Everywhere you turn today, someone is tired. Not just garden-variety tired, but deeply, soul-wearily exhausted. People wake up tired, yawn through the workday, and collapse into bed at night only to sleep restlessly and wake up feeling just as depleted. And it’s not just a few overworked professionals or parents of newborns—millions are reporting this persistent fatigue with no obvious cause.
Enter adrenal fatigue, a term that has swept across wellness blogs, health podcasts, and even some doctor’s offices. The concept has become a catch-all explanation for a host of vague symptoms: fatigue, brain fog, mood swings, salt cravings, insomnia, dizziness, and difficulty coping with stress. It seems like a convenient and comforting label—finally, a name for what people are feeling. But is adrenal fatigue a real medical condition or a seductive myth rooted in pseudoscience?
The Role of the Adrenal Glands
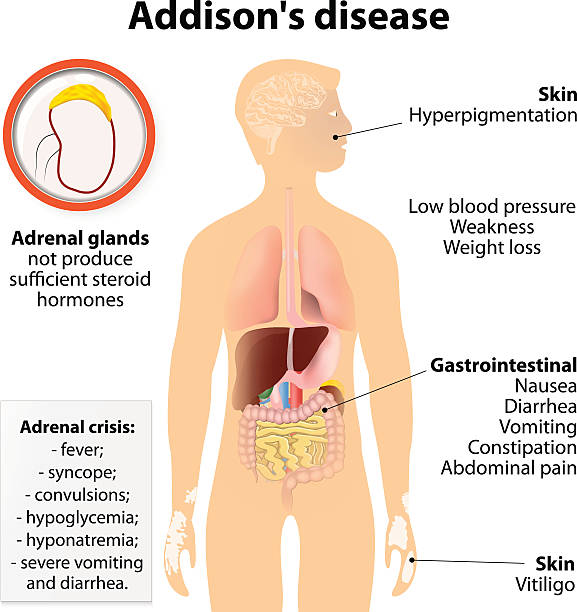
To evaluate whether adrenal fatigue holds water as a legitimate diagnosis, it helps to understand what the adrenal glands actually do. These small, triangular organs sit atop your kidneys like tiny pyramids and are crucial players in your body’s endocrine system. They produce a variety of hormones, including cortisol, adrenaline (epinephrine), norepinephrine, and aldosterone.
Cortisol, in particular, is the star of this hormonal ensemble. Often called the “stress hormone,” it plays a central role in your body’s response to stress, regulating blood pressure, metabolism, immune function, and blood sugar levels. When you’re confronted with a threat—whether a hungry lion or a looming deadline—your adrenal glands pump out cortisol and adrenaline to initiate the fight-or-flight response.
Once the danger has passed, cortisol levels drop and your body returns to a state of balance. In theory, adrenal fatigue occurs when chronic stress forces the adrenal glands to churn out cortisol constantly, eventually “exhausting” them to the point of underperformance. As the narrative goes, your adrenal glands become fatigued, like overworked employees who start slacking off after too much overtime.
The Origin of the Adrenal Fatigue Theory
The term “adrenal fatigue” was first popularized in 1998 by Dr. James Wilson, a chiropractor and naturopath, in his book Adrenal Fatigue: The 21st Century Stress Syndrome. In it, he described a new condition afflicting people in high-stress environments—those with relentless workloads, poor sleep, and modern anxieties.
Wilson claimed that persistent stress leads to suboptimal adrenal function and a drop in cortisol production, resulting in chronic tiredness and a constellation of other symptoms. His book offered diagnostic quizzes and protocols for recovery involving lifestyle changes, stress management, and supplements marketed as adrenal boosters.
The idea resonated deeply with people. It offered a plausible biological explanation for a common but frustrating experience. It also offered solutions—herbs, vitamins, rest, and specific diets—that seemed more holistic and manageable than prescription medications or vague reassurance from doctors.
Yet, from the standpoint of mainstream medical science, adrenal fatigue was—and still is—an unrecognized diagnosis.
What the Medical Establishment Says
Ask an endocrinologist about adrenal fatigue, and you’re likely to get a raised eyebrow or a gentle eye roll. The term does not appear in any major medical textbooks, nor is it recognized by the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), or the Endocrine Society.
From a clinical perspective, adrenal dysfunction is a very real phenomenon—but it manifests as specific, well-defined conditions. The most notable is Addison’s disease, also called primary adrenal insufficiency, which occurs when the adrenal glands are damaged and cannot produce enough cortisol. This condition is rare, affecting roughly 1 in 100,000 people, and has distinct diagnostic criteria and lab markers, including very low cortisol levels and elevated ACTH (a hormone from the pituitary gland that stimulates the adrenals).
Secondary adrenal insufficiency can also occur when the pituitary gland fails to signal the adrenals, often due to steroid withdrawal or pituitary tumors. Again, this is a clear-cut diagnosis with measurable hormonal disruptions.
But adrenal fatigue, as described by Dr. Wilson, exists in a murky gray zone. The theory posits that the adrenal glands can be partially worn out—not diseased, not healthy, just sluggish. However, there is no scientific consensus that this happens. Numerous studies have attempted to detect changes in cortisol levels among individuals diagnosed with adrenal fatigue by alternative practitioners, but results have been inconclusive or contradictory.
The Trouble with Cortisol Testing
One of the main arguments used to support adrenal fatigue is cortisol testing, typically performed through saliva samples taken at multiple times throughout the day. These tests are often used by functional medicine practitioners to show “flattened” cortisol curves—a supposed sign of adrenal burnout.
