Yeast infections are incredibly common, affecting up to 75% of women at least once in their lifetime. And yet, despite how widespread they are, they remain something we often whisper about or bury beneath discomfort and embarrassment. Whether it’s your first time or your fifth, the burning, itching, and irritation can feel not only physically overwhelming but emotionally frustrating too. Understanding yeast infections isn’t just about knowing how to treat them—it’s about learning how to prevent them, recognize them early, and take back control of your body with confidence and calm.
Yeast infections are not a reflection of poor hygiene or carelessness. They’re the result of a delicate internal ecosystem being thrown off balance. And the more we understand that ecosystem, the better we can support it. So, let’s take a journey into the world of yeast infections—why they happen, how to prevent them, and how to treat them in ways that actually work.
What Is a Yeast Infection, Really?
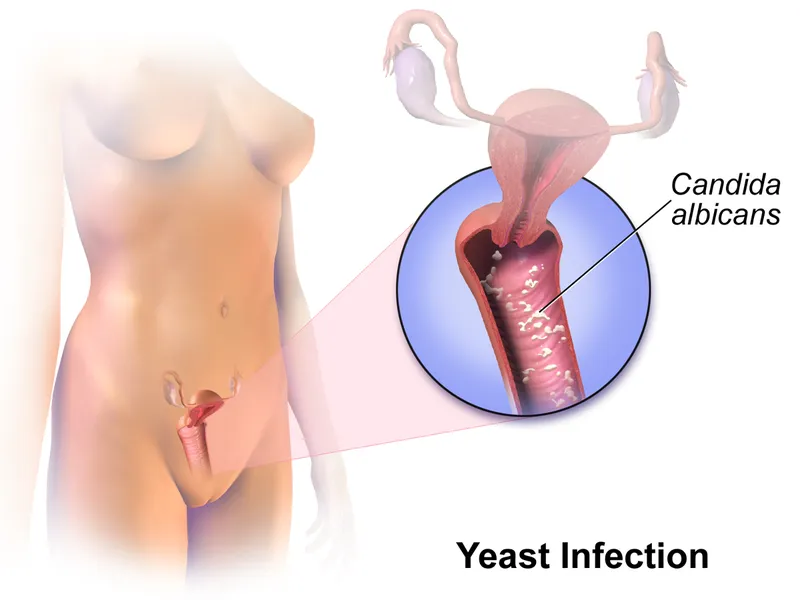
At the heart of every yeast infection is a microscopic organism called Candida. Candida is a type of fungus that naturally lives in small amounts in various parts of the body, including the mouth, digestive tract, and yes—the vagina. Under normal circumstances, Candida coexists peacefully with other microbes. The vaginal environment, in particular, is home to a complex and fascinating mix of bacteria and yeast, all working together to keep each other in check.
When this natural balance is disrupted, however, Candida can grow out of control. That overgrowth leads to the familiar symptoms of a yeast infection: itching, redness, swelling, a thick white discharge that resembles cottage cheese, and sometimes even painful urination or intercourse. In medical terms, this condition is known as vulvovaginal candidiasis.
It’s important to note that while Candida albicans is the most common strain behind yeast infections, there are other species like Candida glabrata that can be more stubborn and less responsive to standard treatments. Knowing the exact type isn’t always necessary for mild cases, but recurrent or persistent infections may require a closer look.
What Causes an Overgrowth of Candida?
Several factors can tip the balance in favor of Candida. Antibiotics are among the most common triggers because they don’t discriminate between “good” and “bad” bacteria. By killing off beneficial lactobacilli—the bacteria that help keep Candida in check—antibiotics create a perfect opportunity for yeast to multiply.
Hormonal changes are another major influence. Estrogen, in particular, plays a big role in vaginal health. Fluctuations due to pregnancy, birth control, hormone replacement therapy, or even the menstrual cycle can make the environment more hospitable to yeast. That’s why some women notice a pattern of developing yeast infections at specific points in their cycle or during pregnancy.
Diet also plays a supporting role. High sugar intake can feed yeast and contribute to overgrowth, while processed foods and refined carbs may weaken your body’s defenses. Tight, non-breathable clothing—especially synthetic underwear or wet swimsuits—can trap moisture and heat, which yeast absolutely loves.
