Bacteria, among the oldest life forms on Earth, are single-celled organisms that exist in virtually every environment, from the air we breathe to the soil beneath our feet. While many bacteria are harmless, even beneficial, certain types can cause diseases, leading to what we know as bacterial infections. These infections are caused when harmful bacteria invade the body and disrupt normal biological processes.
Unlike viral infections, which require a host cell to replicate, bacteria can reproduce independently, often making them formidable foes. In some cases, bacteria are so powerful that they can overpower the body’s natural defenses, leading to illnesses ranging from mild, such as strep throat, to severe, such as pneumonia or sepsis. Understanding bacterial infections involves delving into the science of how bacteria operate, how they interact with our bodies, and what can be done to treat them effectively.
The Anatomy of Bacteria: How They Invade the Body
Bacteria are incredibly diverse, and not all bacteria are bad. In fact, many are essential for life—helping digest food, producing vitamins, and protecting us from harmful pathogens. However, when harmful bacteria infiltrate the body, they can wreak havoc. These pathogens typically enter through cuts, inhalation, ingestion, or sexual contact, and then begin to multiply, often leading to an infection.
The structure of bacteria makes them highly adaptable and resilient. They have a cell wall, cell membrane, and internal components that allow them to thrive in different environments. For example, Gram-positive bacteria have a thick outer wall that resists many antibiotics, while Gram-negative bacteria have a more complex structure with an outer membrane that can make them harder to treat.
Once bacteria invade the body, they can secrete toxins that damage tissues, impair immune responses, and cause inflammation. This can lead to the symptoms of infection, including fever, swelling, and pain. The body responds by activating the immune system, which sends white blood cells to combat the bacteria. However, if the bacteria are particularly virulent or the immune response is inadequate, the infection can spread, causing more severe complications.
Signs and Symptoms of a Bacterial Infection
The symptoms of a bacterial infection can vary significantly depending on the type of bacteria involved, the area of the body affected, and the individual’s overall health. However, there are some common signs that may indicate a bacterial infection is at work.
Localized Symptoms: Red, Swollen, and Painful
If the infection is localized, it may result in symptoms such as redness, swelling, pain, or warmth in the affected area. For example, a skin infection caused by Staphylococcus aureus can lead to a boil, abscess, or cellulitis, with these hallmark signs of inflammation. Similarly, an ear infection caused by bacteria can lead to pain and a feeling of fullness in the ear, sometimes with a yellow or green discharge.
Systemic Symptoms: Fever, Fatigue, and Chills
When the infection spreads throughout the body, it can trigger systemic symptoms. A fever is a common response to bacterial infections, as the body raises its temperature in an attempt to create an environment inhospitable to the bacteria. Chills, sweats, and fatigue are also common as the body fights the infection, often leading to a feeling of general malaise.
In some cases, the infection can lead to sepsis, a life-threatening condition in which the body’s immune system goes into overdrive, causing widespread inflammation. Symptoms of sepsis include rapid breathing, confusion, a dangerously high or low heart rate, and a drop in blood pressure. Sepsis requires immediate medical intervention, as it can rapidly lead to organ failure and death.
