In today’s world, medicine has become far more than a list of ancient remedies or a collection of expert opinions. It is now a field guided by structured thinking, scientific proof, and a methodical approach to choosing the best treatments for patients. This guiding light is what we call Evidence-Based Medicine (EBM).
The term might sound complex or clinical, but at its core, evidence-based medicine is about making the best possible decisions in patient care using the best available evidence. It’s about ensuring that doctors, nurses, and other healthcare professionals don’t just follow tradition or intuition, but rely on actual scientific studies and well-tested data to guide their actions.
But what does that really mean? How does EBM work in real hospitals or clinics? And why should patients care?
This article will take you on a comprehensive, engaging journey to explore evidence-based medicine from the ground up. No jargon, no textbook mumbo-jumbo—just clear, thoughtful explanations designed for anyone who wants to understand how modern medicine works behind the scenes.
The Evolution of Medicine: From Guesswork to Evidence
To appreciate what evidence-based medicine is, it helps to understand what came before it. For much of human history, medicine was a mix of tradition, observation, and intuition.
If you had a fever in ancient Greece, your doctor might have said your “humors” were out of balance. In medieval Europe, leeches were popular for everything from headaches to infections. Even into the early 20th century, treatments were often based on what doctors had learned from mentors or observed from experience—not from scientific trials.
While experience and observation do hold value, relying solely on them often led to ineffective or even harmful treatments. What changed the game was the rise of scientific thinking, particularly in the late 19th and 20th centuries.
With the development of randomized controlled trials (RCTs), epidemiology, and statistical analysis, medicine began to shift. Now, treatments could be tested in structured ways to determine whether they actually worked—and how well they worked compared to alternatives.
This shift laid the groundwork for evidence-based medicine.
The Definition of Evidence-Based Medicine
Let’s now answer the central question: What is evidence-based medicine?
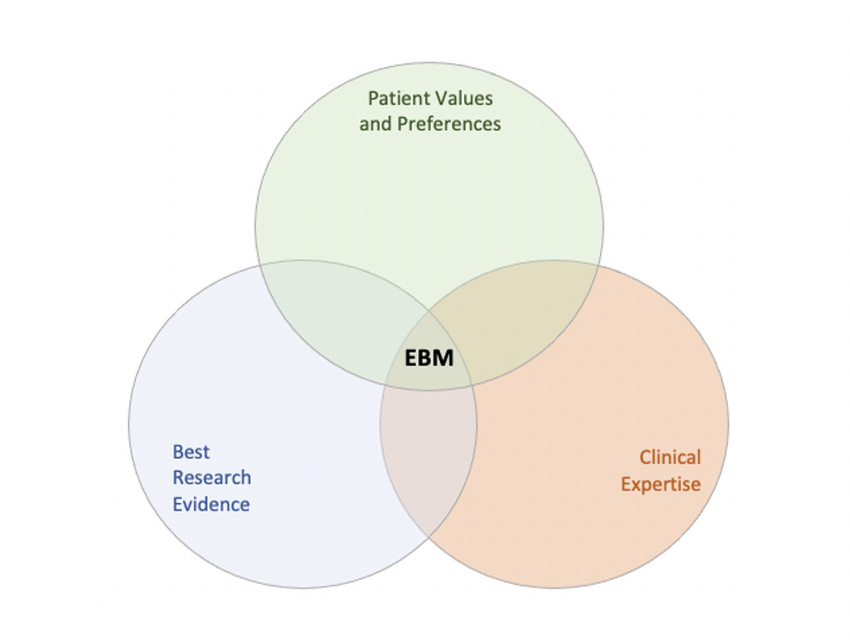
Evidence-based medicine is the careful and thoughtful use of current best evidence in making decisions about the care of individual patients. It blends three essential components:
- Best Available Evidence – This comes from high-quality research studies such as randomized controlled trials, cohort studies, and systematic reviews. It represents the most up-to-date and scientifically valid information available about a treatment or intervention.
- Clinical Expertise – This refers to the healthcare provider’s own skills, experience, and ability to interpret the evidence in the context of a particular patient.
- Patient Values and Preferences – Each patient is unique. Their goals, concerns, culture, and preferences must be considered when deciding on a treatment plan.
In short, evidence-based medicine is not just about cold, hard data. It’s about integrating data, doctor, and patient into one unified decision-making process.
The Evidence Pyramid: Not All Evidence Is Created Equal
One of the most helpful tools in understanding EBM is the evidence pyramid. Imagine a triangle divided into levels, with the most reliable forms of evidence at the top and the less reliable ones at the bottom.
At the base, you have things like case reports (stories of individual patients) and expert opinions. These can offer insights, but they don’t carry much weight when deciding whether a treatment works. That’s because they aren’t tested under controlled, scientific conditions.
As you move up the pyramid, you encounter case-control studies, cohort studies, and randomized controlled trials (RCTs). These involve comparing groups of patients and tracking outcomes over time. They use large sample sizes and careful statistical methods to reduce bias and increase reliability.
At the very top of the pyramid are systematic reviews and meta-analyses. These are studies that analyze multiple other studies. They look at all the available research on a topic, combine the findings, and draw broader conclusions. This is often considered the “gold standard” of evidence.
So, when doctors say they are using “evidence,” they ideally mean evidence from the top of this pyramid—not from hearsay or tradition.
How Evidence-Based Medicine Works in Real Life
Let’s walk through an example to show how evidence-based medicine functions in practice.
Imagine a doctor is treating a patient with high blood pressure. The traditional treatment has been Drug A, but a new medication, Drug B, has recently become available. The patient asks which is better.
