In the microscopic world where life exists beyond the boundaries of sight, bacteria reign as some of Earth’s most ancient, adaptable, and resilient inhabitants. They exist in unimaginable numbers—in soil, oceans, air, even the depths of Earth’s crust. They inhabit the human body by the trillions, forming communities in our gut, skin, mouth, and lungs. For centuries, they remained invisible. And when they were finally glimpsed under early microscopes, they were anonymous specks—living ghosts that science could barely classify or understand.
That changed in the late 19th century, thanks to a man named Hans Christian Gram. With a few drops of dye and iodine, he gave these tiny beings a passport—an identity visible under the lens. His discovery of the Gram stain would become a turning point in microbiology, forever dividing the bacterial world into two grand empires: Gram-positive and Gram-negative.
But what does that really mean? Why does a stain decide how a microbe lives, behaves, or kills? This seemingly simple categorization reflects deep, elegant differences in structure, biology, and survival strategies. And in understanding these differences, we also understand something profound about disease, medicine, and the battle for life on a microbial scale.
A Danish Doctor and a Microscopic Epiphany
In 1884, Danish physician Hans Christian Gram was working in Berlin when he devised a method to visualize bacterial cells more clearly in tissue samples. His intention was practical—he wanted a better way to identify bacteria under the microscope. He combined a violet crystal dye with iodine and alcohol, followed by a counterstain of red safranin. To his surprise, some bacteria retained the violet color, while others washed away the dye and turned pink. He had unknowingly unlocked a fundamental property of bacteria: the architecture of their cell walls.
The Gram stain, as it would be called, did more than differentiate. It opened a portal into a bacterial cell’s soul. Bacteria that retained the violet dye became known as Gram-positive. Those that did not, and instead appeared pink or red, were Gram-negative. This wasn’t a cosmetic difference—it was a reflection of the bacteria’s very blueprint, etched into the layers of their cell walls.
The Cell Wall: Fortress and Identity
To understand the significance of the Gram classification, one must start with the bacterial cell wall. This structure is no mere boundary—it is armor, scaffold, and passport. It protects the bacterium from rupture, maintains its shape, and serves as an interface with the outside world.
Gram-positive bacteria possess a thick, multilayered cell wall composed mainly of peptidoglycan—a mesh-like polymer made of sugars and amino acids. This peptidoglycan layer is so dense and rich that it traps the crystal violet stain, giving the bacteria their characteristic deep purple appearance under the microscope.
But the wall is more than peptidoglycan. Gram-positive bacteria also embed molecules called teichoic acids and lipoteichoic acids into their walls. These acids anchor the cell wall to the membrane and contribute to surface charge, ion regulation, and immune recognition. In the evolutionary arms race, these features make Gram-positive bacteria both tough and visible to host defenses.
In contrast, Gram-negative bacteria are more elusive. Their peptidoglycan layer is thin and located within the periplasmic space between two membranes—the inner plasma membrane and a unique outer membrane. This outer membrane contains lipopolysaccharides (LPS), which act like molecular barcodes and often provoke intense immune responses. The outer membrane also houses porins—protein channels that regulate what enters and exits the bacterium.
This dual-membrane design gives Gram-negative bacteria a cloak of invisibility. The outer membrane can resist many antibiotics and detergents, and it controls permeability in a way that makes these bacteria especially hard to kill.
Living on the Edge: Environmental Niches and Survival Tactics
The differences in cell wall structure shape how Gram-positive and Gram-negative bacteria live in the world. Each group has evolved strategies to suit different environments, hosts, and pressures.
Gram-positive bacteria often thrive in dry, nutrient-rich environments like the skin and soil. Their thick walls make them resistant to desiccation and mechanical stress. Species like Staphylococcus aureus and Bacillus anthracis can survive outside the body for long periods, waiting patiently for the right opportunity to infect or multiply. Some, like Clostridium difficile, form spores that are nearly indestructible—able to resist heat, chemicals, and even radiation.
Gram-negative bacteria, on the other hand, dominate moist environments like the gastrointestinal tract, water systems, and hospital sinks. Their outer membrane gives them the upper hand in chemical resistance, allowing them to resist bile salts, antibiotics, and immune molecules. Escherichia coli, Salmonella, Pseudomonas aeruginosa, and Neisseria gonorrhoeae are all notorious Gram-negative pathogens that have turned this structural complexity into biological power.
