Fungal infections are not typically the first thing that comes to mind when we think of diseases. We’re more likely to think about bacteria, viruses, or even parasites. Yet, in recent years, the conversation surrounding fungal infections has become more urgent. Once relegated to the background, fungi are now coming into sharper focus as a growing threat to human health, both in terms of frequency and severity.
There are several reasons for this shift, from the rise of drug-resistant fungal strains to environmental changes that favor the growth of these organisms. But to understand why fungal infections are on the rise, we first need to grasp the basics of how they work. What exactly are fungi? How do they invade our bodies, and what makes them so tricky to treat?
What Are Fungi? The Invisible Organisms Among Us
Fungi are a diverse group of organisms that includes molds, yeasts, and mushrooms. They exist all around us, in the air, on surfaces, in the soil, and even inside our bodies. They belong to their own kingdom in the biological classification system, separate from plants, animals, and bacteria. Unlike plants, fungi do not photosynthesize, but instead rely on organic matter for nourishment. Some fungi are harmless, playing essential roles in decomposing organic material and recycling nutrients in ecosystems. However, others are opportunistic pathogens, capable of causing a wide range of infections when the conditions are right.
Fungal infections can affect various parts of the body, ranging from superficial skin conditions like athlete’s foot or ringworm to systemic infections that impact internal organs. These infections typically occur when the fungus overwhelms the body’s immune defenses, particularly in individuals with weakened or compromised immune systems.
How Fungal Infections Take Hold: The Pathogenesis
The process by which fungal infections develop in the body involves several steps, each of which underscores the resilience and adaptability of fungi as pathogens. The first step is exposure to fungal spores or conidia, which are microscopic cells capable of reproducing and spreading. These spores can be inhaled, ingested, or come into contact with the skin.
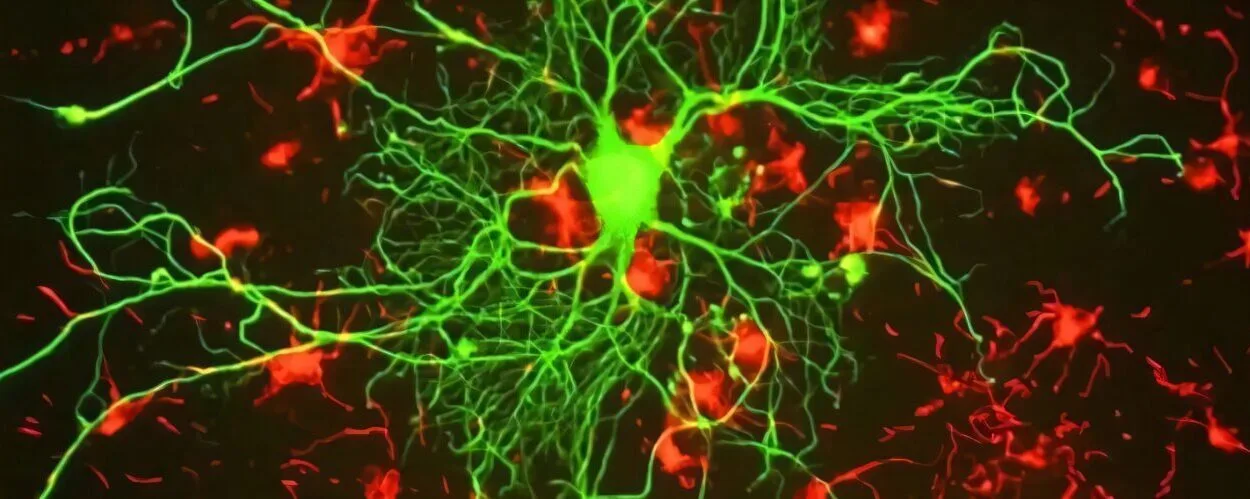
Once inside the body, the fungus begins to establish itself. The environment within the human body is not always hospitable to fungi, so they must adapt to various defenses. The body’s immune system is constantly on alert for pathogens like fungi, but fungi have evolved to evade detection and neutralization in a variety of ways. For instance, they can change their morphology, transitioning from a benign yeast form to a more invasive mold form that can penetrate tissues.
Fungi also produce enzymes that break down host tissues, allowing them to invade deeper layers of skin, mucous membranes, or even internal organs. In some cases, they form biofilms—clusters of cells encased in a slimy, protective matrix—that make it difficult for the immune system or antifungal treatments to reach them effectively.
One of the most dangerous aspects of fungal infections is their ability to spread through the bloodstream, causing systemic infections that can reach the heart, lungs, kidneys, or brain. These types of infections, known as invasive mycoses, are often life-threatening and can be difficult to diagnose due to their nonspecific symptoms, such as fever, fatigue, and cough.
The Three Main Types of Fungal Infections
Fungal infections can be broadly categorized into three types based on their location and severity:
Superficial Infections
These are the most common and least serious fungal infections, often affecting the skin, hair, and nails. They include conditions like athlete’s foot, jock itch, and ringworm. While uncomfortable, these infections are typically treatable with topical antifungal medications. However, in some cases, they can lead to more serious complications if left untreated, particularly in people with weakened immune systems.
Subcutaneous Infections
These infections occur when fungi penetrate the deeper layers of the skin, often following a cut or wound. Subcutaneous fungal infections are rarer than superficial infections but can be more difficult to treat. The most well-known example of this type of infection is sporotrichosis, caused by the Sporothrix fungus, which commonly affects gardeners and farmers.