Stress and lack of sleep don’t help either. A taxed immune system is less effective at keeping yeast in check. And certain medical conditions, such as diabetes or immunosuppressive disorders, can make a person more susceptible to recurring infections.
When It’s Not a Yeast Infection
One of the trickiest things about yeast infections is that their symptoms can mimic those of other conditions. Bacterial vaginosis, trichomoniasis, and even some sexually transmitted infections can cause similar itching, discharge, and discomfort. Using an over-the-counter antifungal when the problem isn’t yeast won’t help—and could even make things worse.
That’s why it’s essential to get a proper diagnosis, especially if it’s your first infection, symptoms are severe, or nothing seems to be working. A quick visit to your healthcare provider can involve a swab or microscopic test to confirm what’s going on. Self-diagnosing is tempting, but it’s always best to be sure.
Preventing Yeast Infections Begins with Everyday Habits
You can’t live in a bubble, and you shouldn’t have to give up every pleasurable thing in life just to avoid a yeast infection. But you can stack the odds in your favor by supporting your body’s natural defenses.
Start with your underwear drawer. Cotton is your best friend when it comes to breathability. Synthetic fabrics like nylon or polyester can trap moisture, while cotton allows airflow and helps keep you dry. Thong lovers, beware—tight styles can create friction and transfer bacteria, especially during exercise.
After workouts or swimming, try to change out of damp clothing as soon as possible. Lingering in sweaty leggings or a wet bikini creates a warm, moist environment that yeast thrives in. The same goes for sleeping in underwear—going commando at night can help your skin breathe and reduce irritation.
Be mindful of soaps, douches, and scented products. The vagina is self-cleaning and doesn’t need internal cleansing. In fact, douching can strip away protective bacteria and increase your risk of infection. Stick to gentle, fragrance-free cleansers for the vulva (external area) only, and avoid anything marketed as “feminine hygiene” with strong perfumes or additives.
Diet also matters more than you might think. A balanced diet rich in leafy greens, lean proteins, healthy fats, and fermented foods can help support your immune system and keep your microbiome thriving. Yogurt with live cultures, kefir, sauerkraut, and other probiotics introduce beneficial bacteria into your gut and vaginal environment. Limiting added sugars and processed carbs can also starve yeast of its favorite fuel.
The Role of Probiotics in Prevention
Probiotics are live microorganisms that can offer health benefits by improving or restoring the gut flora. While we often associate them with gut health, they also play a role in vaginal health. Certain strains of lactobacilli produce hydrogen peroxide, which creates an acidic environment that yeast finds inhospitable.
Probiotic supplements, particularly those targeted for vaginal health, can be especially helpful if you’ve taken antibiotics or have a history of recurrent infections. Look for strains like Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14, which have been studied for their ability to reduce yeast infections and support a healthy vaginal microbiome.
Some women also opt for vaginal probiotic suppositories or inserts, although research on their effectiveness is still growing. Talk to your healthcare provider before starting a new regimen, especially if you’re pregnant, immunocompromised, or have underlying health concerns.
Treating a Yeast Infection at Home
For many women, over-the-counter treatments can provide fast relief. Antifungal creams, ointments, or suppositories are available at most pharmacies and can be used for three to seven days, depending on the product. Common active ingredients include miconazole and clotrimazole.
While these treatments are effective for mild to moderate yeast infections, they can be messy and sometimes cause irritation. If you prefer a one-and-done approach, oral antifungal pills like fluconazole (Diflucan) are available by prescription and can treat infections with a single dose. However, these are not suitable for everyone, especially during pregnancy or in people with liver conditions.
Natural remedies have gained popularity, though they should be approached with caution. Coconut oil, tea tree oil, and boric acid are often touted as yeast-fighting options, but not all of them are safe for internal use or supported by strong scientific evidence. Boric acid, for example, may help with recurrent or resistant yeast infections but must be used exactly as directed and never during pregnancy.
