For millions of people, migraine without aura arrives like an uninvited storm. There are no flickering lights, no shimmering zigzags in the air, no early alarm bells. Just the sudden surge of throbbing pain that can hijack an entire day. This form of migraine, the most common type of this neurological disorder, disrupts work, family life, and even the simplest daily tasks.
Standard treatments exist. Pain-relieving drugs and preventive medications are widely used. But not everyone can tolerate them. For some, the side effects are as disruptive as the migraine itself. For others, relief remains frustratingly incomplete.
So when a new study, published in JAMA Network Open, reported that acupuncture significantly reduced the number of migraine days per month, it stirred more than academic curiosity. It hinted at something deeply human: the possibility of reclaiming lost days.
A Question Doctors Couldn’t Fully Answer
Acupuncture is not new. It has steadily grown in popularity as a complementary therapy, and it is already known to be safe and effective for some people. Yet one puzzle has lingered in the medical world. Why do some patients improve dramatically while others feel little change?
Doctors have long observed this uneven response, but understanding the “why” has remained elusive. Is it chance? Expectation? Biology?
To find out, researchers in China designed a careful randomized clinical trial between 2021 and 2023. They recruited 120 participants diagnosed with migraine without aura. Every participant was living with recurring pain. Every participant was hoping for relief.
Half would receive genuine acupuncture, with needles inserted into specific points intended to trigger a healing response. The other half would receive sham acupuncture, a controlled version designed to minimize therapeutic effects. Both groups would undergo 12 sessions over four weeks.
The design was intentional and balanced. If acupuncture truly worked, the difference would reveal itself.
Inside the Brain Before the First Needle
Before a single treatment began, each volunteer lay inside a machine that could peer into the living brain. Using functional MRI, or fMRI, researchers mapped how different regions communicated with one another. This was not about structure. It was about conversation. Which areas spoke strongly? Which barely whispered?
The brain is not a collection of isolated islands. It is a network, a web of signals constantly flowing. In migraine, that network may be wired in ways that amplify pain or disrupt normal function. The researchers wanted to see whether those wiring patterns might predict who would benefit from acupuncture.
After four weeks of treatment, the results began to emerge.
Fewer Days Lost to Pain
The group receiving genuine acupuncture experienced a significant drop in the number of migraine days per month. The reduction was not subtle. It was measurable and meaningful.
Participants also reported decreased pain intensity. They reached for fewer medications to control their attacks. As the headaches eased, so did the grip migraines had on their daily routines. People described improvements in their quality of life. Activities that once felt impossible during frequent attacks became manageable again.
In contrast, the sham acupuncture group did not see the same level of improvement. The controlled design strengthened the conclusion: something specific about real acupuncture appeared to make the difference.
But the most intriguing part of the study was not only that acupuncture worked for many participants. It was that the brain scans seemed to explain why.
The Hidden Patterns in Brain Communication
To analyze the intricate data from the fMRI scans, researchers turned to connectome-based predictive modeling, known as CPM. This artificial intelligence tool maps complex connections throughout the brain, searching for patterns too subtle for the human eye to detect.
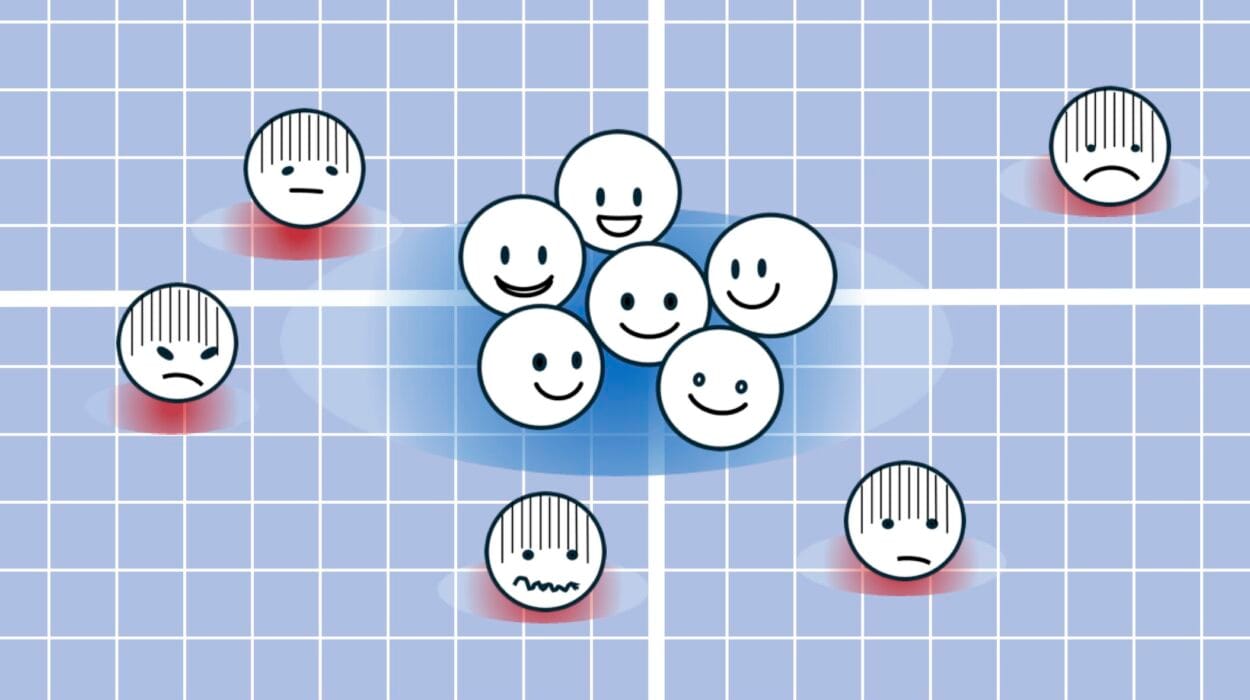