Systemic Infections
Systemic fungal infections are the most dangerous and occur when fungi spread throughout the body via the bloodstream. These infections can affect organs like the lungs, kidneys, brain, and heart, leading to potentially life-threatening conditions such as candidiasis, aspergillosis, and cryptococcosis. The immune system of healthy individuals can typically fight off these infections, but those with compromised immune systems—such as HIV/AIDS patients, cancer patients undergoing chemotherapy, or organ transplant recipients—are at much higher risk.
The Rise of Fungal Infections: A Global Health Concern
The increasing prevalence of fungal infections has become a growing concern for public health officials and researchers. In recent decades, several factors have contributed to the rise in both the frequency and severity of these infections. Some of the key reasons for this surge include:
Climate Change and Environmental Factors
Fungi are highly sensitive to environmental conditions such as temperature, humidity, and atmospheric CO2 levels. As the world’s climate warms, the conditions that favor fungal growth are becoming more widespread. Higher temperatures and increased rainfall create ideal habitats for fungi to thrive, particularly in regions where they previously struggled to survive.
Additionally, environmental changes have led to increased exposure to fungal spores. Wildfires, for example, release large amounts of fungal spores into the air, which can be inhaled by people over large geographic areas. Urbanization and deforestation also disturb natural habitats, driving fungi to adapt to new environments, including human homes and hospitals.
Antibiotic Use and Resistance
The overuse and misuse of antibiotics have played a significant role in the rise of fungal infections. While antibiotics are effective against bacterial infections, they have no impact on fungi. However, the widespread use of antibiotics can inadvertently promote fungal infections by disrupting the natural balance of microbes in the body.
The human microbiome is a delicate ecosystem that includes not just bacteria but also fungi. Antibiotic treatment can kill beneficial bacteria, allowing fungi such as Candida (which causes yeast infections) to overgrow. In some cases, this imbalance can lead to a condition called fungal dysbiosis, where pathogenic fungi dominate and cause infections.
Moreover, fungi themselves are evolving resistance to antifungal drugs. Just as bacteria have developed resistance to antibiotics, fungi are developing mechanisms to survive treatment with antifungal medications. This phenomenon is particularly concerning because antifungal drugs are already more limited in number and variety compared to antibiotics.
Immunocompromised Populations
A major driver of the rise in fungal infections is the growing number of people with weakened immune systems. Advances in medical treatments such as chemotherapy, organ transplants, and immunosuppressive therapies for autoimmune diseases have saved countless lives, but they also render individuals more vulnerable to infections—fungal infections included.
Patients with HIV/AIDS, for example, are at an increased risk for systemic fungal infections like cryptococcosis, a potentially fatal infection that affects the brain. Similarly, cancer patients undergoing chemotherapy have a higher likelihood of developing fungal infections due to the suppression of their immune systems. The same holds true for transplant recipients, whose bodies are often treated with immunosuppressive drugs to prevent organ rejection.
Globalization and Increased Travel
The world has never been more interconnected. Air travel, international trade, and migration have increased the spread of fungal spores across continents. A person exposed to a fungal infection in one country can bring the infection back to their home country, where it may spread to others. This globalization of fungal pathogens makes it more challenging to control outbreaks and prevent the spread of emerging fungal diseases.
For instance, Aspergillus species, which cause invasive lung infections, are found worldwide, but with the rise of international travel and global commerce, these fungi are becoming increasingly prevalent in new areas. Similarly, the emergence of Candida auris, a drug-resistant fungal pathogen, has been traced to several countries and is spreading rapidly in healthcare settings.
Diagnosis and Treatment: A Battle Against the Unknown
The diagnosis of fungal infections can be challenging. Unlike bacterial infections, which often have clear and easily recognizable symptoms, fungal infections can be subtle, with symptoms that overlap with other conditions. For example, an invasive fungal infection might present as a fever, fatigue, and cough, all of which can be attributed to a variety of other illnesses. This makes early diagnosis critical to prevent severe outcomes.
The gold standard for diagnosing fungal infections is laboratory testing, including blood cultures, tissue biopsy, and imaging scans. However, in many cases, fungal infections are not diagnosed until they have reached advanced stages. This delay in diagnosis contributes to the high mortality rate associated with systemic fungal infections.
Treating fungal infections has its own set of challenges. The antifungal drugs available today are limited and often come with significant side effects. In addition, the development of drug resistance, as mentioned earlier, is making it increasingly difficult to treat fungal infections effectively. Some fungal species, such as Candida auris, have become resistant to multiple classes of antifungal drugs, making treatment regimens much more complicated.
Research into new antifungal drugs is ongoing, but it has not kept pace with the emergence of drug-resistant fungi. There is also a need for more rapid diagnostic tools to catch fungal infections early, as well as vaccines to prevent fungal infections in high-risk populations.
The Future of Fungal Infections: Vigilance and Innovation
The rise of fungal infections represents a growing challenge for global health. However, it also underscores the importance of continued research, better diagnostics, and innovative treatment strategies. Scientists are increasingly focusing on the molecular biology of fungi, developing new drugs, and exploring the potential for vaccines.
As we continue to confront the global rise of fungal infections, it is crucial that both the public and the medical community remain vigilant. With the right resources, awareness, and innovation, we can better protect ourselves from these silent, resilient pathogens.