Inside the human body, a symphony of hormones plays a silent, complex melody that dictates how we grow, sleep, reproduce, and function. These chemical messengers float through the bloodstream, orchestrating everything from metabolism to mood. When just one hormone is out of tune, the entire performance can go awry. Among the most common and perplexing hormonal disorders affecting women worldwide is polycystic ovary syndrome, better known as PCOS.
PCOS is more than a reproductive condition. It is a complex hormonal imbalance that touches nearly every part of the body, from the ovaries to the skin to the brain. Affecting at least one in ten women of reproductive age—and potentially many more who remain undiagnosed—it’s a syndrome shrouded in confusion, often misdiagnosed or misunderstood. Yet understanding PCOS is crucial not just for women’s health but for broader conversations about chronic disease, fertility, metabolism, and even mental health.
The Origins of a Syndrome Hidden in Plain Sight
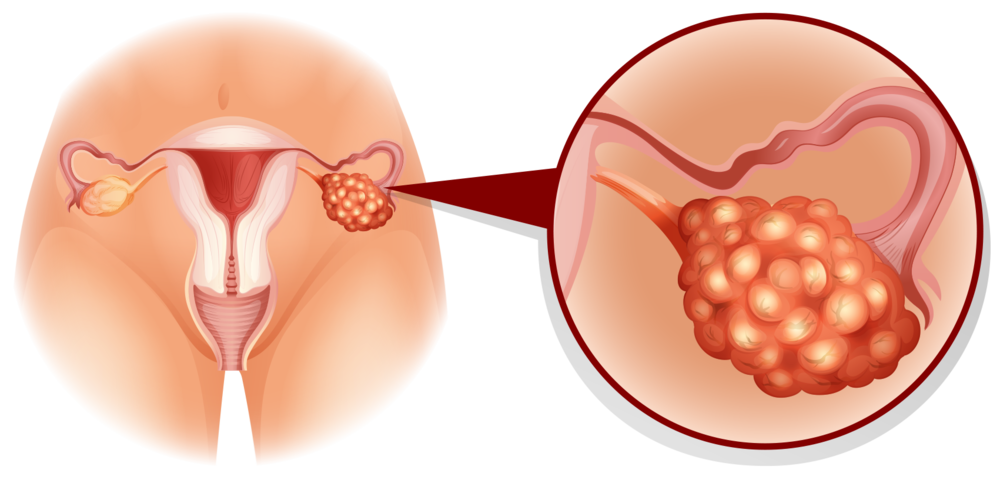
Polycystic ovary syndrome got its name from a peculiar feature often seen on ultrasound scans: ovaries with a ring of small fluid-filled sacs, or cysts, resembling a string of pearls. But the name is misleading. Not all women with PCOS have these cysts, and having cysts doesn’t necessarily mean you have PCOS.
The earliest medical descriptions of this condition go back to the 1930s when gynecologists Irving Stein and Michael Leventhal first linked a pattern of symptoms—irregular menstrual cycles, infertility, and enlarged ovaries—to what they called “sclerocystic ovaries.” Since then, the name has evolved, but the condition remains as complex as ever.
PCOS is not a single disease with a single cause. Rather, it is a syndrome—a cluster of signs and symptoms that can vary widely between individuals. This variability is part of what makes it so challenging to diagnose and treat. No two cases are exactly alike, yet the underlying disruption is typically hormonal in nature, affecting systems far beyond the ovaries.
How the Hormonal Puzzle Unfolds
At its core, PCOS is a disorder of hormonal regulation. The most notable hormonal hallmark is an excess of androgens, commonly known as male hormones, such as testosterone. While it’s normal for women to produce small amounts of androgens, in PCOS, these levels are elevated, leading to a variety of effects.
High androgen levels can disrupt the menstrual cycle by interfering with the development and release of eggs from the ovaries. This leads to irregular or absent periods and can cause difficulty with ovulation and fertility. Androgens also affect other tissues, contributing to symptoms like acne, excessive hair growth on the face and body (known as hirsutism), and hair thinning on the scalp.
But androgens are only one piece of the hormonal puzzle. Many women with PCOS also show signs of insulin resistance, meaning their bodies have trouble using insulin effectively. Insulin is the hormone that regulates blood sugar. When cells become resistant to insulin, the pancreas compensates by producing more of it. This excess insulin can trigger the ovaries to produce more androgens, creating a vicious cycle.
This interplay between insulin and androgens is thought to be a central driver of PCOS in many women. It also links PCOS to other health concerns such as weight gain, type 2 diabetes, and cardiovascular disease.
