What is disease? At first glance, the answer seems deceptively simple: disease is the presence of illness, of something going wrong within the body. But the deeper we probe into this question—scientifically, philosophically, and biologically—the more elusive and complex the definition becomes. Disease is not just a collection of symptoms, pathogens, or malfunctions. It’s a dynamic state—a disruption of the delicate balance that defines life.
To understand disease, we must first understand health. Health isn’t merely the absence of disease; it’s a state of homeostasis—a harmonious equilibrium where all systems of the body, from cellular metabolism to psychological well-being, are functioning in coordinated, adaptive balance. Disease emerges when this homeostasis is lost. It can be triggered by invaders from the outside world, by mutations within our own cells, by imbalances in our immune system, or by complex social and psychological stressors.
In this exploration, we’ll journey through the science of what it means to be ill—from the cellular chaos of cancer to the microscopic hijackings of viruses, from ancient beliefs about divine punishment to the latest innovations in genomic medicine. Along the way, we’ll uncover how disease has shaped human history, redefined our understanding of the body, and continually challenged the boundaries of medical science.
The Origins of Disease: Myths, Spirits, and Humors
Long before the discovery of bacteria or the invention of the microscope, disease was explained through myth and mysticism. In ancient Mesopotamia, illness was thought to be a punishment from gods or the result of demonic possession. Shamans and priests acted as intermediaries, performing rituals or offering sacrifices to restore divine favor.
The ancient Greeks offered a more systematic, though still speculative, interpretation. Hippocrates, often called the “father of medicine,” proposed the theory of the four humors: blood, phlegm, black bile, and yellow bile. Health was the balance of these humors, while disease was caused by their imbalance. Treatments included bleeding, purging, or special diets—an early attempt at evidence-based intervention, albeit without the tools of modern science.
In China, traditional medicine revolved around qi (life energy), and disease was seen as a disruption of this vital flow. In India, Ayurvedic medicine described disease as an imbalance of three doshas—vata, pitta, and kapha—energetic forces that governed the body.
These ancient systems were profound in their time, not because they were accurate by today’s standards, but because they represented humanity’s first attempts to systematize illness—to describe its patterns, its triggers, and its treatments. They paved the way for scientific inquiry by making disease a phenomenon that could be observed, discussed, and addressed.
Pathogens: The Microscopic Puppet Masters
The true breakthrough in understanding disease came with the invention of the microscope in the 17th century and the emergence of germ theory in the 19th. Suddenly, the invisible agents of disease were made visible. Scientists like Louis Pasteur and Robert Koch demonstrated that specific microbes caused specific diseases. Tuberculosis wasn’t a curse—it was the work of Mycobacterium tuberculosis. Cholera wasn’t bad air—it was Vibrio cholerae. The modern age of infectious disease had begun.
Microbes are diverse and ingenious. Bacteria, viruses, fungi, and parasites all have unique strategies for invading the body and reproducing. Some, like Streptococcus pneumoniae, hitch a ride on droplets in the air. Others, like malaria, need insect vectors. Still others, like HIV, use body fluids to spread between hosts.
Viruses, arguably the most enigmatic pathogens, aren’t even alive in the traditional sense. They’re strands of genetic material encased in protein, incapable of reproduction without hijacking a host cell’s machinery. Once inside, they rewrite the cell’s genetic instructions, turning it into a viral factory.
Yet not all microbes are harmful. Our bodies teem with trillions of microbes—our microbiome—which play essential roles in digestion, immunity, and even brain function. Disease occurs not simply because microbes are present, but because balance is lost. An overgrowth of Clostridioides difficile, for example, can wreak havoc in the gut after antibiotics wipe out competing bacteria. Once again, we return to the theme of equilibrium.
