You check your calendar. Count the days. Then count them again. You’re late. No period. No cramps. Nothing. And unless you’re pregnant—because that’s the first place your mind probably went—you’re left wondering, what gives?
A missed period can feel like your body is playing tricks on you. But sometimes, the culprit isn’t hidden in a pregnancy test or a gynecologist’s diagnosis. Sometimes, the answer is hiding in plain sight—in your mind, in your to-do list, in your calendar that’s packed to the minute. The answer might be stress.
Stress is one of those sneaky culprits that can wreak havoc on your health without making a grand entrance. It doesn’t knock on the door and announce, “Hey, I’m about to hijack your hormones!” Instead, it creeps in, sometimes slowly, sometimes like a tidal wave, and before you know it, your period has vanished like a ghost.
Understanding the Menstrual Cycle
To fully appreciate how stress affects your menstrual cycle, it helps to understand what’s actually going on when your body orchestrates this monthly performance. Your period is not just a bleeding episode. It’s a hormonal symphony, a cascade of signals between your brain, ovaries, and uterus.
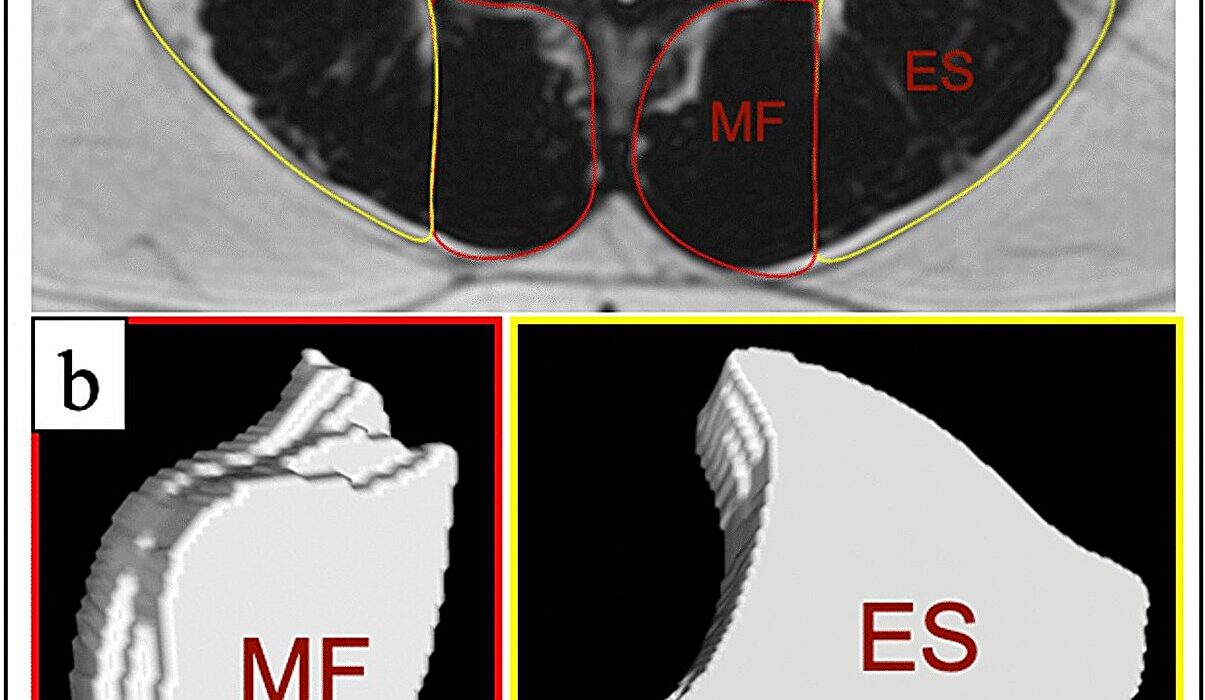
Each cycle starts in the brain—specifically in the hypothalamus, which sends a signal to the pituitary gland. The pituitary responds by releasing hormones—follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones travel to the ovaries, prompting them to mature an egg and prepare for ovulation. In turn, the ovaries produce estrogen and progesterone, hormones that prepare the uterine lining for a possible pregnancy. If no pregnancy occurs, those hormone levels drop, triggering menstruation.
This entire cycle is delicate. It depends on precise timing, hormonal balance, and an unobstructed line of communication between your brain and reproductive organs. When stress enters the scene, it can throw off this timing, interrupt these signals, and disrupt the balance.
