In the shadow of a world that has embraced antibiotics as its shield against infection, a new, silent adversary is emerging: antibiotic resistance. This global crisis, which threatens to render many of the life-saving drugs we rely on ineffective, is often described as a “slow-moving pandemic.” Unlike the viral outbreaks that seize the world’s attention with sudden force, antibiotic resistance creeps silently, insidiously, across borders, affecting people of all ages, ethnicities, and socioeconomic classes.
In the beginning, antibiotics were hailed as the triumph of modern medicine. They promised to vanquish bacterial infections that once claimed millions of lives. Yet, the unintended consequence of their widespread use has been the creation of more virulent strains of bacteria—microorganisms that no longer succumb to the drugs designed to kill them.
The danger is not theoretical. Each year, more than 700,000 people die due to antibiotic-resistant infections. Experts warn that by 2050, this figure could rise to 10 million. This would make antibiotic resistance a leading cause of death, surpassing even cancer. As the global population grows, urbanizes, and becomes more interconnected, the threat of antibiotic resistance looms larger. The question is no longer if we will face an epidemic of untreatable diseases, but when.
The Birth of Antibiotics: A Miracle That Changed Medicine
Before antibiotics, bacterial infections were among the most common and feared causes of death. From pneumonia to tuberculosis, and from wound infections to childhood diseases, humans lived in constant dread of microbial invaders. Even minor wounds could prove fatal, as untreated infections ravaged the body. In this context, the discovery of penicillin by Alexander Fleming in 1928 was nothing short of a revolution.
Penicillin, derived from the mold Penicillium notatum, became the first true antibiotic—a substance capable of killing bacteria without harming human cells. The miracle drug ushered in an era of medical optimism. Infections that once claimed lives became treatable with simple courses of antibiotics. Surgeries that had been perilous were now safer, and the development of antibiotics gave rise to modern medicine as we know it.
But the early promise of antibiotics came with an overlooked caveat. Just as bacteria were vulnerable to the effects of penicillin, they were also capable of adapting to it. Natural selection, the driving force of evolution, would inevitably favor the survival of any bacteria that could resist the drug.
How Antibiotic Resistance Works: A Battle of Survival
At its core, antibiotic resistance is a story of evolution. Bacteria, like all living organisms, are constantly evolving. When antibiotics are used to treat bacterial infections, they kill most of the bacteria. However, some bacteria, through random mutations or the acquisition of resistance genes, survive. These survivors multiply and pass on their resistant traits, making subsequent infections harder, or even impossible, to treat with the same antibiotic.
There are several mechanisms by which bacteria can develop resistance. Some bacteria produce enzymes that break down the antibiotic before it can do harm. Others may change their cell walls, preventing the antibiotic from entering. Some bacteria have developed pumps that actively expel the antibiotic from their cells. In rare cases, bacteria can even swap genetic material with each other, acquiring resistance genes from other bacteria, even those of different species.
What makes antibiotic resistance especially alarming is that it is not confined to one bacterial species. Resistance can spread across entire families of bacteria. For example, the gene responsible for resistance to penicillin can also confer resistance to other antibiotics, like cephalosporins and carbapenems, making it increasingly difficult to find effective treatments.
The Drivers of Antibiotic Resistance: A Global Phenomenon
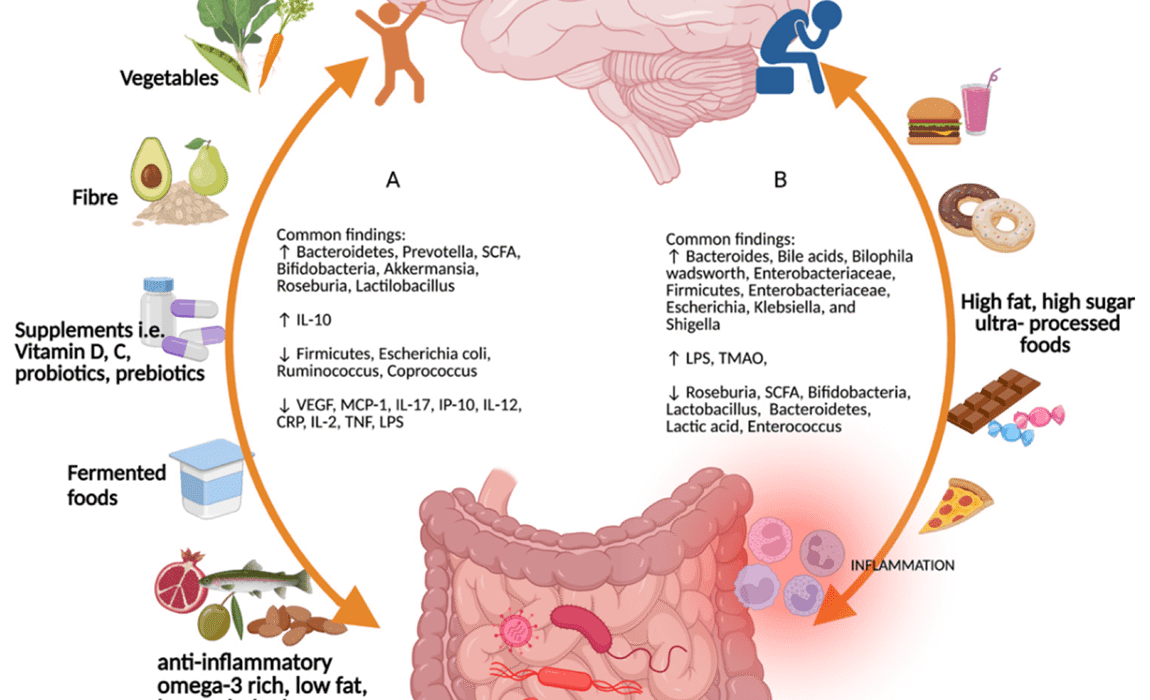
The rise of antibiotic resistance is a global issue, driven by several factors that are both biological and societal. The excessive use and misuse of antibiotics, particularly in humans and animals, have been the primary contributors to the emergence of resistant bacteria.