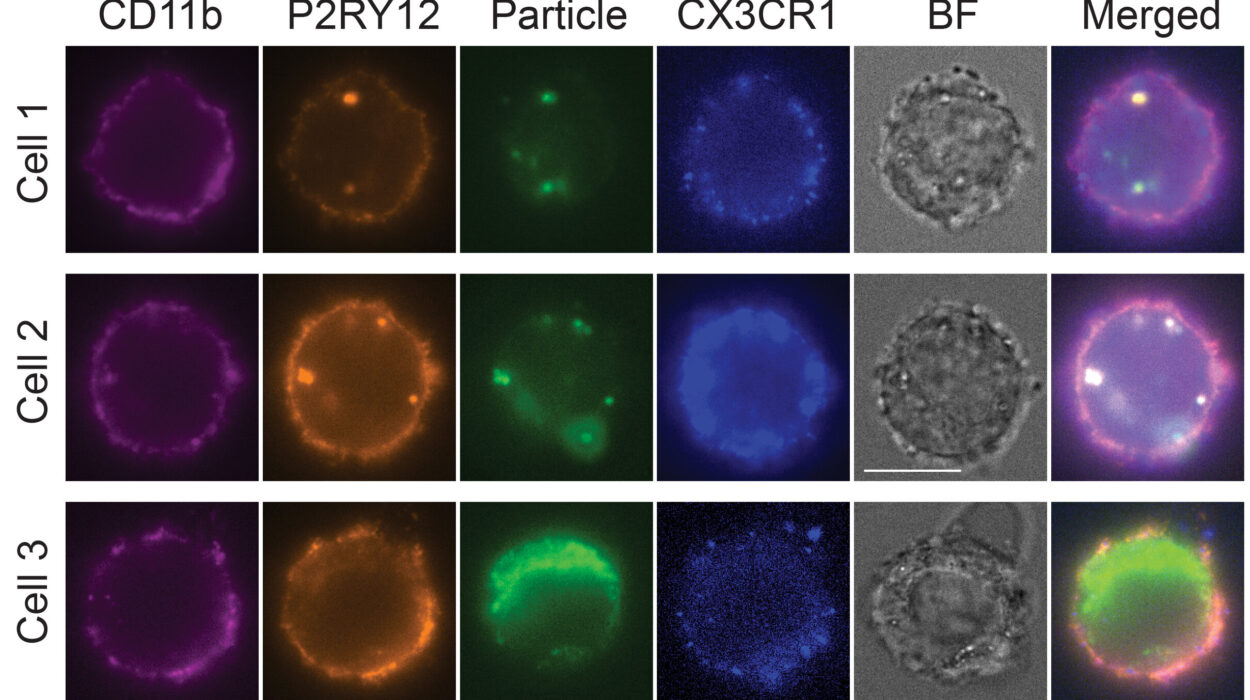
The Body’s Battlefield: Immune Warfare
When the body detects an invader or malfunction, it responds with the full force of its immune system—a complex network of cells, tissues, and signaling molecules that act as sentinels, soldiers, and assassins.
Innate immunity is our first line of defense. It includes physical barriers like skin, as well as cells like neutrophils and macrophages that attack anything unfamiliar. Adaptive immunity is more specialized. It involves T cells and B cells that recognize specific pathogens, remember them, and respond faster upon re-exposure.
However, the immune system is a double-edged sword. It can become hyperactive, attacking not just invaders but the body’s own tissues. This leads to autoimmune diseases like lupus, multiple sclerosis, and rheumatoid arthritis—where the immune system becomes the source of disease rather than its cure.
There are also cases of immunodeficiency, where the immune system is too weak to function. This can be genetic, as in severe combined immunodeficiency (SCID), or acquired, as in AIDS. These conditions leave the body vulnerable to opportunistic infections that would normally be harmless.
And in an age of pandemics and vaccine breakthroughs, the immune system has taken center stage in public consciousness. We’ve learned that immunity isn’t just about biology—it’s about memory, timing, regulation, and risk.
The Genetic Machinery of Malfunction
Some diseases are encoded in our DNA from the very beginning. Genetic diseases arise from mutations—changes in the DNA sequence—that disrupt normal development or cellular function. These can be inherited, as in cystic fibrosis or sickle cell anemia, or they can arise spontaneously, as in many forms of cancer.
Cancer, in particular, is not a single disease but a family of diseases characterized by uncontrolled cell growth. It arises when mutations accumulate in genes that regulate the cell cycle. Tumor suppressor genes fail. Oncogenes activate inappropriately. The result is cellular rebellion—a population of cells that no longer obeys the rules.
Cancer is also a disease of time. Our cells are constantly dividing, and with each division comes the risk of copying errors. Over decades, exposure to carcinogens, random mutations, and aging itself all increase the likelihood that cancer will arise. It is, in a way, the price we pay for complex, multicellular life.