The analysis revealed two specific connectivity patterns that predicted how well someone would respond to acupuncture.
The first pattern involved communication between the brain’s self-reflection centers and its coordination centers. Participants whose brains showed weaker communication between these regions before treatment experienced the most pronounced pain relief. It was as though a quieter internal dialogue between these areas made the brain more responsive to acupuncture’s effects.
The second pattern involved the connection between coordination centers and movement centers. Those with stronger links in this network showed the greatest improvements in daily physical activities after treatment. Their ability to move through life, less hindered by migraine, seemed tied to how efficiently these regions communicated from the start.
These were not vague impressions. They were measurable patterns in brain connectivity. And they offered something rare in migraine research: a predictive clue.
A Step Toward Personalization
For years, migraine treatment has often followed a trial-and-error approach. A medication is prescribed. If it fails, another is tried. Patients may cycle through options, hoping for relief.
This study suggests a different future may be possible. If brain functional connectivity can predict who will benefit most from acupuncture, doctors might one day tailor treatment decisions based on individual brain patterns.
The researchers noted in their paper that the findings highlight changes in brain connectivity during acupuncture and reveal the brain connectome’s potential for personalized therapy. In simpler terms, the brain’s communication map could become a guidebook.
Instead of asking, “Will this work for you?” doctors might one day ask, “What does your brain suggest will work best?”
More Than Needles
The story unfolding here is not just about acupuncture. It is about the brain’s adaptability and the possibility that treatments can reshape how regions interact.
Migraine without aura is often invisible to others. There are no visible warnings. No outward signs until the pain begins. Yet inside the skull, networks are constantly in motion. When those networks shift, even subtly, the experience of pain can change.
This study does not claim that acupuncture works for everyone. It does not suggest replacing standard treatments entirely. What it shows is that for a significant group of patients, genuine acupuncture brought meaningful relief compared to a carefully designed sham procedure.
And crucially, it hints at a biological explanation rooted in measurable brain connectivity patterns.
Why This Research Matters
Migraine without aura is not just a headache. It is a condition that steals days, limits productivity, and erodes quality of life. For patients who cannot tolerate standard medications, options can feel painfully limited.
This research matters because it does two important things at once. First, it provides controlled clinical evidence that real acupuncture can significantly reduce migraine days, lessen pain intensity, and decrease reliance on medication. Second, it moves the field closer to personalized treatment, using the brain’s own connectivity patterns as a guide.
The discovery of predictive patterns through fMRI and CPM suggests that migraine therapy may one day be chosen not by guesswork, but by neuroscience. It transforms acupuncture from a one-size-fits-all option into a potentially targeted approach.
In a condition defined by sudden, unwelcome pain, predictability is powerful. The idea that a brain scan might forecast relief offers hope grounded in data, not wishful thinking.
For those living with migraine without aura, fewer days lost to throbbing pain is more than a statistic. It is time returned. It is movement regained. It is life, less interrupted.
Study Details
Xinyu Zhang et al, Acupuncture for Migraine Without Aura and Connection-Based Efficacy Prediction, JAMA Network Open (2026). DOI: 10.1001/jamanetworkopen.2025.55454