In the unseen universe of microscopic life, viruses have long been considered nature’s villains. They slip silently into cells, hijack their machinery, and replicate like saboteurs multiplying behind enemy lines. From influenza to HIV to SARS-CoV-2, viruses have been synonymous with disease, pain, and even death. Yet, paradoxically, some of these very organisms—once feared as agents of biological chaos—are being recast as powerful allies in modern medicine. These repurposed viruses are called viral vectors, and they are at the heart of two of the most revolutionary fields in medicine today: gene therapy and vaccines.
Viral vectors are not just scientific curiosities. They are living vehicles engineered to deliver hope—literally carrying life-saving genetic material into the cells of patients with devastating illnesses. They form the invisible engines behind therapies that have given sight to the blind, extended the lives of children with genetic disorders, and even brought the world a new kind of vaccine during a pandemic that touched every corner of the globe.
To understand what a viral vector is, and why it holds such transformative potential, we must explore its biological roots, its role in modern biotechnology, and its ethical and scientific implications for the future of health and humanity.
The Viral Code: Turning Enemies Into Allies
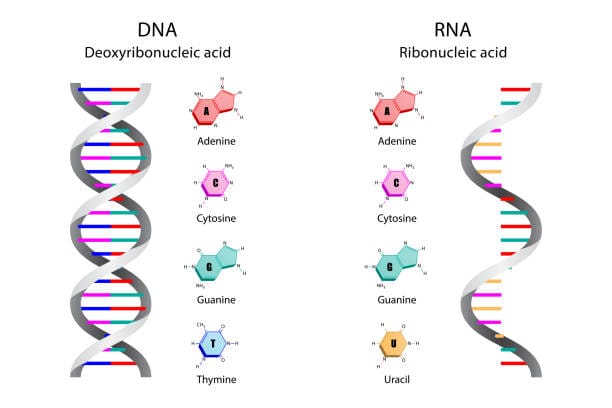
Viruses are, at their core, simple machines. They are made up of genetic material—either DNA or RNA—wrapped in a protein coat. Lacking the tools to reproduce on their own, they must enter a living host cell, inject their genetic instructions, and commandeer the host’s cellular machinery to replicate.
This “infect and replicate” strategy has evolved over millions of years to become astonishingly efficient. Different viruses target different tissues—some favor the lungs, others the liver, the blood, or even the brain. This tissue specificity, called “tropism,” is one of the reasons they make such effective delivery tools in biotechnology.
To create a viral vector, scientists strip the virus of its disease-causing genes, rendering it harmless. What remains is the virus’s natural ability to enter cells and deliver genetic material. In place of the original viral genes, researchers insert therapeutic DNA—genes that can correct a mutation, produce a missing protein, or train the immune system to recognize a threat. What was once a biological invader becomes a courier of healing.
A Brief History of Gene Transfer Dreams
The concept of using viruses as genetic delivery systems is not new. The roots of gene therapy trace back to the 1960s, when scientists first speculated that viral infection mechanisms could be harnessed to insert corrective genes into human cells. But the road from idea to reality was long and fraught with setbacks.
In the 1990s, early gene therapy trials raised hopes and alarms. The tragic death of 18-year-old Jesse Gelsinger in a 1999 gene therapy trial at the University of Pennsylvania marked a turning point. He had a rare liver disorder and was given an adenoviral vector—a modified common cold virus—to deliver a corrective gene. His immune system mounted a massive response to the virus, resulting in multi-organ failure and death.
Jesse’s story cast a long shadow over gene therapy research. For years, funding and public confidence declined. But rather than ending the field, his death led to rigorous safety reforms, stricter oversight, and deeper exploration into the behavior of viral vectors. Scientists went back to the drawing board—determined not only to honor his sacrifice but to build something safer and stronger.
Today, gene therapy is no longer an experimental gamble. It’s a clinically approved reality for conditions ranging from spinal muscular atrophy to inherited blindness, thanks to safer, smarter viral vectors.
The Art of Engineering a Viral Vector
Creating a viral vector is an exercise in precision engineering. Scientists choose a virus based on how efficiently it can infect target cells and how safe it is. The most commonly used viral families include adenoviruses, adeno-associated viruses (AAVs), lentiviruses (a type of retrovirus), and herpes simplex viruses.
Each type has distinct advantages. Adenoviruses can deliver large genes and produce strong short-term effects—ideal for vaccines. AAVs are less likely to provoke immune reactions and integrate rarely into the host genome, making them suitable for long-term gene therapies. Lentiviruses, on the other hand, can integrate into dividing cells and are often used in treatments for blood disorders or immunodeficiencies.
