Disease, in all its forms, has shadowed humanity since the dawn of civilization. From the earliest records etched on ancient tablets to the cutting-edge diagnostics of modern medicine, diseases have shaped human history, culture, and progress. Yet, the world of diseases is not a monolith; it is broadly divided into two fundamentally different realms—infectious and non-infectious diseases. This division, while seemingly simple, opens a vast window into how life on Earth interacts with microscopic invaders, lifestyle, genetics, and environmental factors.
Understanding the difference between infectious and non-infectious diseases is more than a scientific classification. It is a journey into the mechanisms of health and illness, a guide to how we prevent, treat, and live with these conditions, and a story of how humanity fights against the unseen enemies within and outside our bodies.
Infectious Diseases: The Microscopic Invaders
Infectious diseases are the dramas of survival played out on the microscopic stage. They are caused by pathogens—tiny, often invisible agents such as bacteria, viruses, fungi, and parasites—that invade the body, multiply, and disrupt normal function. This invasion triggers the body’s defense system, setting off a cascade of symptoms as it battles to expel the invader.
These diseases are the product of a biological conflict, a battlefield where survival means either the eradication or the control of the intruder. Their spread can be swift and sweeping. Some infectious diseases can move from person to person like wildfire, carried through the air, water, bodily fluids, or vectors like mosquitoes. Others remain contained, infecting only the most vulnerable or those exposed through specific environmental factors.
Throughout history, infectious diseases have shaped human destiny. The bubonic plague, smallpox, tuberculosis, and influenza epidemics decimated populations, altered empires, and shaped cultural practices around hygiene and medicine. Even today, infectious diseases such as HIV/AIDS, malaria, and emerging viral infections like COVID-19 command global attention and resources.
But what exactly sets infectious diseases apart? It is the presence of a living, replicating agent that can be transmitted. The pathogen is the key. Without it, no infection can occur. This biological invader triggers the disease process by hijacking cells, releasing toxins, or provoking an overzealous immune response that damages tissues.
The Machinery of Infection: How Pathogens Strike
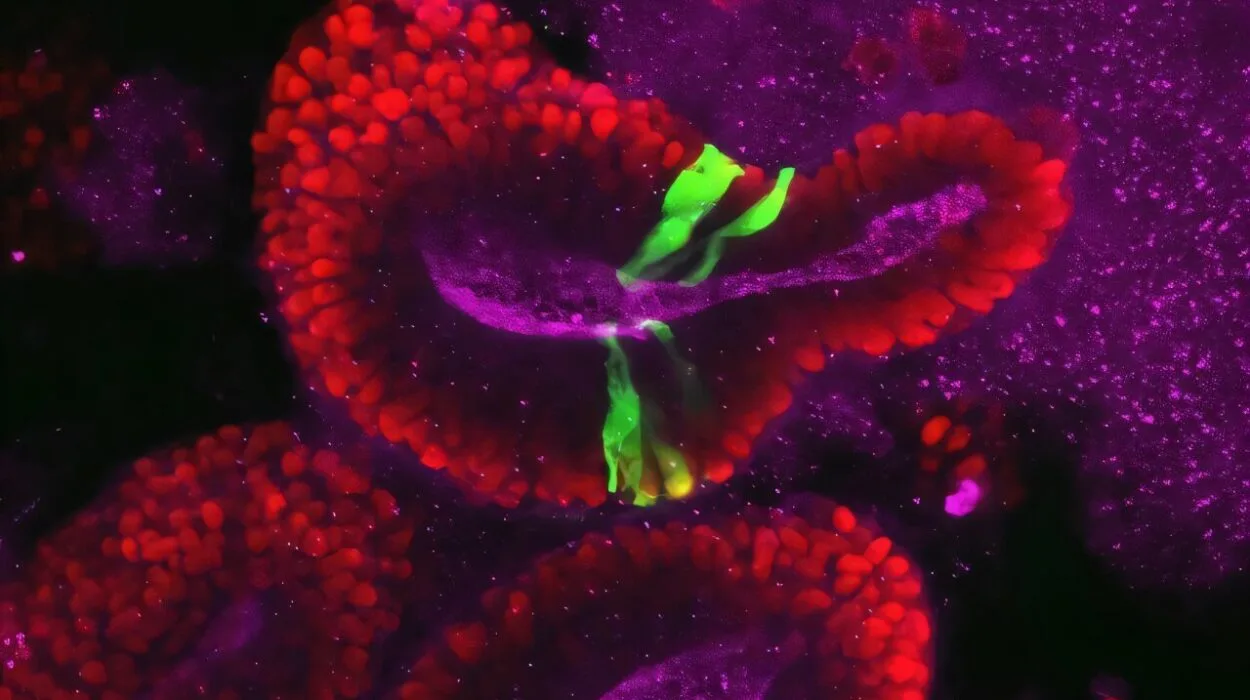
The journey of an infectious disease begins with exposure. Pathogens must breach the body’s natural barriers—the skin, mucous membranes, and immune defenses. Some pathogens are cunning masters of disguise and evasion. Viruses, for example, infiltrate host cells and use the cell’s own machinery to reproduce, often killing the host cell in the process.
