meaning the bacteria do their job without causing widespread inflammation or cytokine storms—dangerous side effects seen in other forms of bacterial therapy.
The Beauty of Biological Balance
What makes AUN truly revolutionary is not just that it works, but how it works.
This is not a blunt-force attack. It’s a carefully choreographed biological ballet. The bacteria don’t just kill—they adapt, evolve, and communicate within the tumor microenvironment. Their behavior is regulated by each other, responding to cues from the cancer itself.
UN-gyo, for instance, doesn’t fight the tumor directly. Instead, it plays a behind-the-scenes role, keeping A-gyo in check and ensuring the therapy remains safe and targeted. This concept of “division of labor” between two organisms mimics natural ecosystems—yet here, it’s applied to medicine in a stunningly effective way.
It’s a living system that becomes smarter and more effective once it enters the tumor. It doesn’t depend on external control, drugs, or immune cells. It self-organizes. It evolves within the cancer to do exactly what’s needed.
Why This Matters for Real Patients
For millions of cancer patients around the world, especially those undergoing chemotherapy or suffering from late-stage cancers, their immune systems are simply not strong enough for traditional immunotherapy. Checkpoint inhibitors and CAR-T therapies, while powerful, require a functioning army of immune cells to be effective.
AUN changes that equation.
“This therapy offers a long-awaited solution for patients who can’t be helped by current immunotherapies,” said Professor Eijiro Miyako, the lead author of the study. “We’re finally seeing the dawn of truly immune-independent cancer treatment.”
What’s more, the bacteria used in AUN are naturally occurring and have high biocompatibility, meaning they don’t trigger massive immune responses or dangerous side effects like cytokine release syndrome—a common and potentially deadly complication in other aggressive therapies.
The therapy was shown to be safe and well-tolerated, at least in the preclinical models. The bacteria stayed inside the tumor, didn’t spread to healthy tissues, and didn’t provoke harmful inflammation.
Looking Ahead: Clinical Trials and Beyond
The research team is already planning the next phase: moving from the lab to the clinic. They hope to launch a biotech startup and begin human clinical trials within the next six years.
That’s a long time for patients in need—but in the world of drug development, it’s remarkably fast.
Of course, many hurdles remain. What works in mice and lab models doesn’t always translate to human patients. Safety must be ensured. Dosing must be perfected. And large-scale trials must prove that the therapy works not just in theory, but in real-world clinical settings.
Still, the excitement in the scientific community is real. This could mark the beginning of a new chapter in cancer treatment—one that returns to the promise of bacteria as a weapon against cancer, but with all the power of modern science behind it.
A Revolution Rooted in History
It’s poetic that this breakthrough comes more than 150 years after the first reports of bacteria curing cancer. What began as anecdotal stories and trial-and-error has now matured into a precise, targeted, and intelligent therapy.
Back then, scientists injected patients with bacteria and hoped for the best. Now, researchers can engineer microbial ecosystems to behave in specific ways, adapting to the unique conditions inside a tumor.
It’s a fusion of ancient inspiration and modern technology. And it’s being led by scientists in Japan who saw beauty not just in biology, but in harmony—AUN.
The Bottom Line
AUN is more than a scientific discovery. It’s a hopeful message: that even in the most hostile environments, cooperation can overcome destruction. That bacteria, once seen only as threats, can become healers. That cancer, for all its complexity, may one day be outsmarted not by brute force, but by balance.
If future trials are successful, AUN could become the first truly immune-independent cancer therapy—giving new hope to patients who need it most, and redefining what we think bacteria can do.
The war on cancer has many fronts. AUN opens a new one—quiet, precise, and full of promise.
More information: Tumour-resident oncolytic bacteria trigger potent anticancer effects through selective intratumoural thrombosis and necrosis, Nature Biomedical Engineering (2025). DOI: 10.1038/s41551-025-01459-9