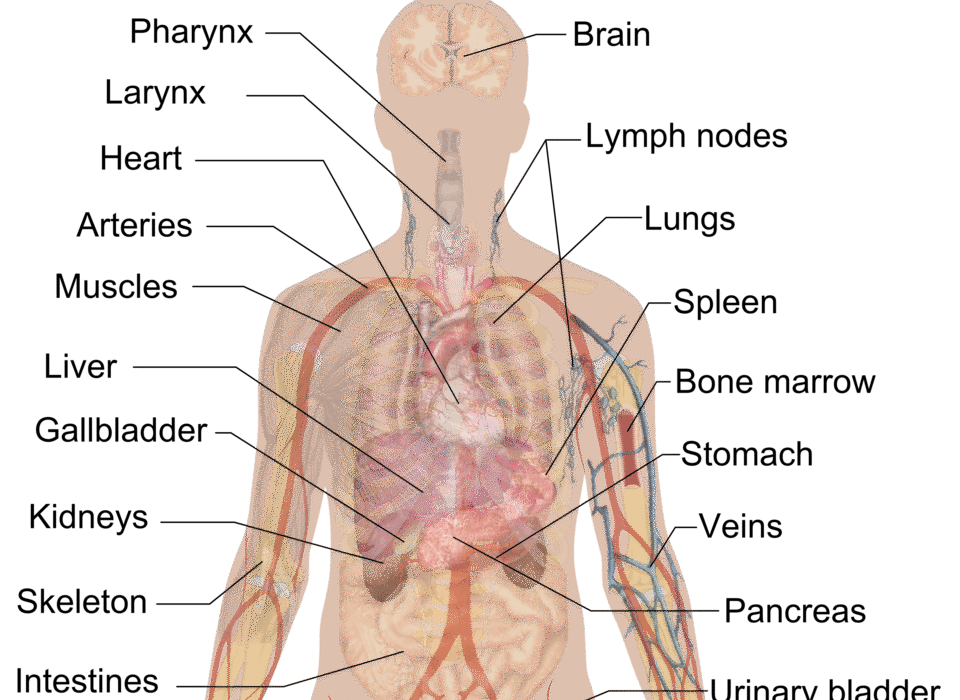
Organ-Specific Symptoms: From Respiratory to Urinary Infections
Bacterial infections often target specific organs, and the symptoms will depend on where the infection occurs. For instance, a respiratory infection caused by Streptococcus pneumoniae can lead to coughing, shortness of breath, chest pain, and, in more severe cases, pneumonia. A urinary tract infection (UTI), caused by bacteria such as Escherichia coli, may cause painful urination, urgency, and cloudy or bloody urine.
If the infection reaches the bloodstream, it can cause bacteremia, which can spread rapidly to other organs, making the infection even more dangerous.
Risk Factors for Bacterial Infections: Who Is Most Vulnerable?
While bacterial infections can affect anyone, certain groups of people are at a higher risk due to various factors, such as age, underlying health conditions, lifestyle, and even genetic predispositions. Understanding these risk factors is key to prevention and early intervention.
Age: The Young and the Elderly
Both infants and the elderly are particularly susceptible to bacterial infections. Babies have underdeveloped immune systems, making them vulnerable to pathogens. In contrast, older adults often experience a decline in immune function, as well as chronic conditions like diabetes or heart disease, which can increase their risk of developing severe infections. For example, elderly individuals are at higher risk for infections like pneumonia and urinary tract infections.
Chronic Health Conditions: A Breach in Defense
Chronic diseases such as diabetes, cancer, HIV/AIDS, and liver or kidney disease can compromise the body’s ability to fend off infections. For instance, diabetes can lead to poor circulation, which increases the likelihood of skin infections, while patients undergoing chemotherapy for cancer have weakened immune systems, making them more prone to bacterial infections.
Lifestyle Factors: Hygiene, Diet, and Habits
Certain lifestyle factors can also increase the risk of bacterial infections. Poor hygiene, such as infrequent handwashing or improper food handling, can introduce harmful bacteria into the body. Unprotected sexual activity increases the risk of contracting sexually transmitted bacterial infections, such as gonorrhea, chlamydia, or syphilis.
Diet also plays a role in immunity. A lack of essential vitamins and minerals can weaken the immune system, making the body more vulnerable to infections. Smoking and alcohol consumption, which both affect the immune system and respiratory tract, can also heighten the risk of infections like pneumonia.
Environmental Exposure: Hospitals and the Outdoors
Certain environments can increase the likelihood of exposure to harmful bacteria. For instance, healthcare settings, despite rigorous infection control measures, can harbor antibiotic-resistant bacteria like Methicillin-resistant Staphylococcus aureus (MRSA). These bacteria can be difficult to treat and cause serious complications. Similarly, outdoor activities like hiking in areas with contaminated water sources or contact with animals can lead to bacterial infections such as Lyme disease or Leptospirosis.
