When you walk into a doctor’s office with a cough, a strange pain, or a persistent symptom, you might not realize that behind every question your doctor asks, every test they order, and every treatment they prescribe is a time-tested process—one grounded in rigorous logic, cautious inquiry, and scientific skepticism.
This process is the scientific method, and it is the backbone of modern medicine.
But medicine isn’t just about science. It’s also deeply human. Doctors don’t treat diseases—they treat people. And people are complex, messy, emotional, and unique. That’s why the application of the scientific method in medicine is not purely mechanical or mathematical. It’s thoughtful. It’s interpretive. It requires critical judgment, ethical reflection, and empathy.
In this article, we’ll explore how the scientific method functions in medical practice—not just in research labs and clinical trials, but in the real-world decisions doctors make every day. We’ll look at how hypotheses are formed, how evidence is gathered, how uncertainty is managed, and how scientific thinking helps save lives. We’ll also explore where things can go wrong, and why evidence-based medicine is both essential and sometimes elusive.
This is the story of how doctors think—not as wizards or technicians, but as scientists in white coats, doing detective work with human lives on the line.
The Foundations: What Is the Scientific Method?
To understand how medicine works, we need to understand the scientific method itself.
At its core, the scientific method is a structured process for asking and answering questions about the natural world. It begins with observation, followed by the formation of a hypothesis—a testable explanation. Then comes experimentation or data collection, leading to analysis. Based on the results, the hypothesis is either supported, refuted, or refined. The process is repeated, often countless times, to arrive at robust conclusions.
Here’s a simplified version:
- Observe a phenomenon.
- Ask a question.
- Form a hypothesis.
- Test the hypothesis through experiment or data.
- Analyze results and draw conclusions.
- Communicate and replicate findings.
This method has powered centuries of progress—from the structure of DNA to the development of antibiotics to the mapping of the human genome. It is not a formula, but a mindset: skeptical, curious, and rigorous.
In medicine, the stakes are uniquely high. Doctors don’t have the luxury of perfect knowledge. They must often act under uncertainty, balancing risks and benefits. That’s where the scientific method becomes not just a guide—but a lifeline.
From Bedside to Bench: The Loop of Observation
Let’s begin at the bedside, where most medical journeys start.
A patient arrives with symptoms: chest pain, dizziness, a rash, a cough. These symptoms are observations, and they launch a chain of reasoning. The doctor asks questions, examines the body, and begins forming hypotheses about what might be wrong.
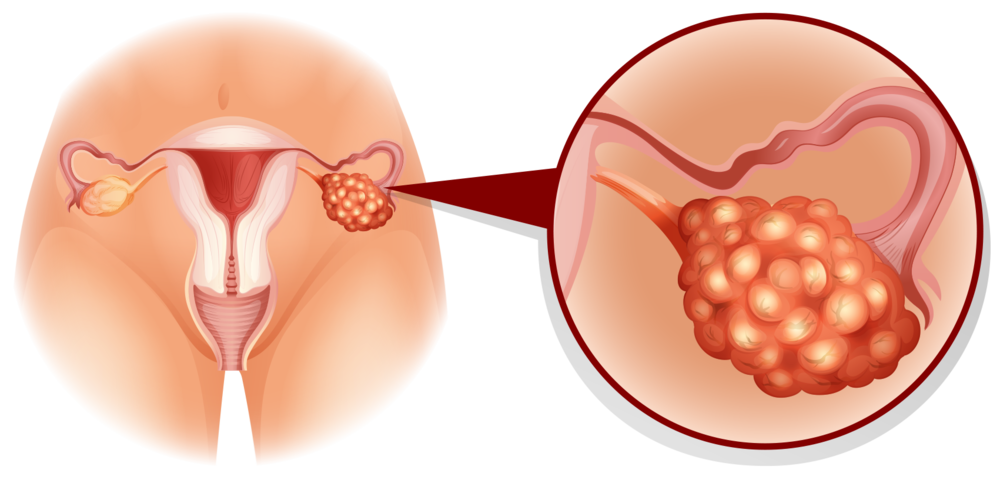
This is where medicine gets personal. The same symptom can mean different things in different people. A cough could be a cold, asthma, pneumonia, lung cancer, or acid reflux. Each possibility becomes a differential diagnosis—a list of hypotheses to be tested.
The doctor uses a mix of pattern recognition, clinical reasoning, and evidence-based knowledge to narrow down the list. Sometimes, the answer is obvious. Other times, it requires extensive investigation.