The doctor will begin by consulting the best available evidence. That might mean looking at recent randomized trials comparing Drug A and Drug B, or a meta-analysis summarizing those studies. Let’s say the evidence shows that Drug B is more effective and has fewer side effects in most patients.
Next, the doctor will apply their clinical expertise. Perhaps they’ve treated dozens of patients with similar profiles and have noticed that Drug B sometimes causes dizziness in elderly patients. This experience is valid and must be considered.
Finally, the doctor talks with the patient. The patient says they’re very sensitive to side effects and want to avoid dizziness at all costs, even if that means slightly higher blood pressure. They also prefer to avoid new drugs until they’ve been on the market longer.
Now the doctor has all three pieces:
- The evidence says Drug B is better.
- Their experience suggests Drug B may not be ideal for this particular patient.
- The patient’s preference leans toward Drug A.
Based on all this, they may jointly decide to stick with Drug A, or perhaps use a lower dose of Drug B under close monitoring.
That’s evidence-based medicine in action: not blind obedience to data, but thoughtful integration of all factors to do what’s best for this patient, right now.
The Five Steps of Evidence-Based Practice
To apply evidence-based medicine consistently, healthcare professionals typically follow a five-step process known as the EBM cycle:
- Ask – Formulate a clear, answerable clinical question.
- Acquire – Search for the best available evidence.
- Appraise – Evaluate the quality, validity, and relevance of the evidence.
- Apply – Combine the evidence with clinical expertise and patient values.
- Assess – Reflect on the outcome and seek ways to improve.
These steps are simple in theory but require training, discipline, and often collaboration to carry out effectively.
Why Evidence-Based Medicine Matters to Patients
You don’t need to be a doctor to benefit from understanding EBM. As a patient, it directly affects the quality of care you receive.
Imagine two hospitals. In one, doctors follow the latest research and adjust their practices based on new findings. In the other, they rely on outdated routines and anecdotal experiences. Where would you rather be treated?
Evidence-based medicine promotes safer, more effective care. It helps reduce unnecessary procedures, minimize side effects, and improve outcomes. It ensures that treatments are not just “what we’ve always done,” but “what we know works.”
EBM also empowers patients. When you ask your doctor, “Why are you recommending this treatment?” an EBM-trained physician can give you a clear, reasoned answer based on science—not guesswork.
Challenges and Criticisms of EBM
While evidence-based medicine is a powerful approach, it’s not perfect. Like all systems, it has limitations.
One major challenge is information overload. There are thousands of new medical studies published every year. No individual doctor can read them all, let alone assess their quality and relevance. This is where tools like clinical guidelines and decision support systems help by summarizing evidence for busy professionals.
Another issue is study quality. Not all research is created equal. Some studies have flawed methods, small sample sizes, or hidden biases (often due to pharmaceutical funding). Doctors must learn to critically appraise evidence, not just accept it blindly.
There’s also the concern of individual variability. What works in a study may not work for every patient. Clinical trials often use average results from large groups, but real patients are individuals with unique genetics, lifestyles, and co-existing conditions.
Furthermore, accessibility and equity can complicate matters. In some countries or regions, the best evidence-based treatments may not be available or affordable, making it difficult to apply EBM fully.
Despite these hurdles, the philosophy of EBM remains sound: make decisions based on the best evidence available, while considering the needs of the patient.
EBM in the Digital Age
Technology is revolutionizing how evidence-based medicine is practiced. Digital platforms, apps, and online databases like PubMed, Cochrane Library, and UpToDate allow doctors to access research at the bedside. AI tools can now scan thousands of studies in seconds to recommend treatment options.
Electronic health records (EHRs) are also being designed to include clinical decision support systems (CDSS), which flag outdated prescriptions or suggest more effective alternatives based on recent research.
Even telemedicine and remote monitoring tools can now be evaluated through EBM methods, ensuring that new technologies are truly beneficial before being adopted widely.
As healthcare becomes more data-driven, the need for strong evidence-based frameworks will only grow.
Teaching and Learning EBM
Evidence-based medicine is now a core part of medical education worldwide. Students are taught how to read studies, critique them, and apply findings in clinical settings.
The teaching methods are hands-on and practical. Rather than just memorize facts, students learn to formulate clinical questions, search for evidence, and apply it to patient cases. This makes them better, more thoughtful clinicians in the long run.
Importantly, EBM also promotes lifelong learning. Medicine evolves constantly. New diseases appear. New drugs are developed. Guidelines change. An EBM-trained doctor never stops learning and adjusting their approach to reflect the most current knowledge.
The Human Side of Evidence
While EBM is rooted in science, it never forgets that patients are people—not statistics.
A key tenet of EBM is respect for patient values. No amount of data can dictate what a patient wants for their own body or life. Some might choose aggressive treatment; others may prioritize quality of life over longevity. Evidence-based medicine supports these choices by providing clear, honest information to guide them.
Doctors are not robots following formulas. They are compassionate professionals who use evidence as a tool, not a cage. At its best, EBM is about shared decision-making—where doctor and patient sit together, review the facts, and choose the path forward as a team.
Conclusion: A Better Way to Practice Medicine
Evidence-based medicine is more than a medical trend. It is a movement—a quiet revolution in how healthcare is delivered. It replaces tradition with testing, opinion with proof, and guesswork with guidance.
It doesn’t claim to have all the answers. But it offers a better way to find them.
By combining the best available research, the wisdom of experienced practitioners, and the values of each unique patient, EBM creates a form of medicine that is smarter, safer, and more humane.
It reminds us that the goal of medicine isn’t just to treat disease—it’s to care for people, one thoughtful decision at a time.