Bacteria can release powerful toxins that disrupt cellular processes or directly invade tissues. Parasites, ranging from microscopic protozoa to larger worms, have complex life cycles and often manipulate their hosts’ immune systems to survive and thrive.
Transmission routes vary widely. Respiratory droplets can carry influenza or tuberculosis from one cough to the next host’s lungs. Contaminated water or food can harbor cholera bacteria or hepatitis viruses. Sexual contact spreads HIV and other infections. Insects like mosquitoes transmit malaria parasites and Zika virus. The pathogen’s mode of entry shapes the disease’s pattern and the strategies humans develop to combat it.
Once inside, the body mounts an immune response. Fever, inflammation, fatigue, and pain are not just symptoms—they are the battle cries of the immune system. While many infections are acute and self-limiting, some become chronic or latent, lying dormant until conditions favor reactivation. Tuberculosis and herpes are notorious for this stealth.
Non-Infectious Diseases: The Silent Disruptors
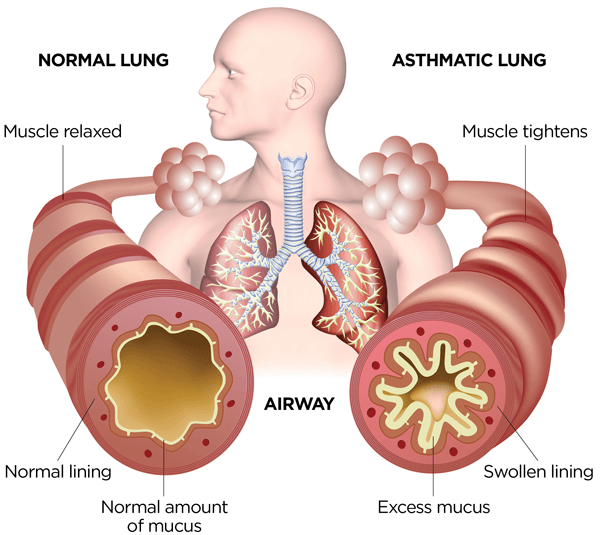
Non-infectious diseases, by contrast, are conditions not caused by invading pathogens. They arise from within—the body’s own cells, genetic blueprint, environmental exposures, or lifestyle choices. These diseases encompass a wide range of ailments, from heart disease and diabetes to cancer, asthma, and autoimmune disorders.
While infectious diseases represent a battle against external invaders, non-infectious diseases often reflect an internal imbalance or malfunction. They may develop slowly over years, silently eroding health and function, often without the dramatic onset that characterizes infections.
Unlike infectious diseases, non-infectious diseases cannot be transmitted from person to person. They are not contagious. Instead, their causes are multifactorial, frequently involving complex interactions between genetics, environment, diet, physical activity, stress, and other factors. For instance, cardiovascular diseases are driven by a combination of genetic predisposition, unhealthy diets, smoking, and sedentary lifestyles.
The rise of non-infectious diseases is closely linked to modernization, urbanization, and increased life expectancy. As infectious diseases have come under better control with vaccines, antibiotics, and improved sanitation, chronic non-infectious diseases have become the leading cause of death globally.
