Stress is invisible. It doesn’t show up on your skin like a rash. It doesn’t appear on an X-ray like a broken bone. But inside your body—especially inside your heart—stress can be just as damaging as any physical injury. It hums in the background like a low-voltage current, sometimes buzzing quietly, sometimes surging like a thunderstorm. And while you may not always feel it, your heart does.
We often think of stress as an emotional state, a mental response to life’s demands. But stress is also profoundly physical. It shapes the rhythm of your heartbeat, the pressure in your arteries, and even the electrical impulses that keep your heart pumping. Chronic stress can make your heart race, your blood vessels constrict, and your risk of heart disease skyrocket. It is both silent and dangerous—a sneaky saboteur of cardiovascular health.
Understanding how stress affects your heart is about more than managing emotions. It’s about recognizing that your emotional life and your heart health are deeply, inseparably connected. And once you understand that connection, you can take steps not only to feel better but to live longer and stronger.
The Biology of Stress: A Quick Look Under the Hood
To understand stress’s impact on the heart, we first need to understand what stress is at a biological level. When your brain perceives a threat—real or imagined—it sounds an alarm. This alarm activates the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system. Together, they release a cascade of stress hormones: adrenaline (epinephrine) and cortisol being the main players.
Adrenaline speeds up your heart rate, raises your blood pressure, and floods your muscles with glucose for quick energy. Cortisol, meanwhile, helps prolong the stress response by altering metabolism, immune function, and mood. In small doses, this system works perfectly. It’s designed to keep you alive in emergencies—like when you’re running from a bear.
But modern stress isn’t about bears. It’s about bills, deadlines, traffic jams, breakups, burnout, and bad news. And these stressors don’t just come and go. They hang around. The result? A chronic activation of the stress response—a steady drip of adrenaline and cortisol that wears down your heart over time.
The Heart Under Pressure: Immediate Effects of Acute Stress
Think about the last time you were startled or scared. Maybe someone jumped out at you, or you almost got into a car accident. Your heart likely leapt in your chest, your breathing quickened, and you felt a sudden jolt of energy. This is your body’s acute stress response, often called the “fight or flight” reaction.
During this response, your body prepares for action. Your heart pumps faster and harder to deliver oxygen and nutrients to your muscles. Your blood vessels constrict, raising your blood pressure. Platelets in your blood become stickier, ready to clot in case of injury. All of this is fine—if you actually need to fight or flee.
But even brief surges of stress can be dangerous if they happen too often or in people with underlying heart conditions. Acute emotional stress can trigger events like:
- Heart palpitations or arrhythmias (abnormal heart rhythms)
- Angina (chest pain due to reduced blood flow to the heart)
- Heart attack (especially in people with existing coronary artery disease)
- Takotsubo cardiomyopathy, also known as “broken heart syndrome”
Acute stress doesn’t just feel intense—it can be physiologically intense too, especially for your heart.
Broken Heart Syndrome: When Emotion Mimics a Heart Attack
Takotsubo cardiomyopathy is one of the most dramatic examples of how stress can affect the heart. Named after a Japanese octopus trap (because of the way the heart balloons out at the bottom during the episode), this condition is triggered by extreme emotional stress—like the death of a loved one, a breakup, or even a surprise party gone wrong.
It presents exactly like a heart attack: chest pain, shortness of breath, and changes on an EKG. But unlike a traditional heart attack, there’s no blocked artery. Instead, the heart muscle becomes temporarily stunned and weakened, unable to pump efficiently.
Most people recover fully within weeks, but the fact that a broken heart can literally break your heart is a chilling reminder of the emotional-physical connection.
Chronic Stress: A Slow Burn for the Cardiovascular System
If acute stress is a thunderclap, chronic stress is a smoldering fire. Day in and day out, low-grade stress keeps your heart on high alert. The constant exposure to cortisol and adrenaline changes the way your cardiovascular system operates.