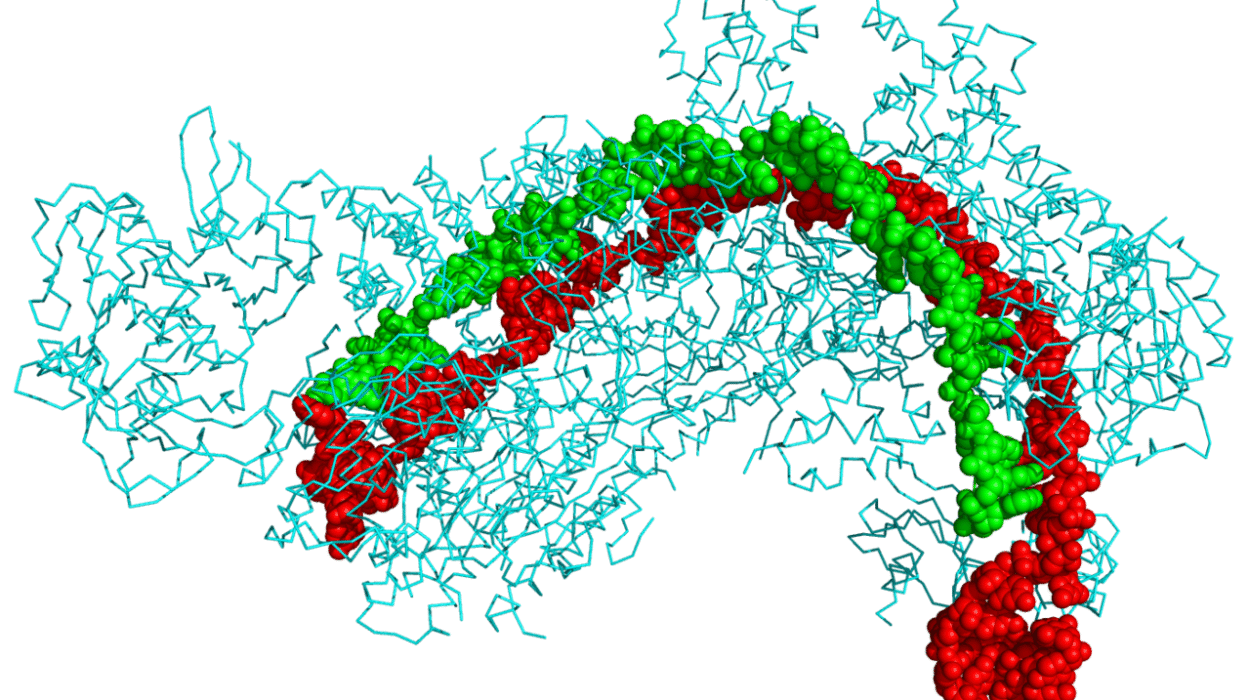
Once the virus is chosen, scientists delete the genes responsible for replication and pathogenicity. They then insert the therapeutic gene, often along with regulatory sequences that control how, when, and where the gene is expressed. The modified virus is then produced in specialized cell cultures, purified, and rigorously tested for safety and effectiveness before it ever reaches a patient.
The end result is a viral particle that can no longer cause disease—but can still do what viruses do best: deliver genetic material with surgical precision.
Viral Vectors in Gene Therapy: Curing the Incurable
One of the most breathtaking applications of viral vectors has been in gene therapy for rare genetic diseases—conditions once considered incurable, even untreatable.
Consider spinal muscular atrophy (SMA), a devastating neuromuscular disorder that strikes infants, causing progressive muscle wasting and early death. The root cause is a missing or defective SMN1 gene. In 2019, the FDA approved Zolgensma, a gene therapy using an AAV9 vector to deliver a functional copy of the gene. With a single intravenous infusion, the therapy enters the motor neurons, restores SMN1 function, and can dramatically alter the child’s prognosis.
Or take Leber’s congenital amaurosis (LCA), a form of inherited blindness. In 2017, Luxturna became the first FDA-approved gene therapy for a genetic disease affecting the eye. It uses an AAV vector to deliver a corrective gene directly into the retina, restoring light perception and, in many cases, functional vision.
There’s also beta-thalassemia, a blood disorder caused by mutations in the hemoglobin gene. Viral vectors—especially lentiviruses—can be used to insert functional hemoglobin genes into a patient’s own stem cells, which are then reinfused into the bloodstream. These modified cells go on to produce healthy red blood cells, reducing or even eliminating the need for transfusions.