However, interpreting cortisol rhythms is far from straightforward. Cortisol naturally fluctuates during the day, rising in the early morning and tapering off at night. Many factors—poor sleep, blood sugar dips, medications, even time of sampling—can influence levels. Moreover, slight variations in cortisol output are normal and do not necessarily indicate adrenal dysfunction.
In peer-reviewed studies, researchers have found that people reporting symptoms of adrenal fatigue often had normal cortisol levels or levels that varied within the normal range. Even when cortisol levels were slightly low or blunted, they did not correspond consistently with symptoms. In other words, you can feel exhausted and still have perfectly functioning adrenal glands.
The Vague Allure of a Catch-All Diagnosis
So why does adrenal fatigue continue to thrive in popular discourse despite the lack of clinical validation? Part of the answer lies in the frustration many people feel when they seek medical help for symptoms like fatigue, insomnia, and low motivation—and are told nothing is wrong.
Conventional medicine is excellent at diagnosing diseases but often poor at addressing subclinical conditions or nuanced imbalances. If your blood tests come back normal and your thyroid function checks out, you may be told that your fatigue is “just stress,” or worse, that it’s all in your head.
In contrast, the adrenal fatigue narrative offers validation and explanation. It provides a name for a suffering that feels very real. It also promises agency. You can “heal your adrenals” through natural remedies, stress reduction, and better habits—strategies that feel empowering compared to being handed an antidepressant or a shrug.
There’s also a psychological comfort in believing that your body is tired because it’s trying to protect you from too much stress. In a society that prizes constant productivity, being able to say, “My adrenals are exhausted” offers a respectable excuse to slow down.
What Science Suggests Is Really Happening
While adrenal fatigue itself may be a medical mirage, the symptoms people report are undeniably real. Chronic fatigue, poor stress resilience, brain fog, and irritability are legitimate experiences—and they deserve legitimate inquiry.
One of the leading explanations for these symptoms is not adrenal burnout but HPA axis dysregulation. The HPA axis—short for hypothalamic-pituitary-adrenal axis—is a complex feedback loop that governs your body’s stress response. It’s more accurate to think of this system as a thermostat than a battery. Rather than wearing out, it can become imbalanced or hypersensitive over time due to chronic stress, poor sleep, trauma, or systemic inflammation.
In this framework, the problem isn’t that your adrenal glands are fatigued—it’s that the brain signals regulating them are maladapted. This can lead to disrupted cortisol rhythms, exaggerated or blunted responses to stress, and changes in energy regulation. These shifts can mimic the symptoms described in adrenal fatigue—but with a more nuanced biological explanation.
Additionally, many cases of so-called adrenal fatigue may be better understood through the lens of other overlooked or underdiagnosed conditions. These include:
- Sleep disorders such as sleep apnea
- Chronic infections like Lyme disease or Epstein-Barr virus
- Thyroid dysfunction, especially subclinical hypothyroidism
- Depression or anxiety
- Nutrient deficiencies, particularly B12, iron, or magnesium
- Blood sugar dysregulation or insulin resistance
Each of these conditions can cause fatigue and related symptoms, and many are not routinely tested for in standard exams.
The Importance of Listening to the Body
Regardless of whether adrenal fatigue is a real diagnosis, its popularity speaks to a deeper truth: people are tired, and they’re not being heard. The modern lifestyle—with its relentless pace, digital overload, and chronic stress—is biologically unsustainable. The body was not designed to be constantly on high alert. Over time, the stress-response system begins to fray, leading to real physiological consequences.
What people are describing when they talk about adrenal fatigue may be the body’s cry for balance. It may not be adrenal glands collapsing under pressure, but a signal from the nervous system that the tempo of life has become too fast, too loud, too unrelenting.
The interventions often recommended for adrenal fatigue—more sleep, better nutrition, gentle exercise, mindfulness, reduced caffeine, and prioritizing rest—are not just placebos. They’re legitimate ways to support the HPA axis, improve metabolic health, and recalibrate the stress response.
In that sense, even if the diagnosis is flawed, the prescriptions are often wise.
Toward a New Paradigm of Fatigue
Rather than clinging to a contested label like adrenal fatigue, some clinicians and researchers are pushing for a more precise and holistic understanding of chronic fatigue. Terms like “stress-related exhaustion,” “allostatic overload,” and “HPA axis dysfunction” are gaining traction in academic literature. These terms reflect the complexity of the body’s stress systems and avoid the misleading notion that the adrenal glands themselves are tiring out.
This newer model emphasizes the role of the brain-body connection, gut health, inflammation, mitochondrial function, and circadian rhythms. It acknowledges that fatigue is not just a matter of hormone levels but of systemic imbalance.
Importantly, it also invites a more compassionate, less stigmatizing view of people suffering from chronic fatigue. Rather than dismissing them or overmedicalizing them, it encourages clinicians to look deeper, listen more, and treat the whole person.
The Final Word on Adrenal Fatigue
In the end, adrenal fatigue may be best understood not as a literal condition but as a metaphor—a symbolic name for a very real constellation of modern malaise. It captures the feeling of being burnt out, overextended, and hormonally off-kilter. But science demands precision, and as far as current evidence shows, the adrenal glands themselves are not the villains.
Still, that doesn’t mean people are imagining their symptoms. Far from it. They are simply looking for answers in a medical landscape that often fails to meet them where they are.
The true challenge for modern medicine is not to dismiss adrenal fatigue as pseudoscience and walk away—but to investigate the underlying causes of chronic fatigue with the same curiosity and rigor we apply to other conditions. That means funding better research, improving diagnostics, and expanding our definition of what it means to be unwell.
Until then, people will continue to search for answers, and adrenal fatigue will continue to be a cultural touchstone—a signpost pointing toward something our medical systems have yet to fully understand.