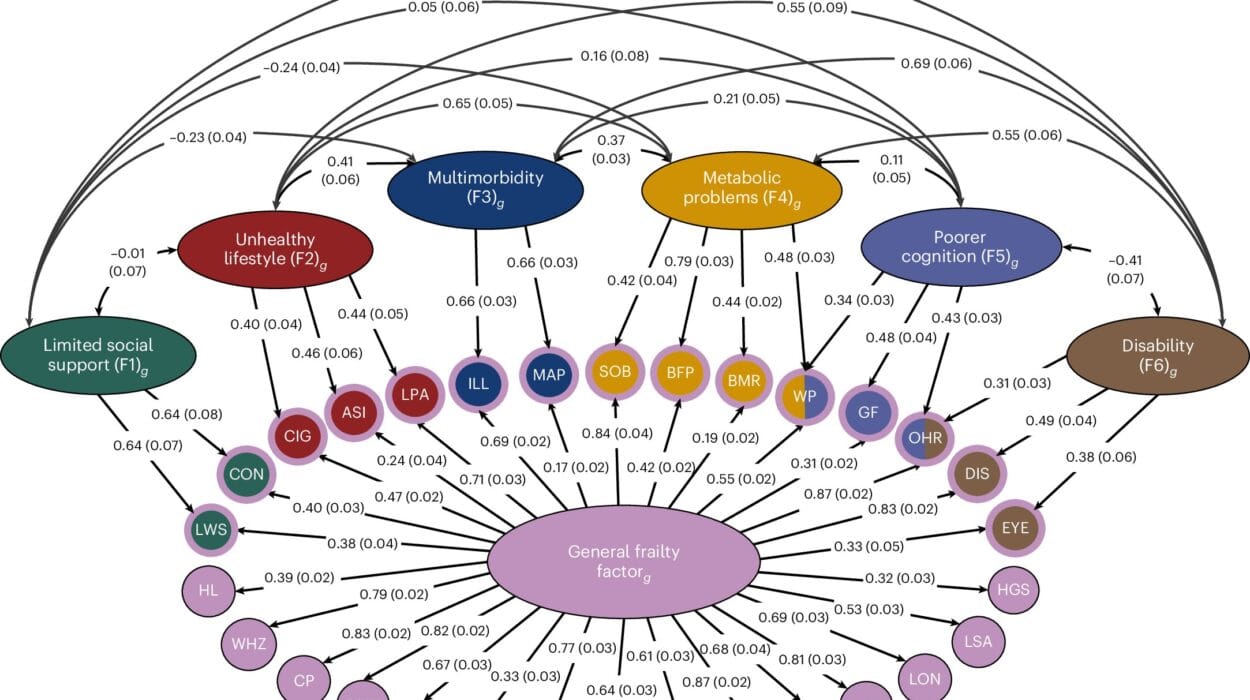
Here’s what chronic stress does over time:
- Raises blood pressure persistently, straining your arteries
- Elevates resting heart rate, forcing your heart to work harder
- Promotes inflammation, a key player in the development of atherosclerosis (hardening of the arteries)
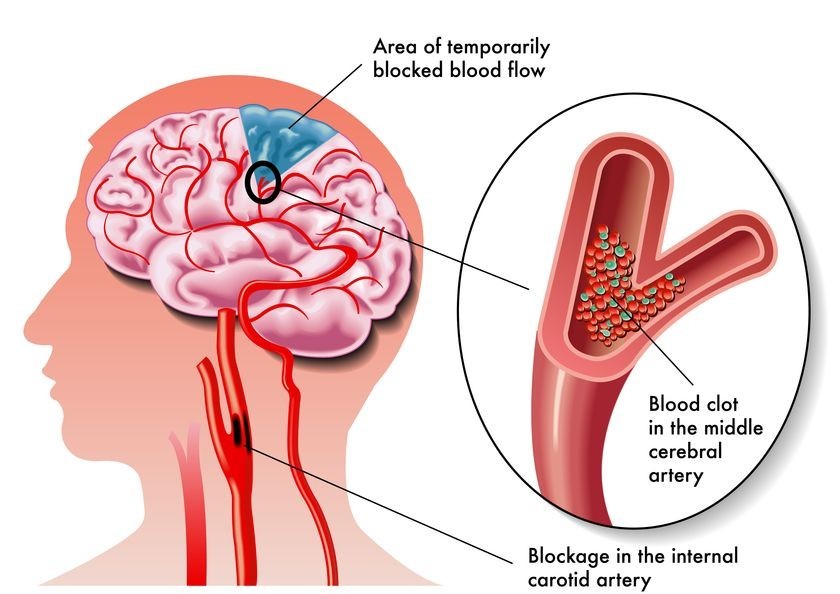
- Encourages plaque buildup in the arteries, increasing the risk of heart attack and stroke
- Contributes to insulin resistance, a precursor to diabetes—another heart disease risk factor
- Disrupts lipid metabolism, raising bad cholesterol (LDL) and lowering good cholesterol (HDL)
In essence, chronic stress doesn’t just make you feel tense—it ages your arteries, tires out your heart, and distorts your metabolic balance. It creates a hostile environment inside your body, where disease can take root.