Pathogenesis: How Bacteria Cause Disease
When bacteria cause disease, they do so by breaching barriers, multiplying rapidly, and evading or manipulating the host’s immune system. The structural differences between Gram-positive and Gram-negative bacteria play a central role in how this happens.
Gram-positive pathogens often release powerful exotoxins—proteins secreted into the surrounding tissue that can damage cells, disrupt signaling, or paralyze the immune response. Streptococcus pyogenes, for instance, produces toxins that destroy red blood cells and connective tissue, leading to devastating infections like necrotizing fasciitis, sometimes called “flesh-eating disease.”
Gram-negative bacteria, in contrast, often rely on their outer membrane and LPS. When they die, they release endotoxins—lipid components of LPS—that can trigger massive immune reactions. In severe infections, this can lead to septic shock, a life-threatening condition where the body’s immune response spirals out of control.
Some Gram-negative bacteria also use sophisticated injection systems—like molecular syringes—to deliver toxins directly into host cells. These type III secretion systems are like biochemical weapons, capable of hijacking the cell’s internal machinery.
Antibiotic Warfare and the Challenge of Resistance
When antibiotics were first discovered, they were hailed as miracle drugs—magic bullets that could eliminate infections with precision and speed. But the structural divide between Gram-positive and Gram-negative bacteria has always shaped how effective these treatments can be.
Gram-positive bacteria, with their exposed peptidoglycan walls, are generally more vulnerable to antibiotics that target cell wall synthesis, like penicillin and vancomycin. These drugs disrupt the construction of peptidoglycan, causing the bacteria to burst under osmotic pressure. However, resistance has emerged even here—MRSA (methicillin-resistant Staphylococcus aureus) is a notorious example, evading entire classes of antibiotics.
Gram-negative bacteria present a deeper challenge. Their outer membrane blocks many antibiotics from even reaching the vulnerable inner layers. They also possess efflux pumps—molecular devices that actively expel antibiotics—and enzymes like beta-lactamases that break down drugs before they can work.
As resistance spreads, especially among Gram-negative pathogens like Klebsiella pneumoniae and Acinetobacter baumannii, medicine faces a mounting crisis. Multidrug-resistant strains now cause untreatable infections in hospitals worldwide. In the microbial war for survival, bacteria are winning some critical battles.
Immunity and Inflammation: The Body’s Reaction to Bacterial Invaders
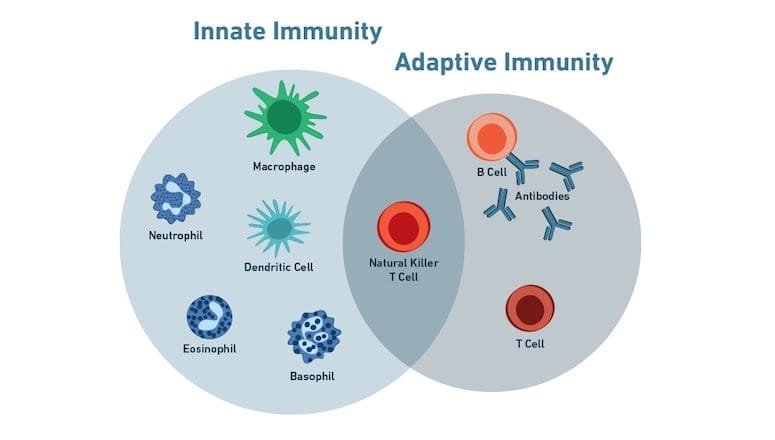
Our immune system evolved in a bacterial world. Every cell in our immune arsenal—from macrophages to neutrophils—recognizes and responds to bacterial patterns. The structural features that define Gram-positive and Gram-negative bacteria are also the very signals that alert the immune system to their presence.
Teichoic acids in Gram-positive bacteria and LPS in Gram-negative bacteria are recognized by toll-like receptors—molecular sentinels that trigger inflammation and immune activation. While this recognition is crucial for defense, it can also lead to collateral damage. In severe infections, the immune system’s reaction to LPS can cause systemic inflammation, organ failure, and death.
