Every breakthrough medication, life-saving vaccine, or advanced therapy used in modern medicine has passed through a rigorous and often invisible process known as the clinical trial. To the average person, the term may conjure images of white-coated scientists, patient volunteers, and rows of pills in sterile bottles. But behind those glimpses lies a complex, years-long journey filled with discovery, failure, ethics, hope, and science.
Clinical trials are structured studies designed to evaluate the safety, efficacy, and long-term impact of new medical interventions in humans. They are the bridge between the lab bench and the hospital bedside, where theoretical science is tested in the real world. Without clinical trials, we would never know whether a new drug actually works, whether it causes harm, or how it performs compared to existing treatments.
But these trials are not mere experiments—they are deeply human endeavors. They involve real people with real diseases, doctors who make hard decisions, regulators who enforce strict standards, and scientists whose passion drives the future of medicine. To understand how clinical trials work is to understand how modern medicine advances—not through miracle, but method.
From Discovery to Design: The Preclinical Phase
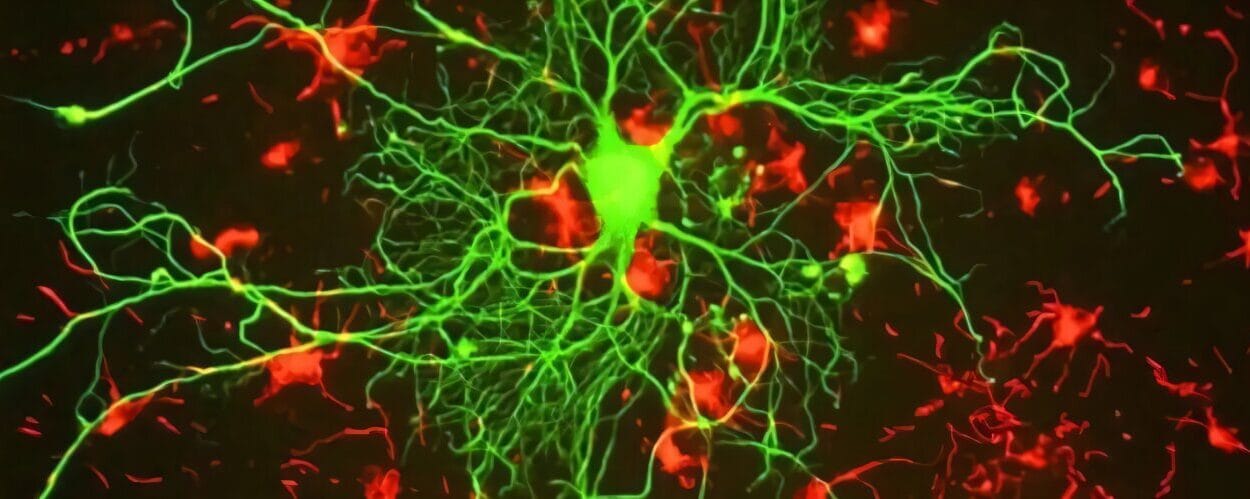
Before a drug ever reaches a human being, it starts in the lab. This preclinical phase is where molecules are mixed, diseases are modeled, and theories are tested on computer simulations or in petri dishes. If early results seem promising, scientists begin testing the potential treatment on animals. This isn’t done lightly. Animal testing is regulated and required, serving one critical purpose: to predict how the treatment might behave in the complex systems of a living organism.
These studies examine a drug’s pharmacokinetics (how it’s absorbed, distributed, metabolized, and excreted) and its pharmacodynamics (how it affects the body). Toxicity levels are gauged, optimal dosages calculated, and biological targets identified.
Only after a treatment proves relatively safe and effective in the preclinical phase can it be considered for human trials. But making that leap is like entering an entirely different universe—one governed not only by biology but by ethics, law, and real-world uncertainty.
Enter the Humans: Phases of Clinical Trials
Once a treatment is approved for testing in humans, clinical trials begin. These are broken into distinct stages, each with its own goals, methods, and scale. Known collectively as Phases I through IV, these steps ensure that new therapies are safe, effective, and ultimately valuable to the public.