Stress and Unhealthy Coping: When the Cure Becomes the Problem
How we respond to stress can be just as harmful as the stress itself. Many people turn to food, alcohol, cigarettes, or even complete inactivity as a way of coping. These behaviors might offer short-term relief, but they come with long-term costs to the heart.
Emotional eating—especially high in sugar and fat—leads to weight gain, insulin resistance, and increased heart disease risk. Alcohol raises blood pressure, damages the heart muscle, and increases arrhythmia risk. Smoking, often triggered by stress, accelerates the formation of plaques in arteries and decreases oxygen supply to the heart.
Even seemingly benign behaviors, like binge-watching TV or isolating oneself, contribute to a sedentary lifestyle and poor cardiovascular conditioning. When stress leads us to self-destructive habits, it multiplies its impact on heart health.
The Connection Between Stress and Hypertension
One of the most direct links between stress and heart disease is high blood pressure, or hypertension. While the role of stress in chronic hypertension is still debated, there’s no doubt that stress raises blood pressure in the short term—and frequent surges can contribute to long-term problems.
Every time your blood pressure spikes, it puts force on the walls of your arteries. Over time, this pressure causes tiny tears, inflammation, and stiffness in the blood vessels. These changes make it easier for plaque to accumulate and harder for your heart to pump efficiently.
Some people are more sensitive to stress-induced blood pressure changes than others. This “reactivity” can be influenced by genetics, personality, life experiences, and even childhood trauma. In these individuals, stress may be a primary driver of hypertension.
Cortisol and the Heart: The Hormone That Doesn’t Know When to Quit
Cortisol is often called the “stress hormone,” and for good reason. It’s involved in nearly every aspect of the stress response, from raising blood sugar to regulating metabolism and immune activity. But when cortisol stays elevated too long, it becomes a wrecking ball for your cardiovascular system.
High cortisol levels are linked to:
- Increased belly fat, which is metabolically active and contributes to heart disease
- Elevated blood sugar and insulin resistance
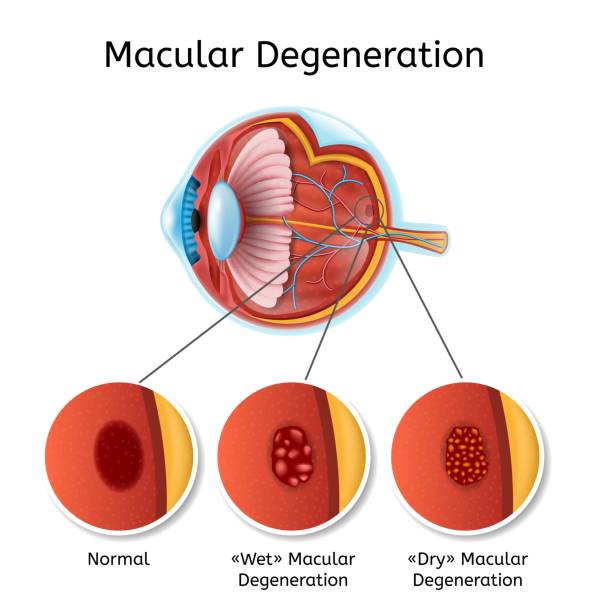
- Suppressed immune function, which affects the repair of blood vessels
- Disrupted sleep patterns, which are crucial for heart health
- Mood disorders, which can indirectly increase cardiovascular risk
Cortisol is not inherently bad—it’s vital for survival. But in a world where stress never sleeps, neither does cortisol. And your heart pays the price.
Sleep, Stress, and the Night Shift of Your Heart
Sleep is the body’s natural reset button. It’s during sleep that your heart rate slows, blood pressure drops, and your cardiovascular system recovers from the day’s demands. But stress often disrupts sleep—making it harder to fall asleep, stay asleep, or achieve deep, restorative rest.
