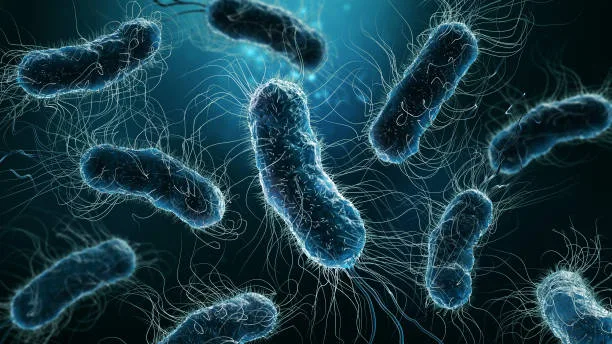
We often picture danger as something we can see—a wild animal, a speeding car, a looming storm. But some of the deadliest threats to human life are invisible to the naked eye. These threats don’t roar or flash. They whisper through the air, drift in water, and cling silently to our skin. They are bacteria—ancient, single-celled organisms that have shared our world for billions of years.
Most bacteria are harmless, and many are even vital to our survival. They help us digest food, produce vitamins, and protect us from more dangerous microbes. But some bacteria—the pathogenic kind—are agents of disease. They slip past our defenses, hijack our cells, and turn our own biology against us. These microbial invaders are responsible for some of the greatest health crises in human history. To understand how bacteria cause disease is to peer into a world of astonishing complexity, evolution, and silent warfare.
Ancient Origins, Endless Adaptations
Bacteria have been on Earth for over 3.5 billion years—long before animals, plants, or even complex cells evolved. They are masters of survival, capable of withstanding boiling heat, crushing pressure, and freezing cold. Their ability to adapt quickly through genetic mutation and horizontal gene transfer makes them formidable opponents.
This ancient legacy means bacteria are not just simple germs. They are living machines, constantly evolving, sharing genes, and experimenting with new ways to thrive. Pathogenic bacteria—the ones that cause disease—are not inherently evil. They’re just doing what all life does: trying to survive and reproduce. Unfortunately, in their quest for survival, they sometimes destroy the very organisms that host them.
Entry Points: How Bacteria Invade the Body
The first step in any bacterial infection is entry. The human body is designed like a fortress, with barriers to prevent intruders. Our skin, mucous membranes, stomach acid, and immune defenses stand guard. But bacteria have evolved many ways to breach these defenses.
They can enter through wounds, insect bites, contaminated food, or even the air we breathe. Some exploit vulnerabilities in our skin—like Staphylococcus aureus, which causes skin infections and boils. Others ride droplets from a cough or sneeze into our lungs, like Mycobacterium tuberculosis. Still others—like Salmonella or E. coli—hide in undercooked food, slipping past our stomach acid to colonize the intestines.
Some bacteria are opportunists. They’re part of our normal flora, living harmlessly in our mouths or on our skin. But when our immune system is weakened, or when they find themselves in the wrong part of the body, they become dangerous. A urinary tract infection, for example, often starts with bacteria from the intestines—harmless in one place, harmful in another.
The Weapons of Infection: Toxins, Adhesion, and Invasion
Once inside, pathogenic bacteria must secure their position. They need to anchor themselves to our cells, resist being washed away, and defend against our immune system. To do this, they use a wide range of tools.
Many bacteria produce adhesins—special molecules on their surfaces that stick to the host’s cells. These act like grappling hooks, allowing the bacteria to cling to tissues even when surrounded by bodily fluids. For instance, Neisseria gonorrhoeae, the bacteria that causes gonorrhea, uses hair-like projections called pili to attach to the walls of the urethra.
Next, they may produce toxins—powerful chemicals that damage host cells, disrupt signaling, or suppress the immune response. There are two main types of bacterial toxins: endotoxins and exotoxins.
Endotoxins are part of the bacterial cell wall, released when the bacterium dies. These toxins, especially from Gram-negative bacteria like E. coli or Salmonella, can cause widespread inflammation, fever, and even septic shock.