Recognizing the Many Faces of PCOS
There is no single way that PCOS presents itself. One woman may struggle with painful acne and hair growth while having regular periods, while another may have no visible symptoms but find out she has PCOS after struggling to conceive. Still another may be diagnosed only after developing metabolic issues like high blood sugar or cholesterol.
The diagnostic criteria for PCOS reflect this diversity. According to the widely accepted Rotterdam criteria, a woman must have at least two of the following three features to be diagnosed with PCOS:
- Irregular or absent ovulation
- Signs of elevated androgens, either clinically (e.g., acne, hirsutism) or through blood tests
- Polycystic-appearing ovaries on ultrasound
Other conditions that can mimic these symptoms must also be ruled out, including thyroid disorders, adrenal tumors, and elevated prolactin levels. This process can take time and patience, and many women experience years of symptoms before receiving a correct diagnosis.
The Impact on Fertility and Reproductive Health
One of the most well-known consequences of PCOS is its effect on fertility. Because ovulation is often irregular or absent, many women with PCOS have trouble conceiving. But having PCOS does not mean infertility is inevitable. Many women with the condition go on to have healthy pregnancies, sometimes with the help of ovulation-inducing medications or lifestyle changes.
Beyond fertility, PCOS can impact other aspects of reproductive health. It is associated with a higher risk of miscarriage, pregnancy complications such as gestational diabetes and preeclampsia, and long-term risks like endometrial hyperplasia, a thickening of the uterine lining that can lead to cancer if left untreated. These risks are often tied to prolonged irregular cycles and lack of progesterone exposure due to infrequent ovulation.
Early diagnosis and treatment can help mitigate these risks, but awareness remains a barrier. In many cases, women are told to wait until they try to conceive before addressing PCOS—missing critical windows for intervention.
The Invisible Burden on Mental and Emotional Health
PCOS does not just affect the body. It also takes a toll on the mind. Numerous studies have shown that women with PCOS are at increased risk for depression, anxiety, and body image distress. This is not simply due to cosmetic symptoms like acne or weight gain—though those can be distressing—but also due to the chronic nature of the condition, the uncertainty around fertility, and the emotional fatigue of navigating an often misunderstood diagnosis.
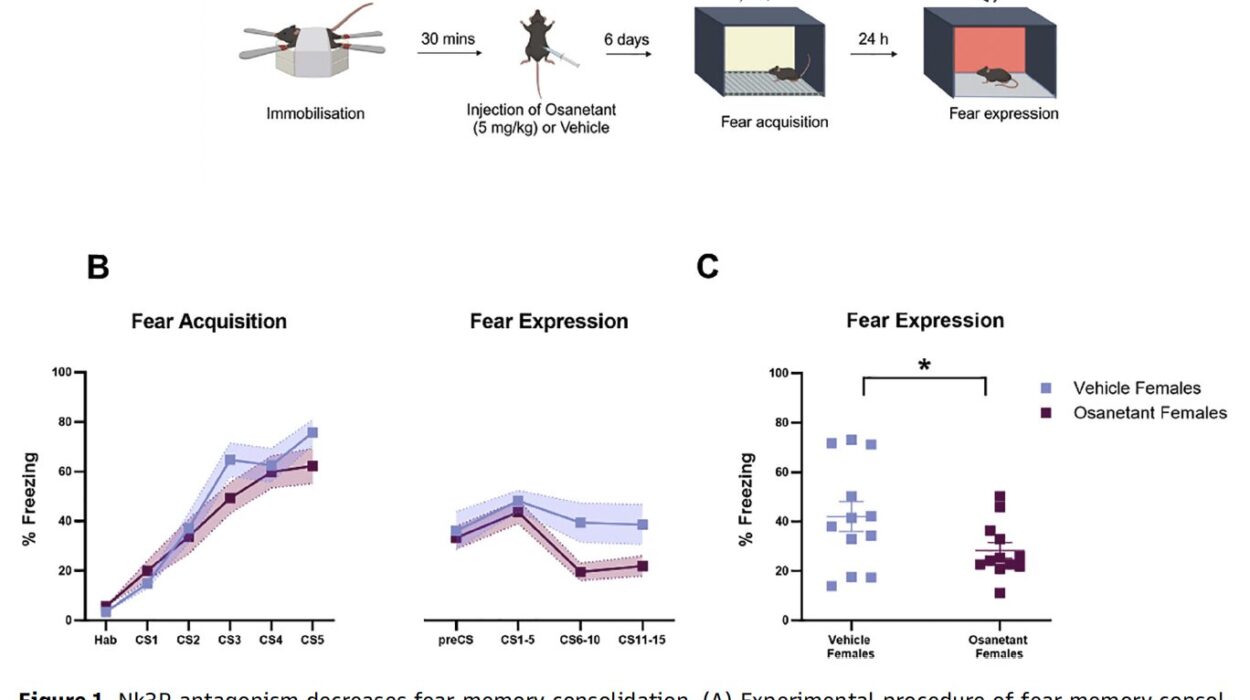
Hormonal imbalances themselves may also contribute to mood disorders. For example, insulin resistance and inflammation—both common in PCOS—are linked to altered neurotransmitter activity and increased risk of depression. Some researchers have also speculated about a possible connection between PCOS and neurodivergent conditions like ADHD, particularly given shared features such as dopamine dysregulation.