Phase I: Is It Safe?
This phase is the first test in human beings, usually involving 20 to 100 healthy volunteers or patients. The primary objective is safety—what does the drug do in the body, and how much can be given without causing harm?
Phase I trials are often “dose-escalation” studies, where participants are given gradually increasing doses to identify side effects and determine the maximum tolerable dose. Researchers monitor everything: vital signs, lab tests, adverse reactions, even psychological changes.
Interestingly, Phase I trials often take place in highly controlled environments, sometimes even with participants living on-site for observation. These trials rarely test for therapeutic effects—though occasionally, signs of efficacy emerge, adding excitement to the findings.
Phase II: Does It Work?
If Phase I shows the drug is reasonably safe, it moves to Phase II. This phase includes a few hundred participants, typically people who actually have the condition the drug is intended to treat.
Now the question becomes: does the drug work as intended?
These trials compare the new treatment against a placebo or standard treatment. They are often “double-blinded,” meaning neither the patient nor the doctor knows who is receiving which treatment—ensuring objectivity.
Phase II identifies the optimal dose and further evaluates safety, but it’s also the first moment where researchers look for real evidence of efficacy. Did tumors shrink? Did symptoms improve? Did the disease progression slow?
At this stage, many drugs still fail. A promising treatment in animals or small samples might disappoint when tested more broadly in humans. But if the data looks good, the drug can graduate to the next level.
Phase III: How Well Does It Work?
Phase III is the real proving ground. Involving thousands or even tens of thousands of participants across multiple locations, this phase aims to confirm effectiveness, monitor side effects, and compare the new treatment against standard options.
These trials often span years and cost millions—or even billions—of dollars. They are multinational, highly regulated, and statistically complex. Phase III data is what ultimately determines whether a drug receives approval from regulatory bodies like the FDA (U.S.), EMA (Europe), or similar institutions in other countries.
Success in Phase III is far from guaranteed. Many treatments show marginal benefits or unforeseen risks when tested at scale. But if a treatment proves both safe and effective in Phase III, it has a high chance of being approved for public use.
Phase IV: What Happens in the Real World?
Approval isn’t the end—it’s just the beginning of a new chapter.
Phase IV, often called post-marketing surveillance, occurs after a drug has hit the market. These trials continue to monitor long-term safety, effectiveness in broader populations, rare side effects, and how the drug is used in real-world settings.
Sometimes, Phase IV trials uncover serious issues that weren’t visible in earlier phases—leading to dosage changes, new warnings, or even withdrawal from the market. But they also provide valuable insights into how a treatment performs outside the laboratory bubble.
Who Participates—and Why?
Clinical trials rely on volunteers. Without human participants, no new treatment could ever be tested. But why do people choose to enroll?
Motivations vary. Some seek access to cutting-edge therapies not available elsewhere, especially when battling life-threatening diseases. Others want to contribute to science or help future patients. In some trials—especially early phase studies—participants may receive compensation.
Every participant must provide informed consent, a formal process ensuring they understand the risks, benefits, and nature of the study. This consent is not a one-time signature—it’s an ongoing conversation, and participants can withdraw at any time.
Ethical considerations are paramount. Trials are reviewed by Institutional Review Boards (IRBs) or Ethics Committees, which ensure that patient rights are protected and that risks are minimized.
Historically, there have been serious abuses in medical research—the Tuskegee Syphilis Study, for instance—making ethical oversight absolutely vital. Today’s standards reflect lessons hard-learned, placing human dignity at the center of medical progress.
The Power of Placebos and Controls
To evaluate whether a treatment truly works, researchers must isolate its effects from other variables. That’s where placebos and control groups come in.
A placebo is an inactive substance designed to look and feel like the real treatment but has no therapeutic effect. Participants receiving a placebo serve as a baseline for comparison.
Control groups—whether they receive placebos or standard treatments—allow researchers to determine whether the new intervention performs better, worse, or the same.
These trials are often double-blind or even triple-blind, meaning neither the participant, the doctor, nor the data analysts know who received which treatment. This eliminates bias and ensures that expectations don’t skew results.