Overuse and Misuse in Medicine
One of the most significant drivers of antibiotic resistance is the overuse and misuse of antibiotics in human medicine. In many countries, antibiotics are prescribed too readily, often for viral infections like the common cold, against which antibiotics are ineffective. In some cases, patients demand antibiotics even when they are not needed, and doctors, under pressure, comply.
In addition, the incorrect use of antibiotics—such as not completing a full course of treatment or using suboptimal dosages—can promote resistance. If a patient stops taking antibiotics prematurely, the surviving bacteria may develop resistance. This is particularly problematic with chronic conditions, where antibiotics are prescribed for prolonged periods.
Antibiotics in Agriculture and Animal Farming
The use of antibiotics in agriculture, particularly in livestock farming, has become another major contributor to the spread of resistance. In many countries, antibiotics are used not just to treat illness in animals, but also to promote growth and prevent disease in healthy animals living in crowded, unsanitary conditions. This widespread use of antibiotics in agriculture creates a breeding ground for resistant bacteria.
These resistant bacteria can spread to humans through the consumption of contaminated meat, milk, or other animal products, as well as through environmental contamination from waste runoff from farms. In some cases, resistant bacteria can be transmitted directly to humans through close contact with animals or farm workers.
Global Travel and Trade
The interconnectedness of the modern world also plays a crucial role in the spread of antibiotic resistance. With the rise of global travel and trade, resistant bacteria can travel across borders in a matter of hours. International travelers may carry resistant strains of bacteria from one part of the world to another, while goods and foods can also serve as vehicles for bacteria.
This means that antibiotic resistance is not confined to one country or region. It is a global problem that requires global cooperation to address. Countries with strong healthcare systems may be able to contain outbreaks of resistant infections, but in less-developed regions with weaker healthcare infrastructure, antibiotic resistance can spread unchecked.
Environmental Contamination
Antibiotic resistance is also linked to environmental pollution. Pharmaceutical manufacturing processes, wastewater from hospitals, and agricultural runoff all contribute to the presence of antibiotics in the environment. When these antibiotics enter water systems, they can create hotspots where bacteria are exposed to sublethal levels of antibiotics, promoting resistance.
In fact, some studies have shown that antibiotic resistance can be detected in rivers, lakes, and other water bodies around the world. This environmental contamination is a growing concern, as it creates additional pathways for resistant bacteria to spread.
The Consequences of Antibiotic Resistance: A World Without Wonder Drugs
The consequences of antibiotic resistance are profound. In a world where antibiotics no longer work, medical procedures that are considered routine today could become deadly. Simple surgeries, organ transplants, cancer treatments, and even childbirth, which rely on antibiotics to prevent infections, could become high-risk procedures once again.
Infections that were once easily treatable will become more severe, and longer hospital stays will be required, further increasing the burden on healthcare systems. Common infections like pneumonia, urinary tract infections, and skin infections could once again become life-threatening.
In addition, antibiotic-resistant infections often require treatment with more expensive and less effective drugs, leading to longer periods of illness and increased healthcare costs. The economic burden of antibiotic resistance is already significant, and it is expected to grow exponentially in the coming years.