These examples are not science fiction. They are living proof that viral vectors can do what was once unimaginable: not just treat symptoms, but correct the root cause of disease at the genetic level.
Viral Vectors and Cancer: Turning the Tables
Viral vectors are not limited to genetic disorders. They are also being used in the war against cancer. In this realm, viruses are engineered to carry genes that either stimulate the immune system or kill cancer cells directly.
Some therapies use viral vectors to reprogram immune cells. A striking example is CAR-T cell therapy, where a patient’s T cells are extracted, genetically modified using lentiviral vectors to express chimeric antigen receptors (CARs), and then returned to the body. These engineered cells are trained to recognize and destroy cancer cells—particularly in leukemia and lymphoma.
Other approaches involve oncolytic viruses—viruses designed to infect and kill cancer cells while sparing healthy ones. In 2015, the FDA approved T-VEC, an oncolytic herpes virus for advanced melanoma. It works by entering tumor cells, replicating until the cells burst, and releasing substances that alert the immune system to the presence of cancer.
In both cases, viral vectors play a crucial role in tilting the balance of power back in favor of the patient, using the very tools of biology that once threatened life to now preserve it.
The COVID-19 Vaccine Revolution
The COVID-19 pandemic, one of the most urgent global crises in modern history, gave viral vectors their most public and high-stakes debut. As the world scrambled for protection, multiple vaccine platforms were pursued—including traditional protein-based vaccines, mRNA vaccines, and viral vector vaccines.
The Oxford-AstraZeneca vaccine (ChAdOx1), the Johnson & Johnson vaccine, and Russia’s Sputnik V all use viral vectors—specifically adenoviruses—to deliver a gene encoding the spike protein of the SARS-CoV-2 virus. Once inside human cells, this gene instructs the cell to produce the spike protein, triggering an immune response without causing illness.
These vaccines offered several advantages: they were stable at standard refrigeration temperatures, relatively inexpensive to produce, and capable of inducing both antibody and T-cell responses. In a world racing against time and death, viral vectors helped immunize billions.
Despite concerns about rare side effects, including blood clots, the technology proved adaptable, scalable, and effective—cementing the place of viral vectors in global public health.
Challenges and Controversies
For all their promise, viral vectors come with complex challenges. The human immune system, evolved to detect and destroy viral invaders, doesn’t always cooperate with therapeutic intentions. If the immune system recognizes the viral vector as a threat, it can eliminate the therapy before it takes effect—or cause inflammation and side effects.
Another concern is insertional mutagenesis. Some viral vectors integrate their genetic material into the host genome. If this happens near a cancer-causing gene (oncogene), it could potentially trigger malignancy. This risk is carefully monitored, especially with integrating vectors like lentiviruses.
Manufacturing viral vectors is another hurdle. Producing them at the scale, purity, and consistency required for human therapies is expensive and technically demanding. And regulatory approval processes are rigorous, requiring years of testing, clinical trials, and long-term safety monitoring.
There are also ethical considerations. As gene therapy advances toward editing embryos or altering traits beyond disease correction, questions of consent, access, and societal impact loom large.
Viral vectors open a door—not just to healing, but to fundamental questions about who we are, what we can change, and what boundaries we are willing to cross.
The Road Ahead: Toward a Genetic Renaissance
Viral vectors are not the end of the story—they are the beginning. As science advances, hybrid approaches are emerging. Some therapies combine viral vectors with CRISPR gene editing, creating systems that not only deliver new genes but can precisely edit existing ones. Others explore non-viral vectors like nanoparticles, which could someday replace viruses entirely.
Yet for now, viruses remain our most effective genetic messengers. What evolution designed for parasitism, human ingenuity has turned into a symphony of healing.
The future holds breathtaking possibilities. Could we one day treat Alzheimer’s by delivering protective genes to the brain? Eradicate HIV by inserting immune-enhancing DNA into T cells? Cure sickle cell disease with a single injection? These are not idle dreams—they are active areas of research, built on the backbone of viral vector technology.
A Legacy of Transformation
The story of viral vectors is the story of scientific redemption. It’s the story of how the smallest, most dangerous forms of life became vehicles of hope. It’s about how human beings, faced with suffering and loss, turned to nature’s own machinery and reimagined it for healing.
From the death of Jesse Gelsinger to the smiles of children who now walk, see, or live because of a single gene, the journey of viral vectors has been marked by pain, perseverance, and profound triumph.
These microscopic messengers carry more than DNA. They carry the dreams of families, the aspirations of scientists, and the promise of a future where disease no longer dictates destiny.
And that, in the truest sense, is the power of life—not just to survive the virus, but to transform it.