Diagnosing a Bacterial Infection: The Path to Identification
When a bacterial infection is suspected, a healthcare provider will often begin with a physical examination, looking for signs of infection like redness, swelling, or fever. However, diagnosing a bacterial infection usually requires laboratory tests to identify the specific bacteria involved and determine the most effective treatment.
One of the most common diagnostic tools is the culturing of bacteria. This involves taking a sample from the infected area—whether it’s blood, urine, sputum, or tissue—and allowing the bacteria to grow in a controlled environment. Once the bacteria have grown, they can be examined under a microscope, and their specific characteristics can be analyzed.
In addition to culturing, molecular techniques like polymerase chain reaction (PCR) can be used to identify bacterial DNA or RNA. This method is faster and more sensitive than traditional culturing, allowing for quicker diagnoses, especially in cases where the bacteria are difficult to grow in the lab.
Treating Bacterial Infections: The Power of Antibiotics
The advent of antibiotics revolutionized the treatment of bacterial infections. Antibiotics work by either killing bacteria or inhibiting their growth, allowing the body’s immune system to take over and eliminate the infection. However, not all bacterial infections require antibiotics, and the decision to use them must be made carefully.
Antibiotics: A Double-Edged Sword
Antibiotics have saved millions of lives since their discovery, but their widespread use has led to a serious problem: antibiotic resistance. When bacteria are exposed to antibiotics over time, they can develop mechanisms to survive them, leading to the emergence of so-called “superbugs” that are resistant to common antibiotics. MRSA, Vancomycin-resistant enterococci (VRE), and drug-resistant tuberculosis are just a few examples of the growing list of antibiotic-resistant bacteria.
Doctors now aim to use antibiotics only when necessary, prescribing them for bacterial infections that are confirmed or strongly suspected. The type of antibiotic prescribed depends on the type of bacteria causing the infection. For example, penicillin is commonly used for infections caused by Streptococcus species, while macrolides like azithromycin are used for respiratory infections.
The Role of Supportive Care
In addition to antibiotics, supportive care plays a crucial role in managing bacterial infections. This can include rest, hydration, and fever reduction to help the body’s immune system fight the infection. In some cases, surgery may be required to drain abscesses or remove infected tissue.
For severe infections, hospitalization may be necessary, especially if the infection is causing complications like sepsis. Intravenous (IV) antibiotics may be administered to ensure the drugs reach the bloodstream quickly and effectively.
Preventing Bacterial Infections: A Proactive Approach
While bacterial infections can be treated effectively with the right medications, prevention is always better than cure. Proper hygiene, vaccination, and healthy lifestyle choices can all reduce the risk of infection.
Hygiene and Sanitation
Good hygiene is one of the most effective ways to prevent bacterial infections. Regular handwashing with soap and water, especially after using the bathroom, handling food, or coughing, can prevent the spread of bacteria. Similarly, ensuring food is cooked to the right temperature and avoiding cross-contamination can help prevent foodborne infections.
Vaccination
Vaccines are available for certain bacterial infections, such as tuberculosis, pneumococcus, and meningococcus. These vaccines help prepare the immune system to recognize and fight off specific bacteria, significantly reducing the risk of illness.
Boosting the Immune System
Maintaining a healthy lifestyle can help strengthen the immune system and reduce the likelihood of bacterial infections. Eating a balanced diet, staying physically active, getting enough sleep, and avoiding smoking or excessive alcohol use can all help keep the immune system strong and capable of defending against harmful bacteria.
Conclusion: The Ongoing Battle Against Bacteria
Bacterial infections are a common part of life, but they remain a significant health threat, especially as antibiotic resistance continues to rise. Understanding how bacteria work, recognizing the symptoms of infection, and knowing the risks can help us stay vigilant and take action when necessary.
Thanks to antibiotics, most bacterial infections can be treated effectively. However, the rise of resistant bacteria calls for a more nuanced approach to their use. As we continue to fight this microbial battle, it’s important to remember that prevention is key, and a healthy lifestyle can go a long way in keeping us free from the harmful effects of bacterial infections.