The Global Response: The Race to Combat Resistance
Recognizing the urgent nature of the problem, countries around the world are taking action to combat antibiotic resistance. In 2015, the World Health Organization (WHO) launched the Global Action Plan on Antimicrobial Resistance, calling for a coordinated global response to the crisis. The plan aims to strengthen regulations and policies regarding antibiotic use, improve infection prevention and control measures, and foster better stewardship of antibiotics.
In addition, governments are funding research into new antibiotics and alternative treatments. However, the development of new antibiotics has slowed in recent years, largely due to economic factors and the scientific challenges involved in discovering drugs that can outsmart resistant bacteria.
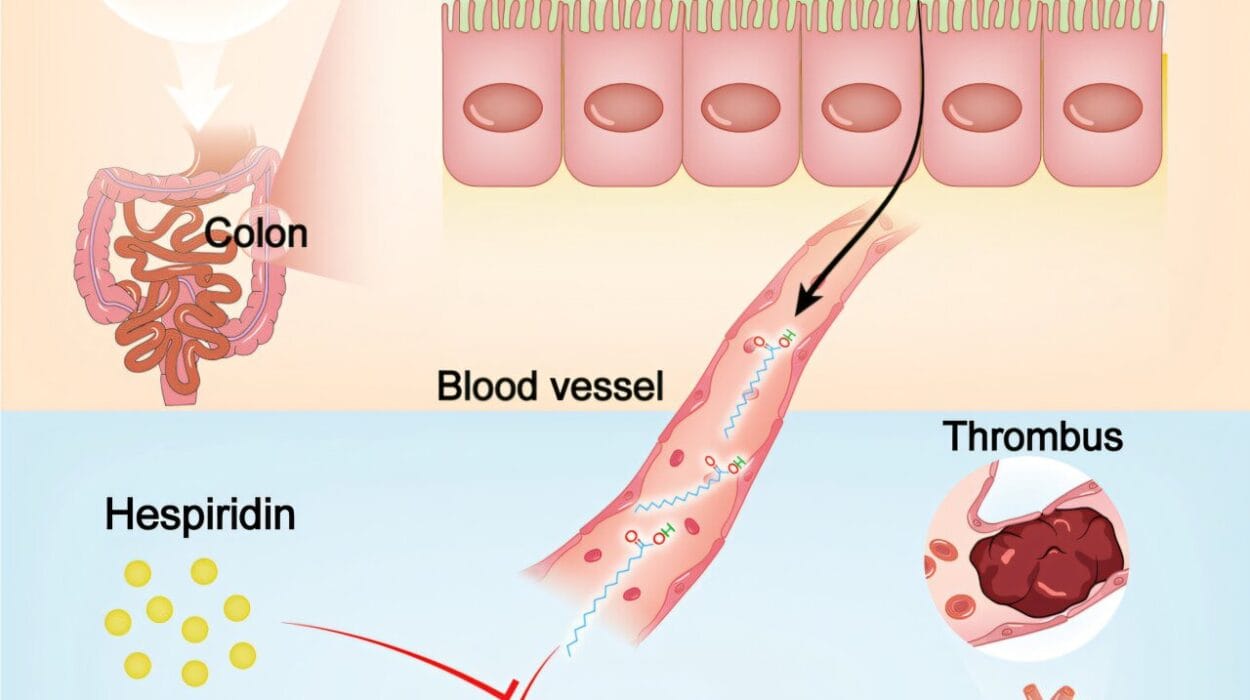
One promising avenue of research involves bacteriophage therapy, which uses viruses that infect and kill bacteria. This approach offers a potential alternative to traditional antibiotics, though more research is needed to understand its safety and efficacy.
Public education campaigns are also a critical part of the global response. Raising awareness about the proper use of antibiotics, as well as the risks of overuse, is essential in changing behavior. Encouraging patients to complete their antibiotic courses and to seek medical advice before demanding antibiotics can help slow the spread of resistance.
Looking Ahead: A Call to Action
The battle against antibiotic resistance is far from over, and the clock is ticking. Scientists, healthcare professionals, and governments must work together to develop new antibiotics, enforce better practices in both human medicine and agriculture, and promote global cooperation in the fight against this silent pandemic.
The global threat of antibiotic resistance is not a future problem—it is here, and it is growing. But with concerted effort, we can still mitigate the damage. If we take swift, decisive action now, we may be able to preserve the life-saving power of antibiotics for future generations. The world has faced crises before, but none quite like this. It is up to all of us to rise to the challenge, before it is too late.