What Stress Actually Does to Your Hormones
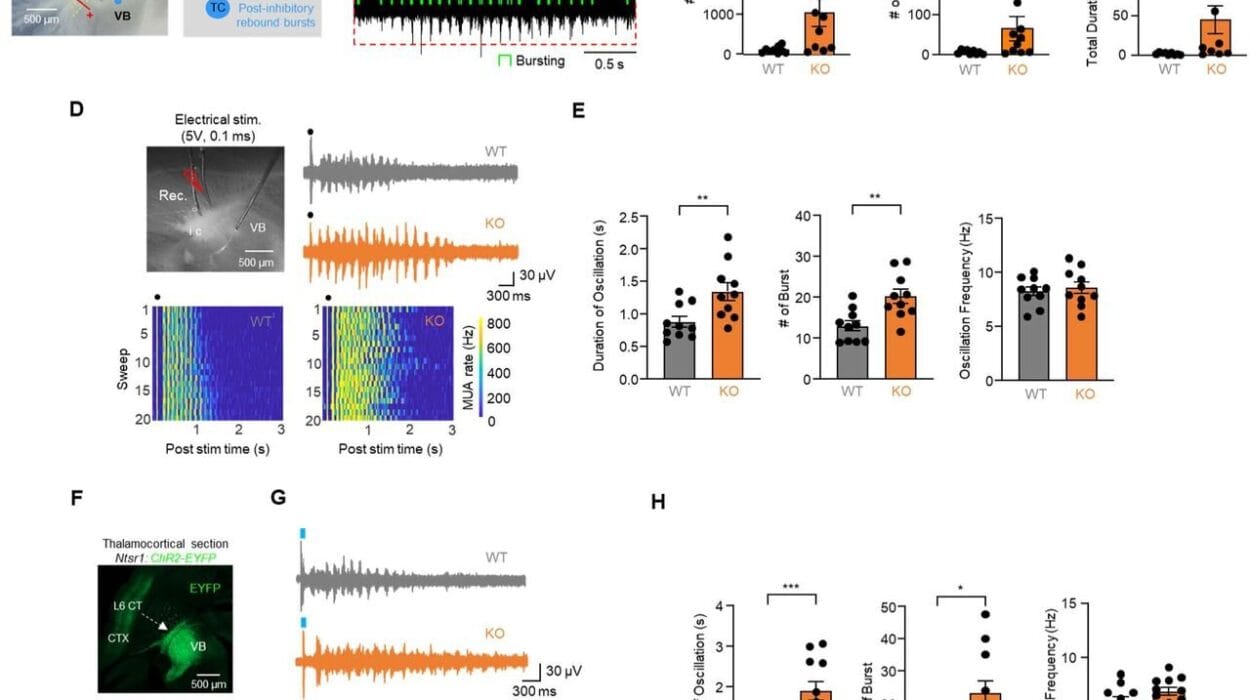
When your body senses stress—whether it’s a looming work deadline, an argument with a friend, financial pressure, or even excessive exercise—it activates the hypothalamic-pituitary-adrenal (HPA) axis. This is your body’s central stress response system. The hypothalamus signals the pituitary, which then tells your adrenal glands to release stress hormones like cortisol and adrenaline.
These hormones are useful in short bursts. They prime your body for “fight or flight.” But chronic stress? That’s a whole different story.
Elevated cortisol levels interfere with the hypothalamus’s ability to function normally. It stops producing gonadotropin-releasing hormone (GnRH), which is the hormone that starts the menstrual cycle. No GnRH means less FSH and LH. Less FSH and LH mean the ovaries don’t ovulate, and without ovulation, there’s no menstruation.
This is why high stress can lead to a missed period—or several. It’s not that your reproductive system is broken. It’s that your body, sensing a potential threat, is prioritizing survival over reproduction. It’s your biology’s way of saying, “Now is not a safe time for pregnancy.”
The Many Faces of Stress
When we talk about stress, it’s easy to think of it as purely emotional or mental. But stress is multifaceted, and the body doesn’t always differentiate between types. All it knows is that something is out of balance.
Acute stress—like a breakup, a move, or an exam—can delay ovulation, which can delay your period. Chronic stress—like long-term caregiving, a toxic work environment, or unresolved trauma—can cause more profound disruptions. Over time, if the stress persists, you may develop a condition called hypothalamic amenorrhea: a fancy way of saying that your brain has stopped sending the signals needed for your period to arrive.
Even “positive” stressors like planning a wedding, starting a new job, or traveling extensively can take a toll. If your lifestyle includes intense exercise and calorie restriction (hello, training for a marathon or adhering to a strict diet), those physical stressors can impact your cycle just as significantly as emotional ones.
The Vicious Cycle of Stress and Worry
Ironically, missing a period can become its own source of stress. You start worrying—Is something wrong with me? Could I be pregnant? Is this early menopause? That worry creates more stress, and the cycle continues. The very act of being stressed about your missed period may further delay it.
This feedback loop can feel maddening. Each day without your period adds a layer of anxiety, which only increases cortisol levels, which in turn further suppresses your reproductive hormones. It becomes a cycle of silence, one that plays out month after month if the root cause isn’t addressed.