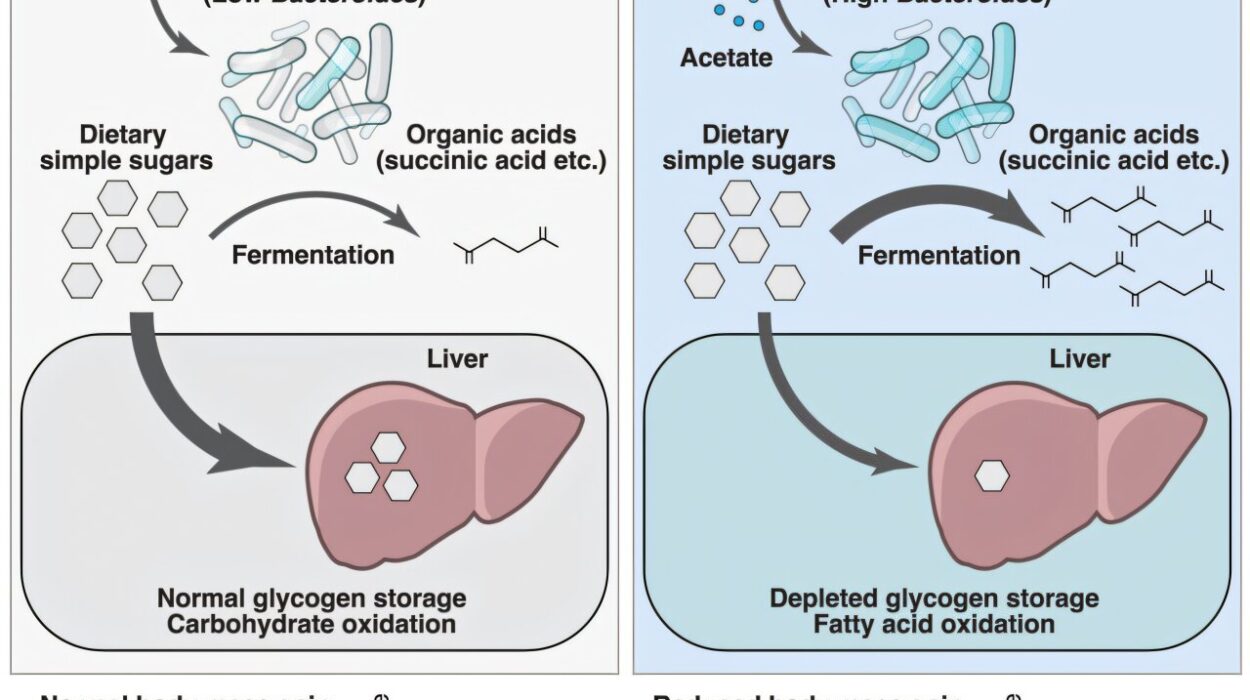
The Biology Behind Non-Infectious Diseases
The biological underpinnings of non-infectious diseases vary widely. In genetic disorders such as cystic fibrosis or sickle cell anemia, mutations in specific genes disrupt normal protein function, leading to lifelong illness. Cancer arises from uncontrolled cellular growth caused by mutations and environmental insults like radiation or carcinogens.
Autoimmune diseases such as lupus and rheumatoid arthritis occur when the immune system mistakenly attacks the body’s own tissues. Metabolic diseases like diabetes result from disruptions in the body’s ability to regulate blood sugar and insulin.
Environmental toxins, pollutants, and lifestyle factors contribute heavily to many non-infectious diseases. Smoking, for instance, is linked to lung cancer, chronic obstructive pulmonary disease (COPD), and heart disease. Obesity, influenced by diet and activity, increases the risk of hypertension, stroke, and type 2 diabetes.
Unlike infectious diseases, which can be cured or eradicated through targeting the pathogen, many non-infectious diseases require long-term management and lifestyle modification. Prevention often revolves around minimizing risk factors and early detection.
Symptoms and Diagnosis: How Diseases Declare Themselves
Both infectious and non-infectious diseases manifest symptoms, but the nature and progression often differ. Infectious diseases tend to present more acutely—fever, chills, cough, diarrhea, and localized pain are common signs. Because the cause is an invading organism, diagnostic tests frequently include cultures, blood tests for antibodies or antigens, and imaging to locate abscesses or pneumonia.
Non-infectious diseases often present gradually. Chest pain or shortness of breath may indicate heart disease; weight loss or lumps can suggest cancer. Diagnosing non-infectious diseases may involve blood tests for markers of organ function or inflammation, genetic testing, biopsies, and imaging to detect structural changes.