Sleep deprivation, in turn, raises cortisol levels, increases appetite for unhealthy food, and leads to higher blood pressure. It’s a vicious cycle: stress disrupts sleep, poor sleep worsens stress, and both increase heart disease risk.
People with chronic insomnia or sleep apnea—conditions often exacerbated by stress—have significantly higher rates of hypertension, arrhythmias, and heart attacks. Protecting your sleep is one of the most heart-protective things you can do.
Personality Types and Stress Vulnerability
Not everyone reacts to stress the same way. Your personality type can influence how stress affects your heart. For example:
- Type A personalities—competitive, driven, impatient—are more prone to heart disease, especially if they are also hostile or angry.
- People with high anxiety tend to have higher heart rate variability and more stress reactivity.
- Chronic worriers and perfectionists often experience long-term stress, even in the absence of immediate threats.
- Optimists and resilient individuals, on the other hand, show lower stress-induced damage to the heart and better recovery after cardiac events.
Your mindset doesn’t just shape your experiences—it shapes your biology. Cultivating emotional resilience, gratitude, and mindfulness isn’t just feel-good advice—it’s heart therapy.
Mind-Body Practices: How Calming the Mind Calms the Heart
If stress can wound the heart, then peace can help heal it. Mind-body practices like meditation, yoga, deep breathing, and progressive muscle relaxation have all been shown to benefit cardiovascular health by calming the autonomic nervous system.
These practices help shift your body from the sympathetic (fight or flight) state into the parasympathetic (rest and digest) state. When this happens:
- Heart rate slows down
- Blood pressure decreases
- Blood vessels relax and dilate
- Inflammation markers decrease
- Cortisol levels drop
- Emotional regulation improves
Mindfulness meditation, in particular, has been studied extensively. Regular practice can reduce resting heart rate, lower blood pressure, and even improve outcomes after heart surgery or heart attacks. It doesn’t require special equipment or a therapist—just your attention and your breath.
Yoga combines physical movement, breath control, and mindfulness into one powerful stress-reduction tool. Even gentle forms of yoga can significantly lower blood pressure and improve heart rate variability, an important marker of cardiovascular resilience.
Breathing exercises, such as box breathing or 4-7-8 breathing, work by directly stimulating the vagus nerve—a nerve that helps control heart rate and parasympathetic activity. With consistent practice, these techniques can shift your heart’s baseline rhythm into a calmer, steadier beat.
Emotional Support and Social Connection: Medicine for the Heart
Humans are social creatures, wired for connection. And the heart, it turns out, thrives on connection just as much as the mind. Social support acts as a powerful buffer against stress. People with strong social ties tend to live longer, recover faster from illness, and have better heart health overall.
Conversely, loneliness and social isolation are associated with higher levels of stress hormones, increased inflammation, and a greater risk of heart attack and stroke. In fact, being socially disconnected can be as harmful to your heart as smoking or obesity.
Talking to someone you trust, whether it’s a friend, family member, therapist, or spiritual guide, can significantly reduce your body’s stress response. Sharing burdens makes them lighter. Laughing with others calms the nervous system. Crying in the presence of empathy can bring physical relief.
Support groups, online communities, religious gatherings—these aren’t just emotional lifelines. They are physiological lifelines, too. They give your heart a reason to beat with strength and hope.
The Role of Exercise: A Double-Edged Sword?
Exercise is one of the most powerful tools for heart health—and also one of the best antidotes to stress. Regular physical activity lowers cortisol, boosts mood, and strengthens the heart muscle. It improves blood flow, increases oxygen delivery, and promotes the release of endorphins—your body’s natural feel-good chemicals.
But it’s important to remember that exercise is also a form of physical stress. When done excessively or in the absence of recovery, intense exercise can actually increase inflammation and stress hormones. This is especially true for endurance athletes or people pushing themselves beyond their limits without adequate sleep, nutrition, or hydration.
The key is balance. Moderate, consistent activity—like brisk walking, swimming, cycling, or dancing—has the most heart-friendly effects. These movements promote parasympathetic dominance, improve heart rate variability, and build resilience against future stressors.
In short, move your body, but don’t punish it. Let exercise be an act of kindness, not aggression.
Nutrition, Stress, and the Heart’s Chemistry
What you eat during stressful times can either soothe your heart or strain it further. Unfortunately, many people reach for comfort foods—high in sugar, salt, and unhealthy fats—that can inflame the cardiovascular system and raise blood pressure.