But genetics also opens the door to precision medicine. With technologies like CRISPR and next-generation sequencing, we can now identify the genetic fingerprints of disease and tailor treatments to the individual patient. We are entering an era where medicine is not just reactive, but predictive.
Diseases of Civilization: When Progress Backfires
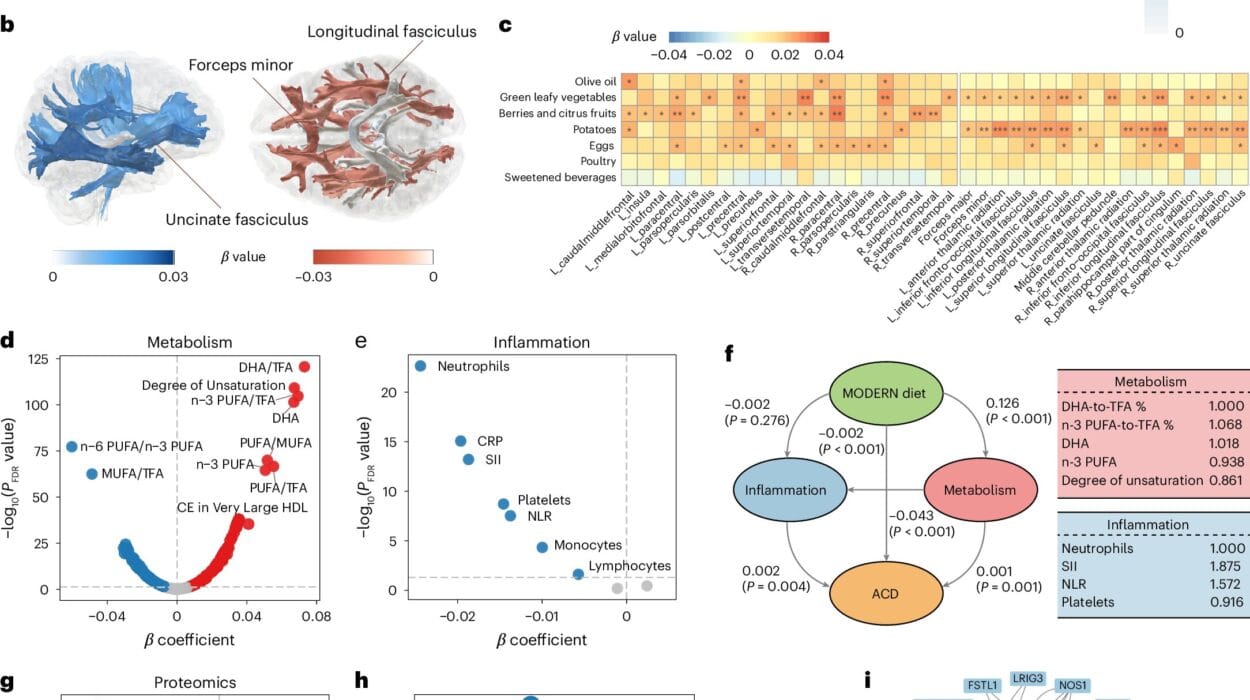
Some of the most pervasive diseases today are not caused by microbes or mutations, but by modern lifestyles. Cardiovascular disease, type 2 diabetes, obesity, and some cancers are heavily influenced by diet, exercise, sleep, and stress. These are sometimes called “diseases of affluence” or “lifestyle diseases,” but this framing can obscure their deeper complexity.
Yes, processed foods, sedentary behavior, and chronic stress play a role—but so do genetics, environment, and social inequality. Poverty is a major predictor of chronic disease, not because the poor make bad choices, but because they have fewer choices. Food deserts, lack of access to healthcare, and occupational hazards create a landscape where disease flourishes.
Moreover, the mind and body are not separate entities. Depression, anxiety, and trauma can have profound physiological effects—altering immune function, hormone levels, and even gene expression. Chronic stress increases the risk of heart disease. Social isolation impairs healing. The field of psychosomatic medicine reminds us that disease is not just biological—it is deeply human.