If symptoms persist after treatment, or if they return frequently, it’s time to dig deeper. You may need a longer course of antifungal therapy, a different medication targeting a resistant strain, or testing to rule out other causes.
Recurrent Infections: A Deeper Dive
Having one or two yeast infections a year is annoying, but relatively normal. When they happen four or more times annually, it’s considered recurrent vulvovaginal candidiasis—a frustrating and often misunderstood condition.
Recurrent infections can stem from unresolved underlying causes, such as hormonal imbalances, poorly controlled diabetes, chronic antibiotic use, or immune system dysfunction. Sometimes, they occur for reasons that are harder to pinpoint.
Managing recurrent yeast infections often requires a multi-faceted approach. This may involve extended antifungal therapy—such as weekly fluconazole for several months—along with lifestyle changes, dietary shifts, and the use of probiotics. In some cases, your healthcare provider may culture the yeast to determine its specific strain and resistance pattern, which can guide more effective treatment.
It’s also worth looking at triggers beyond the obvious. Does an infection reliably show up after sex, antibiotic use, or before your period? Keeping a symptom diary can reveal patterns and help you and your provider tailor a prevention strategy that fits your body.
Sex and Yeast Infections: What You Should Know
Yeast infections aren’t classified as sexually transmitted infections (STIs), but sex can play a role in their development. Intercourse can disrupt the vaginal pH, introduce new microbes, or cause friction that leads to microtears—giving yeast a chance to flourish.
Semen is slightly alkaline, which can temporarily raise vaginal pH and create a more hospitable environment for yeast. Certain lubricants, condoms with spermicides, or even flavored products can also contain additives that irritate sensitive skin and alter the microbiome.
While you can’t “catch” a yeast infection from your partner, Candida can be transferred during sex, especially if your partner has an oral or genital yeast issue. This is more likely in people with weakened immune systems or those using antibiotics.
If you suspect a connection between your sex life and yeast infections, consider using barrier protection, switching to pH-balanced or natural lubricants, and encouraging your partner to get checked if they have any symptoms. Communication, as always, is key.
Pregnancy, Menopause, and Other Hormonal Changes
Pregnancy increases your risk for yeast infections because of hormonal shifts and changes in vaginal secretions. Estrogen levels soar, which increases glycogen—a sugar that feeds yeast. Pregnant women are often more prone to infections in the second and third trimesters, even if they’ve never had one before.
Treating yeast infections during pregnancy should always be done under medical supervision. Oral antifungals are typically avoided, and topical treatments are preferred. The good news is that most infections are easily treated and don’t pose a serious risk to the baby, although severe or untreated cases may lead to discomfort during delivery.
Menopause, on the other hand, brings a different challenge. As estrogen levels drop, the vaginal walls thin and lose elasticity, and natural lubrication decreases. These changes can make the area more susceptible to irritation and infection. Using estrogen creams, vaginal moisturizers, or other therapies recommended by a healthcare provider can help restore balance.
Breaking the Cycle and Healing Long-Term
Healing from a yeast infection isn’t just about killing the yeast—it’s about restoring balance. That means rebuilding your microbiome, identifying and avoiding triggers, and giving your body the support it needs to thrive.
It also means listening to your body, especially if something feels off. Ignoring recurring symptoms or repeatedly using the same over-the-counter treatment without improvement can lead to resistance or chronic irritation.
Creating a health routine that supports your immune system, nourishes your microbiome, and respects the unique needs of your body is the best long-term strategy. And remember, you’re not alone—many women struggle with these infections, and talking about them openly is the first step to finding solutions that work.
Final Thoughts: Empowered, Not Embarrassed
Yeast infections may be common, but that doesn’t make them any less frustrating. Fortunately, they’re also manageable—especially when you’re equipped with the right knowledge. Whether you’re trying to prevent your first infection or stop a recurring cycle, understanding how your body works is the most powerful tool you have.
Don’t let embarrassment hold you back from seeking help or exploring solutions. Vaginal health is a vital part of overall well-being, and it deserves the same care, attention, and respect as any other part of your body. By staying informed, proactive, and compassionate with yourself, you can navigate yeast infections with confidence—and help break the stigma around this all-too-common condition.