Beneath the surface of your awareness—and sitting right on the surface of your skin—lives a teeming metropolis of microscopic life. These organisms are not intruders. They are not foreign agents that happen to take up residence while we sleep. They are as much a part of our biology as the skin they live on. This community, known as the skin microbiome, is a dynamic, intricate, and deeply essential aspect of human health that science is only beginning to fully understand.
A Living Barrier: The Skin as an Ecosystem
The human skin is often thought of as a barrier—a wall between the body and the outside world. But that description, while partially true, is far too simplistic. The skin is not just a passive shield; it is an active, responsive, and living organ that hosts one of the most diverse microbial ecosystems found anywhere on the human body.
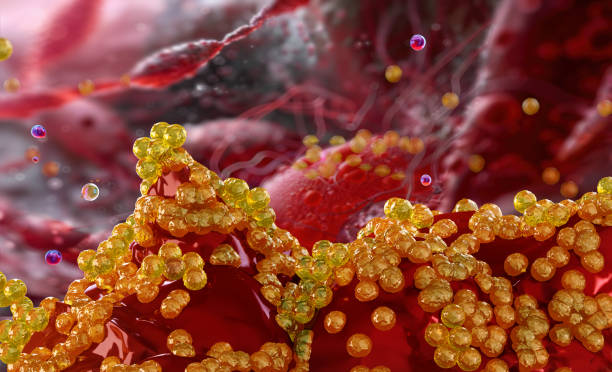
Each square centimeter of your skin harbors millions of bacteria, viruses, fungi, and even microscopic mites. These microorganisms don’t simply sit idly on the surface; they interact constantly with each other and with your body’s immune system. Their influence extends from maintaining skin hydration to training your immune system and even affecting your mood and behavior through complex signaling networks.
This invisible world is what we refer to as the skin microbiome, and it plays an indispensable role in keeping you healthy, protecting you from infection, and influencing the way your body interacts with its environment.
Meet the Microbes: Who Lives on Your Skin?
The skin microbiome is not a single entity, nor is it uniform. It is composed of thousands of microbial species that differ depending on where on the body you look. The oily regions of the face, the dry expanses of the forearms, the moist creases behind the knees—all of these micro-environments host different microbial communities adapted to thrive under specific conditions.
The most commonly found inhabitants include bacteria, such as Staphylococcus, Cutibacterium acnes (formerly Propionibacterium acnes), and Corynebacterium. Alongside these are fungi like Malassezia, which are especially prevalent in oily areas. There are also viruses, including bacteriophages that infect bacteria, and mites like Demodex folliculorum, which nestle into hair follicles and sebaceous glands.
Each type of microbe contributes uniquely to the skin ecosystem. Some help produce molecules that keep harmful invaders at bay. Others consume excess oil and dead skin cells. Some communicate directly with the skin’s immune cells, helping them recognize which microbes are friendly and which are threats.
Together, this complex community forms a symbiotic partnership with the human body. In many ways, it acts like a living extension of the skin itself.
Microbial Fingerprints: Everyone’s Skin Microbiome Is Unique
Just as no two people have the same fingerprint, no two individuals have the same skin microbiome. Your microbial signature is shaped by a dazzling array of factors, beginning at birth. Babies born vaginally receive a different microbial inheritance than those born via cesarean section. Breastfeeding, antibiotic use, environment, and even the pets in your home all contribute to shaping your skin microbiome in infancy and beyond.
As we age, our microbiome continues to evolve. Hormonal changes, diet, hygiene habits, climate, stress levels, and cosmetic products all influence the composition and diversity of the microbes that call your skin home.
Interestingly, even different parts of your own body can have vastly different microbial communities. Your forehead and your foot, despite both being parts of the same organism, are as different microbiologically as a rainforest and a desert.
This variability is not random—it reflects the ability of microbes to specialize and adapt. Some flourish in dry environments, others in moist creases, and still others in oily terrain. The result is a finely tuned, living patchwork that is constantly responding to changes in your internal and external environment.
The Skin’s Defense Force: Immune System Collaboration
One of the most fascinating aspects of the skin microbiome is its intimate relationship with the immune system. Far from being passive tenants, the microbes on your skin engage in a constant dialogue with your immune cells. This relationship is complex, nuanced, and, more often than not, beneficial.