The Ecology of Epidemics and the Age of Global Disease
Throughout history, disease has not only shaped individual lives but entire civilizations. The Black Death in the 14th century killed a third of Europe’s population. Smallpox devastated Indigenous peoples in the Americas. The 1918 flu pandemic claimed more lives than World War I.
In the 21st century, epidemics travel faster than ever. Globalization means a virus can circle the planet in a day. The COVID-19 pandemic revealed just how interconnected—and vulnerable—our species has become. But it also highlighted the power of science to respond with unprecedented speed. Within months, researchers identified the virus’s genome and began developing vaccines based on mRNA technology.
Epidemiology—the study of how diseases spread—has become a critical science in an age of emerging infections. It combines biology with data science, public health, and social behavior to understand the patterns of disease and design strategies for containment.
But controlling disease is not just about vaccines or antibiotics. It’s also about trust, communication, infrastructure, and equity. The fight against disease is as much about social fabric as it is about molecular mechanisms.
From Symptom to Syndrome: The Changing Language of Diagnosis
How do we know we are sick? Often, it begins with symptoms—fever, fatigue, pain, dizziness. But symptoms are only the surface. Diagnosing a disease requires connecting those dots to an underlying mechanism, a root cause.
Medical diagnosis has evolved from stethoscopes and blood tests to sophisticated imaging techniques and molecular assays. We can now scan the brain in real time, sequence tumor DNA, or detect a virus from a single drop of blood.
But not all diseases are easily diagnosed. Some, like chronic fatigue syndrome or fibromyalgia, present with vague, subjective symptoms and no clear biomarkers. Others, like mental illnesses, are diagnosed through behavioral criteria rather than physical tests. This blurs the line between disease and disorder, between pathology and variation.
Moreover, cultural and historical biases influence what we define as disease. Homosexuality was once listed as a mental illness. Female hysteria, a catch-all diagnosis for “unruly” women, reflected more about gender norms than biology. Even today, race-based medical assumptions can lead to misdiagnosis and undertreatment.
Disease, then, is not just a scientific category—it’s a cultural one. It reflects our values, our prejudices, and our evolving understanding of the body.
Healing and the Limits of Medicine
If disease is the disruption of biological harmony, then healing is its restoration. Medicine has made extraordinary strides in treating disease—antibiotics for infection, insulin for diabetes, chemotherapy for cancer. Organ transplants, artificial limbs, and gene therapies have extended life in ways once unimaginable.
Yet not all diseases can be cured. Some can only be managed. Others progress despite our best efforts. Palliative care, pain management, and hospice remind us that the goal of medicine is not just to prolong life, but to preserve dignity.
There is also the enduring mystery of spontaneous remission—cases where disease disappears without explanation. Such stories, though rare, challenge our understanding and offer glimpses of the body’s untapped healing capacities.
Ultimately, the practice of medicine is as much an art as it is a science. It requires empathy, intuition, and humility in the face of uncertainty.
The Future of Disease: Prediction, Prevention, and Precision
The future of disease is already being rewritten in laboratories and clinics around the world. Artificial intelligence is analyzing vast datasets to predict disease before symptoms arise. Wearable sensors are monitoring blood glucose, heart rhythms, and oxygen levels in real time. Personalized medicine is tailoring treatments based on a person’s genes, lifestyle, and environment.
Gene editing technologies like CRISPR may one day eliminate inherited diseases altogether. Microbiome engineering could prevent chronic inflammation and obesity. Synthetic biology might develop immune cells that target tumors with surgical precision.
Yet the more we learn, the more we must ask: How do we define normalcy in a world where biology can be edited? What constitutes disease when we can choose our genes? As we gain control over the biology of illness, we must confront the ethics of health itself.
Conclusion: Disease as a Mirror
To study disease is to study life under duress. It is to observe the body in crisis, the mind in pain, and the systems of society tested by biology’s unpredictability. But it is also to witness resilience—of cells, of organs, of human beings, and of entire populations.
Disease, in all its forms, reflects back to us who we are: fragile yet adaptive, vulnerable yet ingenious. It reminds us that life is not a static state but a dynamic process, constantly negotiating the line between order and chaos.
In seeking to understand disease, we do more than treat symptoms. We ask profound questions about identity, mortality, community, and the essence of being alive. In the end, the science of illness is not just about what goes wrong—it’s about what it means to heal.