Some people are uncomfortable with the idea of placebos, especially in serious illnesses. That’s why ethical trial design often uses “active comparators” instead of placebos—comparing new treatments to the best existing therapies.
Statistical Strength: The Language of Proof
Behind every clinical trial lies a world of mathematics. Statistics determine how many participants are needed, how results are interpreted, and whether findings are “significant.”
A result is considered statistically significant when it’s unlikely to have occurred by chance. This is often indicated by a p-value—a measure of the probability that the observed effect could occur under the null hypothesis.
Statistical power, confidence intervals, standard deviations—these aren’t just technical jargon. They’re the tools scientists use to ensure that their conclusions are valid, reproducible, and trustworthy.
But statistics also come with limitations. A trial might show a statistically significant effect that isn’t clinically meaningful—or vice versa. That’s why interpretation, context, and peer review are crucial.
Trial Failures: Lessons in Disguise
Not all clinical trials end in success. In fact, most drug candidates fail at some point during the process. Sometimes the treatment doesn’t work. Sometimes it works, but with unacceptable side effects. Sometimes the results are inconclusive.
While disappointing, these failures are not wasted. Every failed trial contributes to our understanding of biology, disease mechanisms, and methodology. They refine hypotheses, inspire new directions, and prevent harm.
Pharmaceutical companies invest billions in R&D knowing that many candidates won’t make it to market. But they also know that each failure brings them closer to a success that could change millions of lives.
Breakthroughs and Blockbusters: When Trials Change the World
Despite the long odds, clinical trials do produce triumphs—treatments that revolutionize medicine, extend life, or even cure disease.
Consider the development of penicillin, which underwent early testing in humans during World War II and became the first widely used antibiotic.
Or the polio vaccine, tested in a massive Phase III trial involving over a million children—ushering in an era where polio became virtually eradicated in many parts of the world.
More recently, the rapid development and testing of COVID-19 vaccines demonstrated the power of coordinated, global clinical research. Though developed quickly, these vaccines passed through rigorous trials in tens of thousands of people before being approved.
Each success story represents thousands of hours of research, thousands of volunteers, and often years of effort.
Modern Challenges: Diversity, AI, and Global Trials
Today’s clinical trial landscape is evolving rapidly.
One major focus is diversity. Historically, clinical trials have disproportionately involved white male participants, leaving gaps in understanding how treatments affect women, minorities, and other demographics. Efforts are now underway to ensure broader representation and equitable access.
Another shift is decentralization. With wearable devices, telemedicine, and remote monitoring, participants can now join trials from their homes—reducing geographic barriers and increasing participation.
Artificial intelligence is also being used to design smarter trials, identify patient populations, and even predict outcomes. While still in early stages, AI has the potential to make trials faster, cheaper, and more personalized.
International collaboration is now the norm, with trials conducted across continents. But this introduces new complexities: differing regulations, cultural considerations, and ethical frameworks that must be harmonized.
The Human Side: Stories from the Front Line
Behind every clinical trial is a tapestry of human stories.
A mother with terminal cancer joining a trial as her last hope—and gaining precious extra months with her children.
A college student signing up for a Phase I vaccine trial to help during a pandemic.
A doctor who believes in a new treatment and spends years rallying support, funding, and patients to bring it to life.
These stories remind us that clinical trials aren’t just scientific. They’re emotional. They’re brave. They’re profoundly human.
Conclusion: From Lab to Life
Clinical trials are one of the greatest achievements of modern medicine. They represent a methodical, ethical, and evidence-based path from laboratory discovery to life-saving treatment.
They require rigor, patience, creativity, and most importantly—people. Patients, researchers, regulators, and volunteers all play a role in moving medicine forward.
In a world facing new diseases, aging populations, and global health crises, the importance of clinical trials has never been greater.
They are not perfect. They are not easy. But they are the reason we have vaccines, cancer therapies, heart drugs, mental health treatments, and surgical innovations.
They are the reason that tomorrow’s medicine will be better than today’s.
And perhaps most inspiring of all—they are still just beginning.