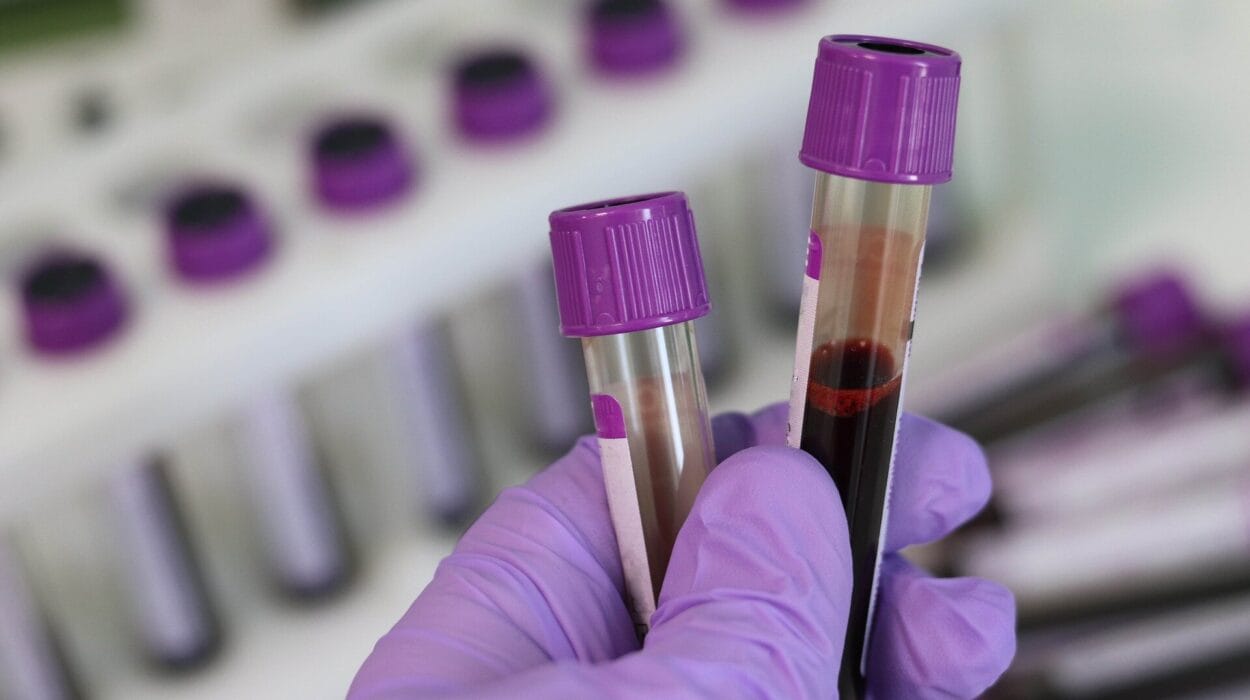
The patient’s history, physical exam, lab results, imaging studies, and response to treatments all provide data—the evidence upon which conclusions are built. Each test serves a purpose: to support or rule out a hypothesis.
This process is inherently scientific: observation → hypothesis → testing → conclusion. It doesn’t always follow a linear path. Medicine is iterative, and so is science.
Clinical Trials: The Engine of Medical Evidence
While the individual doctor uses the scientific method at the bedside, the broader field of medicine relies on a more formal process to generate medical knowledge: clinical research.
Clinical trials are the gold standard for testing new treatments, procedures, and interventions. They take a hypothesis—say, that Drug X lowers blood pressure better than Drug Y—and test it in controlled conditions.
A well-designed trial uses randomization, control groups, and blinding to eliminate bias. Participants are randomly assigned to receive either the treatment or a placebo (or comparison treatment), and neither the patients nor the researchers know who is getting what until the study ends.
Outcomes are measured using pre-defined endpoints—like blood pressure levels, survival rates, or symptom relief. The data is analyzed statistically to determine whether any differences are real or due to chance.
These trials don’t just inform doctors; they shape guidelines, change policies, and save lives.
But clinical trials also have limitations. They can be expensive, time-consuming, and sometimes ethically or logistically difficult. Not every patient fits the mold of a trial participant. Real-world medicine must interpret and apply research findings in nuanced, individual ways.
Evidence-Based Medicine: Bridging Research and Practice
Evidence-Based Medicine (EBM) is the philosophy that brings scientific research into clinical practice. It’s often defined as the integration of:
- The best available research evidence.
- The clinician’s expertise.
- The patient’s values and preferences.
This triad ensures that medical decisions are not based solely on gut instinct or tradition, but on carefully evaluated evidence—applied with wisdom and tailored to the person in front of the doctor.
For example, suppose a large clinical trial shows that Drug A reduces stroke risk in people with high blood pressure. That’s valuable evidence. But the doctor must still decide whether to prescribe it to this patient, who may be elderly, allergic to a component, or worried about side effects.
EBM encourages doctors to ask: What does the evidence say? How strong is it? How applicable is it to this case? What are the patient’s goals and fears? This process honors both science and the human experience.
Diagnostic Reasoning: Hypotheses at the Bedside
Let’s zoom in on one of the most crucial applications of the scientific method in medicine: diagnosis.
Diagnostic reasoning is how doctors figure out what’s wrong. It’s a mix of art and science, intuition and analysis. And at its core is the generation and testing of hypotheses.
Here’s how it works:
A patient presents with symptoms. The doctor forms an initial hypothesis—perhaps based on pattern recognition or experience. Then they test that hypothesis through history-taking, physical examination, and diagnostic testing.
Each result helps refine the hypothesis. A negative test might rule out one disease; a positive test might increase the probability of another. Doctors use Bayesian reasoning—updating probabilities as new data comes in.