When functioning properly, the skin microbiome acts like a bouncer at an exclusive nightclub—it lets in the regulars while turning away the troublemakers. Certain bacterial species, for instance, produce antimicrobial peptides that inhibit the growth of pathogenic invaders. Others help maintain the skin’s acidic pH, which is inhospitable to harmful organisms.
Moreover, the microbiome helps educate the immune system. It teaches immune cells how to distinguish between harmless microbes and those that pose a real threat. This training process is critical in preventing inflammatory diseases and allergic reactions. When this system is disrupted—whether through antibiotic use, over-sanitization, or underlying health issues—the immune system can become confused, leading to problems like eczema, psoriasis, or chronic inflammation.
In essence, your skin microbiome is not just a passive layer; it is an active participant in your body’s defense strategy.
Beauty from the Microbial Lens: Skin Health and Appearance
There is a growing recognition that skin health and appearance are closely tied to the microbiome. Traditional skincare products have often operated on the principle of elimination: destroy bacteria to clear acne, cleanse deeply to remove oil, strip the skin to “purify” it. But this approach can do more harm than good.
Many such products indiscriminately kill off beneficial microbes along with harmful ones, disrupting the delicate balance of the skin’s ecosystem. This microbial imbalance—called dysbiosis—can lead to increased sensitivity, dryness, breakouts, and accelerated aging.
A balanced and diverse microbiome, by contrast, helps the skin maintain its natural barrier function, retain moisture, and resist damage from environmental stressors. It supports wound healing, reduces inflammation, and even influences pigmentation and tone.
Skincare companies are beginning to shift toward a microbiome-friendly philosophy, creating products that support, rather than suppress, this living layer. Ingredients like prebiotics (which feed beneficial microbes), probiotics (which introduce beneficial species), and postbiotics (the beneficial compounds they produce) are at the forefront of this movement.
The emerging science suggests that true skin health—and by extension, beauty—is less about eradication and more about cultivation.
When Things Go Wrong: Dysbiosis and Disease
While the microbiome is usually a force for good, its imbalance or disruption can contribute to skin disorders. One of the most well-known examples is acne, which is linked to the overgrowth of Cutibacterium acnes in the sebaceous glands. While C. acnes is a normal part of the skin flora, certain strains can trigger inflammation, leading to clogged pores and pimples.
Eczema, or atopic dermatitis, is another condition strongly associated with microbial imbalance. People with eczema often have reduced microbial diversity and an overabundance of Staphylococcus aureus, a bacterium that can exacerbate inflammation and damage the skin barrier.
Psoriasis, rosacea, seborrheic dermatitis, and chronic wounds have all been linked in various ways to disruptions in the skin microbiome. In many cases, it’s not just a matter of one bad actor but rather a complex shift in the entire microbial community—a loss of balance that tips the scales toward disease.
The hope is that by understanding these microbial dynamics, we can develop treatments that restore harmony rather than simply fight symptoms. Already, research is exploring microbial transplants, engineered probiotics, and targeted prebiotic therapies as potential ways to treat skin conditions from the inside out.
The Microbiome and the Mind: A Two-Way Street?
The idea that your skin could talk to your brain might sound like science fiction, but it’s rapidly entering the realm of plausible science. Just as researchers have discovered a gut-brain axis, they are now exploring a skin-brain connection.
The skin is not only a sensory organ; it is also an immunological and hormonal interface. Some microbes produce neurotransmitter-like substances that could, in theory, influence mood, stress levels, and even behavior. Conversely, psychological stress can alter the composition of the skin microbiome, making the skin more vulnerable to inflammation and infection.
This bidirectional communication suggests that the skin microbiome could play a role in disorders such as stress-induced eczema or acne flares during emotional upheaval. If these connections are confirmed, they could open up revolutionary approaches to dermatology that include psychological or neurological components.