Exotoxins, on the other hand, are actively secreted by live bacteria. Some of the most notorious exotoxins come from Clostridium botulinum, which causes botulism, and Corynebacterium diphtheriae, the agent behind diphtheria. These toxins can paralyze muscles, destroy tissues, and interfere with vital cellular functions.
Other bacteria are invasive—they burrow into our cells and live inside them. Listeria monocytogenes, for example, can cross the blood-brain barrier and cause meningitis. Mycobacterium tuberculosis hides inside immune cells, using our own defenses as a shield.
Outmaneuvering the Immune System
A key part of being a successful pathogen is avoiding destruction by the host’s immune system. Bacteria have developed numerous strategies for immune evasion.
Some bacteria disguise themselves. They cover their surfaces with a capsule made of sugars that mimic the host’s own molecules, making them invisible to immune surveillance. Streptococcus pneumoniae, a major cause of pneumonia and meningitis, uses this tactic to great effect.
Others play dead—literally. Mycobacterium tuberculosis can enter a dormant state inside immune cells, forming granulomas where it lies in wait for years before reactivating.
Still others mutate quickly, changing their surface proteins so antibodies can’t recognize them. This is part of what makes Neisseria meningitidis so dangerous—it can evade immune memory and strike even those previously exposed.
Some bacteria even turn our immune system against us. They trigger inflammation that damages tissues, making it easier for them to spread. Or they produce enzymes that break down antibodies or complement proteins, neutralizing our defenses.
Hijacking the Host: Manipulating Cells from Within
Once inside the body, many pathogenic bacteria don’t just sit still—they take over host processes for their own benefit. This manipulation is astonishing in its precision.
Some bacteria inject proteins into host cells using a syringe-like apparatus called a type III secretion system. This molecular weapon, used by bacteria like Shigella, Yersinia, and Salmonella, allows them to reprogram host cells—causing them to engulf the bacterium, rearrange their cytoskeletons, or suppress immune signaling.
Chlamydia trachomatis, the bacterium responsible for the most common sexually transmitted infection worldwide, creates a special compartment called an inclusion inside host cells. It lives and reproduces there, shielded from immune attack.
Legionella pneumophila, which causes Legionnaires’ disease, hides inside lung macrophages by altering the internal membranes of the cell, turning the immune cell into a factory for bacterial growth.
These sophisticated mechanisms reveal just how much bacteria have learned, through evolution, about the inner workings of human cells. In many cases, they are better at manipulating us than we are at defending ourselves.
The Cascade of Disease: Symptoms, Damage, and Spread
As the bacteria thrive, the body suffers. The symptoms of bacterial disease are often not caused directly by the microbes, but by the immune system’s response. Fever, pain, swelling, and fatigue are all signs of the body fighting back.
In some cases, the damage is localized. A sore throat, a skin abscess, or a bladder infection may resolve with rest or antibiotics. But when bacteria enter the bloodstream or vital organs, the stakes rise dramatically.
Sepsis, for example, is a life-threatening condition where the immune system goes into overdrive, causing widespread inflammation, tissue damage, and organ failure. It can be triggered by bacteria in the lungs, abdomen, urinary tract, or even from an infected wound.
Meningitis, an infection of the membranes surrounding the brain and spinal cord, can cause permanent damage or death within hours if not treated. Neisseria meningitidis and Haemophilus influenzae are frequent culprits, especially in young children.
Pneumonia, a lung infection often caused by Streptococcus pneumoniae, Klebsiella pneumoniae, or Legionella, impairs oxygen exchange and can be fatal in the elderly or those with weakened immunity.
The bacteria don’t just kill by direct destruction—they overwhelm the host’s systems. In some diseases, like cholera or dysentery, massive fluid loss caused by bacterial toxins can lead to shock. In others, such as endocarditis, bacteria lodge in the heart’s valves, disrupting blood flow and spreading inflammation.