This process is dynamic and ongoing. Doctors think in terms of pre-test and post-test probability—how likely a diagnosis is before and after each new piece of information.
Importantly, doctors must guard against cognitive biases—like anchoring (clinging to an initial diagnosis), confirmation bias (favoring evidence that supports a belief), or premature closure (stopping the reasoning process too early).
Good diagnostic reasoning is not just about having knowledge—it’s about thinking clearly, checking assumptions, and remaining open to new possibilities.
Treatment Decisions: Weighing Evidence and Risk
Once a diagnosis is made, the next question is: What do we do about it?
Treatment decisions are where the scientific method meets real-world complexity. Doctors must weigh benefits and risks, apply evidence to the individual, and anticipate side effects or complications.
Let’s say a patient has high cholesterol. There are medications—statins—that can lower cholesterol and reduce the risk of heart attacks. The evidence is strong. But not everyone needs treatment.
The doctor must ask:
- How high is the cholesterol?
- Does the patient have other risk factors?
- What does the patient value more—reducing risk or avoiding medication?
- Are there lifestyle changes that could help?
This is shared decision-making—a process where doctor and patient work together, informed by science, to choose the best course of action.
Sometimes the decision is urgent—like giving antibiotics for meningitis. Other times, it’s more ambiguous—like choosing whether to undergo elective surgery. The scientific method provides a framework, but human judgment remains essential.
Monitoring and Follow-Up: The Cycle Continues
Medicine doesn’t stop at diagnosis and treatment. Every intervention must be monitored—for effectiveness, side effects, and unintended consequences.
If a treatment works, the hypothesis is strengthened. If it fails, the doctor must reconsider the diagnosis, adjust the treatment, or explore other causes. This is feedback—another key part of the scientific method.
Follow-up allows doctors to track outcomes over time, learn from experience, and improve future decisions. In chronic diseases—like diabetes or heart failure—this process is ongoing and dynamic.
Each visit is another opportunity for observation, hypothesis, testing, and refinement. Medicine is not a one-time event; it’s a continuous experiment in healing.
Mistakes and Uncertainty: When the Method Fails
Despite all its strengths, the scientific method is not infallible. In medicine, things go wrong.
Sometimes the evidence is flawed—due to poor study design, publication bias, or conflicts of interest. Sometimes doctors misinterpret data, fall prey to bias, or lack critical thinking. Sometimes the patient’s condition is truly mysterious—defying all known categories.
Errors in diagnosis, treatment, or communication can harm patients. That’s why critical appraisal, peer review, and quality improvement are essential parts of scientific medicine.
Uncertainty is a constant companion in clinical practice. No test is perfect, no treatment guaranteed. The scientific method helps manage that uncertainty—not eliminate it.
Doctors must learn to say, “I don’t know—but here’s what we’ll do next.”
The Role of Technology: A New Scientific Partner
In recent years, technology has transformed the practice of medicine. Electronic health records, artificial intelligence, genomics, and big data are revolutionizing how doctors gather and analyze information.
AI systems can now interpret X-rays, predict outcomes, and suggest diagnoses. Algorithms based on massive datasets can detect patterns invisible to the human eye.
But these tools are only as good as the science behind them. They must be validated, tested, and continually refined. And they must be used ethically and thoughtfully.
The doctor of the future will be part scientist, part data analyst, and part philosopher—balancing technology with human understanding.
Case Study: The Scientific Method in Action
Let’s walk through a real-world example.
A 52-year-old man comes to the emergency room with chest pain. He’s sweating, anxious, and says the pain started suddenly while mowing the lawn.
Observation: Chest pain, sweating, anxiety, sudden onset.
Hypothesis: Possible heart attack (myocardial infarction), but also consider other causes—muscle strain, indigestion, pulmonary embolism, aortic dissection.
Testing: An EKG, blood tests (troponin), chest X-ray, and physical exam are ordered.
Results: EKG shows ST elevation. Troponin is elevated. Diagnosis: ST-elevation myocardial infarction (STEMI).
Treatment decision: Based on evidence, the patient is given aspirin, nitroglycerin, and rushed to the catheterization lab for emergency angioplasty.
Outcome: A blocked coronary artery is opened. The patient stabilizes.
Follow-up: The patient is started on medications for heart health, enrolled in a cardiac rehab program, and counseled on lifestyle changes.
Every step in this case—observation, hypothesis, testing, action—follows the scientific method. And every step could have gone differently if the data had changed. That is the power—and the precision—of scientific medicine.
Conclusion: The Mind of a Doctor, The Method of Science
Medicine is a field where human lives meet scientific logic. It demands both rigor and empathy, both analysis and intuition.
The scientific method gives doctors a roadmap through the fog of illness. It helps them ask better questions, make better decisions, and learn from every patient they treat. It turns mystery into manageable uncertainty, and chaos into care.
But science alone is not enough. Medicine also requires humility, compassion, and a willingness to admit when we don’t have all the answers.
In the end, the best doctors are not just practitioners of science—they are scientists themselves. Each patient is a hypothesis, each illness a puzzle, each recovery a piece of evidence that pushes the field forward.
And that’s how doctors make decisions: not with magic, but with method.