Despite these known links, mental health support is rarely emphasized in PCOS care. Too often, women are told to lose weight or take birth control without addressing the deeper psychological impact of living with a chronic hormonal disorder. A more holistic approach is urgently needed—one that recognizes the mind-body connection and incorporates mental health into the treatment plan.
Why Weight Is Not the Whole Story
One of the most frustrating aspects of PCOS is the way it is often reduced to a problem of weight. Many women are told that their symptoms will improve if they lose weight, and while there is truth to the idea that weight loss can help regulate cycles and improve insulin sensitivity, this advice is often oversimplified and poorly delivered.
First, not all women with PCOS are overweight. Up to 30 percent have what’s called “lean PCOS”—they may appear slim but still have significant hormonal dysfunction and metabolic issues. Second, weight gain in PCOS is often a symptom, not just a cause. Insulin resistance, high androgens, and low-grade inflammation all promote fat storage, particularly around the abdomen.
Third, and perhaps most importantly, shaming women about their weight or prescribing rigid diets rarely leads to long-term success. What’s needed is a nuanced, compassionate understanding of how PCOS interacts with metabolism and appetite regulation, including the role of stress, sleep, and environmental toxins in weight and hormone balance.
Navigating Treatment Options and Medical Advice
There is no cure for PCOS, but there are many tools available to manage its symptoms and reduce long-term health risks. The right treatment plan depends on a woman’s individual goals—whether she is trying to conceive, control acne, regulate her cycles, or prevent diabetes.
One common approach is the use of hormonal birth control to regulate periods and reduce androgen levels. Combined oral contraceptives can help lower testosterone and improve acne and hirsutism. However, they do not address the root causes of PCOS and are not suitable for everyone, especially those with certain risk factors for blood clots or high blood pressure.
Another widely used medication is metformin, an insulin-sensitizing drug originally developed for type 2 diabetes. It can help reduce insulin levels, restore ovulation, and lower androgen production. Some women also benefit from medications like spironolactone (which blocks androgen receptors), inositol supplements (which improve insulin signaling), or newer approaches such as GLP-1 receptor agonists.
Lifestyle interventions remain a cornerstone of PCOS management. Regular physical activity, balanced nutrition, stress reduction, and sleep hygiene can all improve hormonal balance. But again, these recommendations must be tailored, realistic, and supportive—recognizing the unique challenges women with PCOS face.
The Role of Inflammation and the Gut Microbiome
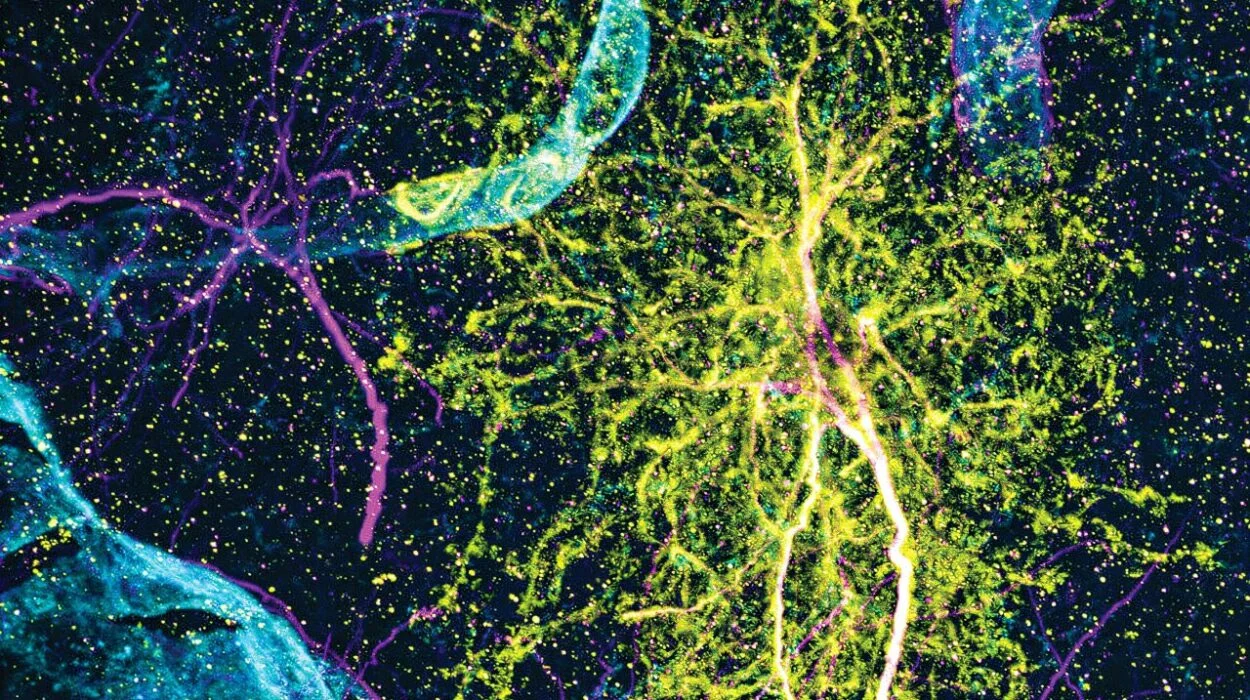
Emerging research suggests that inflammation and gut health play a pivotal role in the development and progression of PCOS. Low-grade chronic inflammation is commonly observed in women with the condition, and it may contribute to both insulin resistance and increased androgen production.