The Future of Skin Science: Personalized Microbiome Medicine
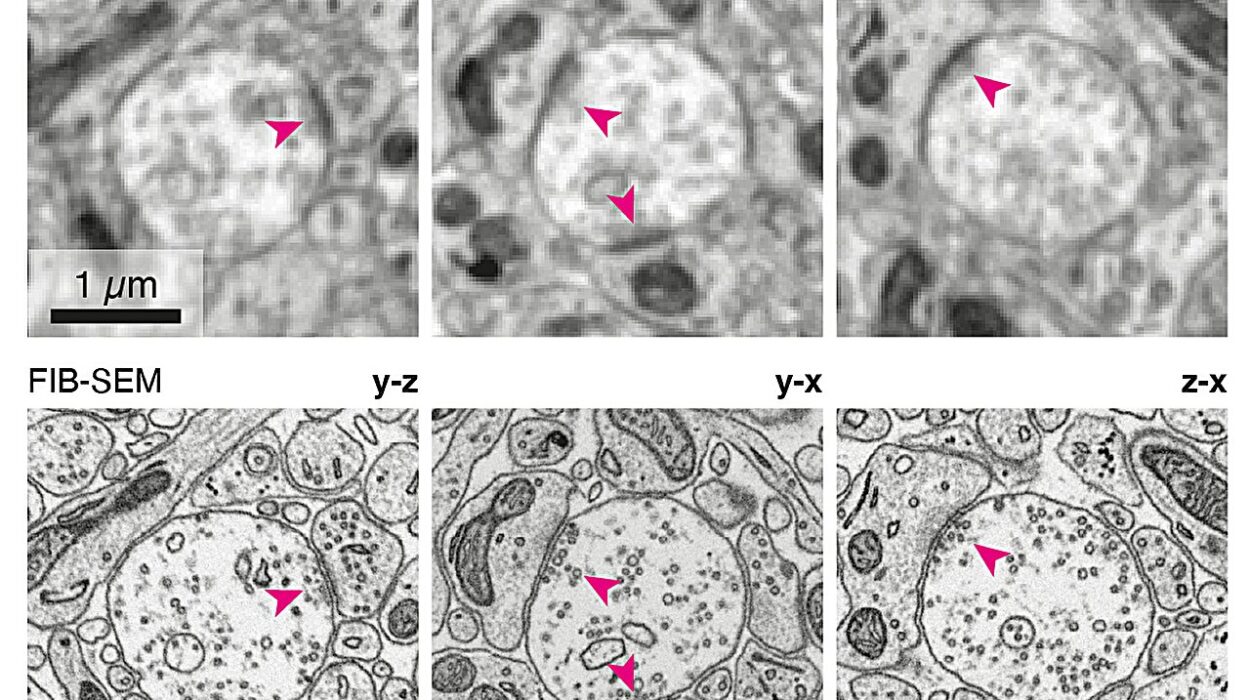
The field of microbiome research is still in its infancy, but it is advancing at a breathtaking pace. Scientists are now able to sequence microbial DNA from tiny skin swabs, analyze patterns across populations, and begin to understand the rules that govern microbial ecology.
This new frontier holds the promise of personalized skincare tailored to your individual microbiome profile. Imagine visiting a dermatologist who maps the microbial terrain of your skin and prescribes a regimen not based on your skin type alone, but on the specific bacteria and fungi living on your body.
Beyond cosmetics, this approach could lead to precision medicine for skin diseases. Instead of broad-spectrum antibiotics or steroids, future treatments might involve the targeted modulation of specific microbial populations to restore balance and health.
Even more futuristic possibilities include engineered microbes that can live on your skin and deliver therapeutic compounds on demand—an army of living, microscopic pharmacists tailored just for you.
Caring for Your Microbiome: What We Know So Far
Though much research remains to be done, there are already practical takeaways from what we’ve learned about the skin microbiome. Excessive use of harsh soaps and sanitizers can strip the skin of beneficial microbes, as can overuse of antibiotics. On the other hand, gentle cleansing, exposure to nature, and even spending time with animals may help support a healthy microbial balance.
Diet, while more often associated with the gut microbiome, can also influence the skin’s ecosystem. Anti-inflammatory foods, hydration, and nutritional balance all play indirect roles in shaping microbial health.
Just as importantly, our cultural attitudes may need to shift. Instead of viewing all microbes as enemies, we must learn to see them as ecological partners—essential collaborators in our quest for health, beauty, and resilience.
Conclusion: Embracing the Life on Your Skin
The skin microbiome represents a remarkable convergence of biology, ecology, and medicine. It forces us to reconsider long-held notions of the human body as a closed system and invites us to embrace a more holistic and dynamic view of health.
You are not just a human. You are a superorganism, a walking, breathing ecosystem whose boundaries extend far beyond your skin. The microbes that live with you, on you, and within you are not incidental; they are essential.
As science continues to peel back the layers of this invisible world, one truth becomes increasingly clear: to care for your skin is not just to moisturize or cleanse—it is to nurture an entire world.
So the next time you touch your face or feel the breeze on your arms, remember: you’re not alone. You’re in good company.