Real-Life Stories, Real Hormonal Chaos
Meet Sara. She’s 29, a high-achieving graphic designer in New York. Her life is a blur of client meetings, late nights, and morning workouts. She eats clean, sleeps little, and runs on ambition—and caffeine. When her period stopped coming, she was alarmed. Pregnancy test? Negative. STI screening? Clear. Ultrasound? Normal. Her doctor asked about stress, and she laughed. “Of course I’m stressed,” she said. “Isn’t everyone?”
Then there’s Amira, a college student juggling a double major, part-time job, and caregiving responsibilities for a sick parent. She missed three periods in a row before finally realizing her body was crying out for rest. Her missed periods were not random—they were a reflection of her overwhelmed nervous system.
These stories aren’t rare. They’re echoes of a larger truth: that modern life often demands more from us than our bodies can safely give, and when we push too hard, menstruation is one of the first systems to go offline.
The Role of Cortisol and the Domino Effect
Cortisol isn’t just a hormone with a bad reputation. In healthy amounts, it regulates blood pressure, metabolism, and immune function. But when it’s chronically elevated, it starts pulling strings in all the wrong directions.
High cortisol suppresses GnRH, as mentioned, but it also alters thyroid function. The thyroid gland plays a huge role in reproductive health, and even subtle shifts can lead to cycle irregularities. High cortisol can reduce conversion of the inactive thyroid hormone (T4) to its active form (T3), which can mimic or lead to hypothyroidism—a known disruptor of menstrual cycles.
Cortisol also impacts blood sugar regulation and insulin sensitivity. Women with conditions like PCOS (polycystic ovary syndrome) already have challenges with insulin and androgens. Add stress to the mix, and the hormonal stew thickens, pushing the cycle even further off course.
Then there’s prolactin, a hormone often associated with breastfeeding. Under stress, prolactin levels can rise. In elevated amounts, prolactin inhibits ovulation. It’s yet another example of how your body, under duress, puts reproductive health on the back burner.
Your Brain Is the Boss
The common denominator in all these disruptions is the brain. Specifically, the hypothalamus and pituitary—often called the “master glands.” They regulate everything from cortisol to estrogen to ovulation itself. When stress scrambles their communication, reproductive hormones go quiet.
That’s why periods are such sensitive barometers of overall health. When the brain senses that life is too chaotic, too threatening, or too energy-depleting, it decides that now is not the time for reproduction. And it pulls the plug on menstruation.
How to Know If Stress Is the Cause
Not all missed periods are caused by stress. Thyroid disorders, significant weight changes, polycystic ovary syndrome, perimenopause, and certain medications can all disrupt your cycle. That’s why it’s important to consult a healthcare provider if your period is irregular or missing.
But if you’ve ruled out medical causes, take a closer look at your lifestyle. Are you sleeping enough? Eating regularly? Pushing yourself too hard? Carrying chronic emotional burdens?
Sometimes your body knows what your mind won’t admit. A missed period can be a message in a bottle—a signal from your nervous system saying, “Something needs to change.”
The Road Back to Balance
Getting your period back after stress isn’t always instant. It requires patience, compassion, and often a radical reevaluation of your relationship with rest. The first step is acknowledging the role stress plays, not just mentally but physically.
Reducing stress doesn’t mean quitting your job and moving to the woods (though wouldn’t that be nice?). It means building buffers into your day—rest, boundaries, joy. It means sleeping at least seven hours a night, eating enough calories (especially healthy fats), and moving your body in ways that feel nourishing, not punishing.
For some women, practices like yoga, mindfulness meditation, or journaling can help calm the nervous system. Others may benefit from therapy, especially if stress is linked to trauma or anxiety. Adaptogenic herbs like ashwagandha and rhodiola are sometimes used to support adrenal health, but they should be used with guidance.
In time, as cortisol levels fall and hormonal communication resumes, the menstrual cycle often returns. It may come back irregularly at first, but with sustained care, many women regain their natural rhythm.
The Bigger Picture
Periods are not just a monthly inconvenience. They’re a vital sign—like blood pressure, pulse, or temperature. They reflect the internal state of your body and mind. When your period goes missing, it’s not just about reproduction. It’s about health, balance, and the often-unseen toll that stress takes on your body.
The connection between stress and missed periods isn’t just theoretical. It’s deeply biological, and deeply human. We are not machines. We are cyclical, sensitive, and responsive beings. When life becomes too much, our bodies let us know. And the absence of a period is often their quiet cry for help.
Reclaiming Your Cycle, Reclaiming Yourself
In a world that glorifies busyness and undervalues rest, honoring your menstrual cycle can feel like an act of rebellion. But it’s also an act of self-respect. Listening to your body when it whispers—before it has to scream—is how healing begins.
Stress will always be part of life. But chronic, unrelenting stress doesn’t have to be. Your period is not your enemy. It’s a messenger. And when it disappears, it’s worth asking not just “what’s wrong with my hormones?” but “what’s happening in my life?”
Reclaiming your cycle means reclaiming your right to rest, your right to nourish yourself, and your right to exist outside the grind. Because your body deserves more than survival—it deserves to thrive.