Chronic stress also alters appetite-regulating hormones like ghrelin and leptin, leading to overeating or undereating. It promotes fat storage around the abdomen, where it poses the greatest risk to heart health.
A heart-smart, stress-reducing diet includes:
- Omega-3 fatty acids (found in fatty fish, flaxseeds, walnuts) which reduce inflammation and stabilize mood
- Leafy greens and colorful vegetables rich in antioxidants and magnesium
- Whole grains that stabilize blood sugar and reduce cortisol spikes
- Fermented foods that support gut health (which is linked to mood and stress resilience)
- Dark chocolate (in moderation), which may lower blood pressure and reduce cortisol levels
Hydration also matters. Dehydration increases cortisol and makes the heart work harder. Drinking enough water is a simple, often overlooked, way to ease the burden on your cardiovascular system.
Childhood Stress and Lifelong Heart Risk
Stress doesn’t just affect adults. In fact, adverse childhood experiences (ACEs)—such as abuse, neglect, or household dysfunction—can set the stage for lifelong cardiovascular problems. The developing brain and body are especially vulnerable to stress, and early trauma can hardwire the stress response system into a hyperactive state.
Adults with a history of ACEs are more likely to develop hypertension, diabetes, obesity, and heart disease. They’re also more prone to depression, anxiety, and substance abuse—all of which compound heart risk.
But here’s the good news: awareness leads to healing. Early intervention, therapy, trauma-informed care, and community support can reverse much of the damage. The brain and heart are plastic—they can adapt, grow, and recover. It’s never too late to rewrite your story.
Stress Management as Preventive Cardiology
Too often, we treat heart disease after it has already taken root. But what if we approached stress management the same way we approach cholesterol or blood pressure control? What if we saw mental wellness as heart medicine?
Preventive cardiology must include:
- Stress screening during routine check-ups
- Referrals to counseling or therapy for chronic stress or trauma
- Workplace wellness programs that address burnout and work-life balance
- Public health campaigns that promote emotional literacy and resilience
- Integration of meditation and mindfulness into schools, hospitals, and communities
Just as we prescribe statins and antihypertensives, we should be prescribing stress-reduction strategies. Because a calm mind creates a strong heart.
When to Worry: Red Flags for Stress-Related Heart Trouble
Not all chest pain is a heart attack, and not all palpitations are life-threatening. But chronic stress symptoms should never be ignored—especially if they involve the heart.
Warning signs include:
- Chest pain or pressure, especially during emotional upset
- Shortness of breath unrelated to physical exertion
- Heart palpitations, fluttering, or irregular beats
- Dizziness or lightheadedness under stress
- Sudden fatigue or fainting
- High blood pressure that resists medication
If you experience these, it’s essential to seek medical advice. Sometimes, the heart’s cries for help are whispered through stress signals before they scream through heart attacks.
Healing the Heart: The Journey Forward
Healing from stress is not about eliminating it entirely—that’s impossible. Life will always bring challenges, heartbreaks, and uncertainties. But healing is about changing your relationship to stress. It’s about reclaiming agency over your emotional and physical responses.
It begins with awareness—learning to recognize the signals your body sends. It continues with action—building habits that restore balance. And it’s sustained through compassion—for yourself, your story, and your journey.
The heart is a powerful organ. It beats over 100,000 times a day without your asking. It adapts, it recovers, and, given the right conditions, it thrives. Don’t wait for a scare to start protecting it. Don’t wait for silence to begin listening.
Every calming breath you take, every kind word you speak, every act of self-care you offer yourself—these are not small things. They are signals to your heart: you are safe, you are strong, and you are loved.
Conclusion: The Heart Remembers
The heart doesn’t just pump blood. It remembers. It keeps the rhythm of your laughter, the ache of your losses, the joy of your triumphs. It remembers every surge of stress, every flood of relief, every moment of love.
Stress is part of life. But it doesn’t have to rule your life—or damage your heart. Through mindfulness, connection, movement, nourishment, and rest, you can create a sanctuary inside your body, a place where the heart feels supported, not attacked.
Let your heart be more than a machine. Let it be a guide, a barometer, a companion. And above all, let it be protected—because the heart you save might just be your own.