The gut microbiome—the community of trillions of microbes living in the intestines—also appears to be altered in PCOS. Dysbiosis, or microbial imbalance, may impair metabolism and hormone regulation, promoting weight gain and inflammation. Some studies have even shown that transplanting gut bacteria from women with PCOS into mice can induce PCOS-like symptoms.
This area of research is still young, but it opens up exciting possibilities. Could probiotics, prebiotics, or dietary changes that support gut health play a role in PCOS treatment? Could anti-inflammatory strategies, from omega-3s to mindfulness practices, help break the cycle of hormone dysfunction? As science continues to evolve, these questions are likely to lead to new, more integrative approaches to care.
PCOS as a Lifelong Condition
While PCOS is often diagnosed in adolescence or early adulthood, it does not disappear with age. Its manifestations may change over time—fertility issues may give way to metabolic concerns, and acne may fade while insulin resistance worsens—but the underlying hormonal imbalance persists.
Women with PCOS are at increased risk of developing type 2 diabetes, cardiovascular disease, and endometrial cancer. They may also face challenges during menopause, when shifting estrogen levels further alter the hormonal landscape. Yet because PCOS is seen primarily as a reproductive disorder, many women lose access to care or attention once they are no longer trying to conceive.
This is a major oversight. PCOS should be recognized and treated as a chronic, systemic condition requiring lifelong monitoring and support. That means regular screening for diabetes and cholesterol, attention to mood and mental health, and a healthcare system that listens, validates, and adapts.
The Importance of Advocacy and Awareness
In recent years, the voices of women with PCOS have grown louder. Online communities, advocacy groups, and research collaborations are shining a light on the condition and demanding better care. September is now recognized as PCOS Awareness Month, and social media is helping spread knowledge and solidarity.
Still, much work remains. Research funding for PCOS lags behind that of other chronic conditions, despite its prevalence. Medical education often glosses over it. And too many women still go years without a diagnosis, told that their symptoms are “normal” or “all in their head.”
Breaking this silence requires not just better science, but better storytelling. Women with PCOS must be empowered to share their experiences, ask hard questions, and advocate for themselves in the doctor’s office. Clinicians must be willing to listen, to treat patients as partners, and to see beyond weight and reproduction.
Looking Toward the Future of PCOS Research
The future of PCOS care lies in personalization. As we learn more about the genetic, environmental, and epigenetic factors that shape this condition, we will move closer to individualized treatments—ones that target the root causes in each woman rather than relying on a one-size-fits-all approach.
Advances in genomics, microbiome science, metabolomics, and hormone testing may allow for earlier detection and more precise interventions. Artificial intelligence and machine learning could help identify subtypes of PCOS and predict which therapies will work best for which patients. Integrative models that combine medical, nutritional, psychological, and environmental perspectives will pave the way for more holistic healing.
A Syndrome Worth Understanding
Polycystic ovary syndrome is not just a “women’s issue.” It is a mirror reflecting deeper truths about how we understand hormones, metabolism, gender, and chronic illness. It is a challenge to the medical status quo, a call for more inclusive science, and a reminder that the body is not a machine but a living, dynamic system.
To understand PCOS is to see the complexity of human biology up close—and to recognize the resilience of those who live with it every day. For the millions of women affected by PCOS, knowledge is power. And in that knowledge lies the hope of better treatments, more compassionate care, and a future in which no one has to suffer in silence.