Both categories require medical expertise for diagnosis, but the diagnostic approaches highlight their fundamental differences. Infectious disease diagnosis often focuses on identifying and eliminating the culprit pathogen, whereas non-infectious disease diagnosis emphasizes identifying physiological abnormalities or genetic predispositions.
Treatment and Management: Fighting the Different Battles
The treatment landscapes for infectious and non-infectious diseases reflect their distinct causes. Infectious diseases can often be cured or controlled by targeting the pathogen itself. Antibiotics destroy bacteria, antivirals interfere with viral replication, antifungals eradicate fungi, and antiparasitic medications target parasitic worms or protozoa.
Vaccines have revolutionized infectious disease control, preventing illnesses like polio, measles, and influenza by training the immune system to recognize and eliminate pathogens before they cause disease.
However, the rise of antibiotic resistance poses a growing threat, turning some infections into persistent challenges and reminding us that the battle with pathogens is ongoing.
Non-infectious diseases demand different strategies. While some can be cured—such as certain cancers treated by surgery or chemotherapy—many require long-term management. Lifestyle changes like diet modification, exercise, quitting smoking, and controlling blood pressure play crucial roles.
Medications to control symptoms or slow disease progression are common. Insulin for diabetes, statins for high cholesterol, immunosuppressants for autoimmune diseases, and inhalers for asthma exemplify treatments that manage rather than cure.
Emerging therapies, including gene editing and personalized medicine, offer hope for more precise interventions tailored to individual genetic and environmental factors.
Prevention: The Power of Knowledge and Behavior
Prevention of infectious diseases has been one of humanity’s greatest triumphs. The development of clean water supplies, sanitation systems, vaccines, and antibiotics transformed public health. Hygiene practices like handwashing, quarantine, and mosquito control remain frontline defenses against many infections.
Non-infectious disease prevention, by contrast, is often rooted in lifestyle and environmental changes. Public health campaigns promote healthy eating, physical activity, tobacco cessation, and reduced alcohol consumption to prevent heart disease, diabetes, and cancer.
Understanding social determinants—like income, education, and access to healthcare—is crucial in addressing both types of diseases. Inequities often lead to disparities in disease burden, with marginalized populations suffering disproportionately.
The Interplay: When Infectious Meets Non-Infectious
Although these two categories seem distinct, they often intersect. Infectious diseases can trigger or exacerbate non-infectious conditions. For example, chronic infections with hepatitis B or C viruses can lead to liver cancer. Human papillomavirus (HPV) infection is linked to cervical and other cancers.
Conversely, non-infectious diseases can impair immune function, increasing vulnerability to infections. Diabetes and cancer patients are more prone to infections due to compromised immunity.
This interplay complicates diagnosis and treatment, requiring integrated approaches that consider the full spectrum of a patient’s health.
Global Challenges and the Future
As the world changes, so too do the challenges posed by infectious and non-infectious diseases. Climate change, urbanization, and globalization influence the spread of infectious diseases, introducing pathogens into new regions and populations.
At the same time, aging populations and lifestyle shifts increase the burden of non-infectious chronic diseases. The dual challenge of managing both infectious outbreaks and chronic conditions strains healthcare systems worldwide.
Advances in genomics, immunology, and technology hold promise for better diagnostics, treatments, and prevention strategies. The COVID-19 pandemic underscored the importance of global cooperation, rapid response, and investment in science to combat infectious threats.
Meanwhile, tackling the non-infectious disease epidemic requires broad social, economic, and policy changes, including healthier environments, equitable healthcare access, and education.
A Shared Story of Resilience and Innovation
Ultimately, the stories of infectious and non-infectious diseases are stories of human resilience. They reveal how life adapts and persists amid constant threats, how knowledge evolves from ancient wisdom to modern science, and how the quest to understand and conquer disease continues to drive innovation.
Both infectious and non-infectious diseases challenge us to look beyond symptoms to root causes, beyond individual health to social and environmental factors. They compel us to think globally, act locally, and embrace complexity.
As we continue this journey, the lessons from both realms remind us that health is not just the absence of disease but the presence of balance, harmony, and an ever-curious spirit to explore the unknown.