Transmission: From One Host to the Next
For a pathogen, disease is not the goal. Survival is. And to survive, bacteria must spread.
Transmission is the final stage of the bacterial life cycle within a host. Some bacteria, like Vibrio cholerae, trigger explosive diarrhea to exit the body and contaminate water sources. Others, like Bordetella pertussis (whooping cough), cause violent coughing that sprays bacteria into the air.
Sexually transmitted bacteria, such as Treponema pallidum (syphilis) or Neisseria gonorrhoeae, exploit intimate contact. Others, like Borrelia burgdorferi (Lyme disease), hitch rides on ticks. The modes of transmission are as varied as the bacteria themselves.
What’s remarkable is how transmission strategies shape disease symptoms. In respiratory infections, for instance, coughing is not just a symptom—it’s the bacterium’s exit strategy. In skin infections, oozing lesions serve the same purpose. Bacteria are not just fighting to survive; they are broadcasting themselves to the next host.
Antibiotics: A Double-Edged Sword
The 20th century brought a revolution in the battle against bacterial disease with the discovery of antibiotics. Penicillin, the first true antibiotic, saved millions of lives during World War II. Other drugs followed—streptomycin, tetracycline, erythromycin—and diseases once considered deadly became treatable.
Antibiotics work by targeting bacterial structures or functions not found in human cells. Some disrupt cell walls, others inhibit protein synthesis or DNA replication. The specificity and power of antibiotics made them medical miracles.
But the story didn’t end there. Bacteria adapted.
Through mutation and horizontal gene transfer, many bacteria developed resistance to antibiotics. Misuse and overuse of these drugs in medicine and agriculture accelerated the problem. Today, drug-resistant infections kill hundreds of thousands of people each year—a number projected to rise dramatically.
Methicillin-resistant Staphylococcus aureus (MRSA), multi-drug resistant tuberculosis, and carbapenem-resistant Enterobacteriaceae are just a few of the superbugs threatening a return to the pre-antibiotic era. The same evolutionary genius that made bacteria powerful pathogens now fuels their resistance.
Fighting Back: Vaccines, Hygiene, and Innovation
Despite the rising challenge of resistance, humanity is not defenseless. Many bacterial diseases are preventable with vaccines. Diphtheria, tetanus, pertussis, and meningococcal disease have all been dramatically reduced thanks to immunization programs.
Basic hygiene—clean water, handwashing, food safety—remains one of the most effective tools against bacterial spread. Sanitation systems have done more to prevent disease than any single drug.
New technologies offer hope. Phage therapy, which uses viruses that infect bacteria, is being revisited. CRISPR-based tools may allow us to selectively disable bacterial genes. And advances in microbiome science hint that supporting our beneficial bacteria might be a way to outcompete the harmful ones.
But the ultimate battle will not be won in laboratories alone. It will require global cooperation, responsible use of antibiotics, and a deeper understanding of the bacteria that share our world.
Living with Bacteria: The Path Forward
To study how bacteria cause disease is not just to explore the biology of infection. It is to confront a mirror of evolution itself. These microscopic invaders challenge our immune systems, our technologies, and our public health systems—but they also illuminate the complexity of life.
Most bacteria are not our enemies. The gut microbiome, in particular, is now recognized as essential for digestion, mood regulation, and immune function. We live in symbiosis with trillions of bacterial cells. We are not alone, even in our own bodies.
Understanding bacterial pathogenesis helps us draw a clearer line between friend and foe—but it also teaches us that this line is not always fixed. In one context, a bacterium is a lifesaving probiotic; in another, it’s a killer.
As we move into an age of precision medicine and synthetic biology, our relationship with bacteria is evolving. We may one day engineer microbes to heal us, clean our environments, or even prevent infections before they begin.
The story of bacteria and disease is far from over. It is an arms race, a dialogue, and a partnership—sometimes hostile, sometimes helpful, but always unfolding inside and around us.