Vaccines, too, often target these unique structures. The pneumococcal vaccine, for example, uses polysaccharide components of the Gram-positive Streptococcus pneumoniae cell wall. The meningococcal vaccine targets proteins and sugars from the outer membrane of the Gram-negative Neisseria meningitidis.
Understanding these differences is not just academic—it saves lives. It shapes how we diagnose infections, choose antibiotics, and design vaccines.
The Gram Stain Today: A Vital First Step in Diagnosis
Over a century after Hans Christian Gram’s discovery, the Gram stain remains one of the most important tools in clinical microbiology. It is often the first test performed on a sample suspected of infection. In just minutes, a technician can determine whether bacteria are present, what shape they are, and whether they are Gram-positive or Gram-negative.
This information immediately guides treatment. If a spinal fluid sample from a patient with meningitis shows Gram-negative diplococci, doctors will suspect Neisseria meningitidis and act quickly. If a wound swab shows Gram-positive cocci in clusters, Staphylococcus aureus becomes a likely culprit.
In an era of genetic sequencing and molecular diagnostics, the Gram stain may seem quaint. But its speed, simplicity, and reliability keep it at the frontline of microbial diagnosis. It’s a reminder that sometimes, the most profound insights come from the simplest tools.
Evolutionary Echoes: A Tale of Two Lineages
The division between Gram-positive and Gram-negative bacteria is more than a staining artifact—it reflects deep evolutionary lineages. Gram-positive bacteria belong mostly to the phylum Firmicutes and Actinobacteria. Gram-negatives dominate phyla like Proteobacteria and Bacteroidetes.
These lineages diverged billions of years ago, shaped by planetary chemistry, ancient ecosystems, and the pressures of survival. The structural differences that Gram observed were forged in deep time, reflecting divergent paths toward the same goal: persistence.
Interestingly, not all bacteria fit neatly into this binary. Some, like Mycobacterium tuberculosis, have complex walls that resist Gram staining altogether. Others, like Mycoplasma, have no cell wall at all. The bacterial world is diverse and full of exceptions—but the Gram division remains a useful and powerful lens.
Gram Status and the Microbiome: Friends, Not Just Foes
Not all bacteria are enemies. In fact, most are benign or beneficial. In the human microbiome, both Gram-positive and Gram-negative bacteria coexist in complex communities that influence digestion, immunity, and even mood.
Gram-positive species like Lactobacillus and Bifidobacterium help ferment food and maintain gut health. Gram-negative species like Bacteroides break down complex carbohydrates and regulate immune tolerance. These bacteria are not passive residents—they interact with human cells constantly, sending signals, training immune responses, and influencing metabolism.
When this microbial harmony is disrupted—by antibiotics, poor diet, or illness—disease can follow. Understanding the Gram identity of these microbes helps researchers develop probiotics, design better diets, and treat inflammatory diseases.
A Future Built on Bacterial Wisdom
The story of Gram-positive and Gram-negative bacteria is not static. It continues to evolve with every discovery. Scientists are now developing new antibiotics that bypass traditional resistance, engineering bacteriophages that infect specific Gram types, and designing synthetic membranes to mimic bacterial defenses.
Microbiologists are also harnessing the power of these microbes for industry—using Gram-positive bacteria to produce enzymes and biofuels, or Gram-negative bacteria for bioremediation and synthetic biology.
Even in the search for life beyond Earth, we look for bacterial analogs. Could Martian soil contain something like a Gram-negative microbe, with a complex outer membrane? Might icy moons harbor cell walls built on alien chemistry?
These questions link back to Gram’s simple stain—a flash of color that turned an invisible world into a legible one.
Conclusion: More Than Just a Color
When Hans Christian Gram first observed the staining differences in bacteria, he probably did not imagine the profound implications of his work. Yet his stain illuminated more than cell walls—it revealed survival strategies, evolutionary histories, and mechanisms of disease. The terms “Gram-positive” and “Gram-negative” are not just laboratory labels; they are windows into the biology, ecology, and danger of the microbial world.
In this vast and often invisible universe, a touch of violet and pink still guides our understanding. It connects the early days of microbiology with modern medicine, uniting simplicity with sophistication. And as science advances, we continue to learn from this first great divide—between the bacteria that hold their color and those that let it go.