For many women, the days leading up to their period can bring a familiar suite of symptoms: mood swings, cravings, fatigue, irritability, maybe some cramping or bloating. It’s the classic premenstrual syndrome, better known as PMS, and while not exactly welcome, it’s expected—like a moody old friend who drops by once a month.
But for some women, this monthly shift is something altogether different. The symptoms don’t just cause discomfort—they derail. They’re not just inconvenient—they’re debilitating. They don’t pass with a bowl of chocolate ice cream and a hot bath—they tear through daily life like an emotional tornado, leaving chaos in their wake. This is not PMS. This is something deeper, more intense, and often misunderstood. This is PMDD—Premenstrual Dysphoric Disorder.
To the casual observer, PMS and PMDD might look like two shades of the same monthly storm. But for the women living with PMDD, the difference isn’t subtle—it’s seismic. Understanding what sets them apart is essential for awareness, empathy, and proper medical care.
Peeling Back the Acronyms: Defining PMDD
PMDD stands for Premenstrual Dysphoric Disorder, and despite being described in medical literature for decades, it’s only recently gained traction in both public discourse and clinical practice. The disorder is characterized by severe emotional and physical symptoms that begin in the luteal phase of the menstrual cycle—the period between ovulation and menstruation—and resolve shortly after menstruation begins.
These aren’t mild symptoms. They are intense, intrusive, and life-disrupting. Women with PMDD may experience overwhelming depression, anxiety, anger, or irritability, often to the point where personal relationships suffer, work becomes unmanageable, and life feels out of control. It’s as if a hormonal switch flips, and suddenly, the brain and body turn against them.
The key distinction between PMDD and PMS lies in this severity. While PMS can be uncomfortable and annoying, PMDD is often described as unbearable. It’s not a matter of “just dealing with it”—many women with PMDD report that they feel like a different person for a week or two every month. Some compare it to a Jekyll-and-Hyde transformation that recurs relentlessly, cycling with cruel regularity.
A Complex Web of Hormones and Sensitivities
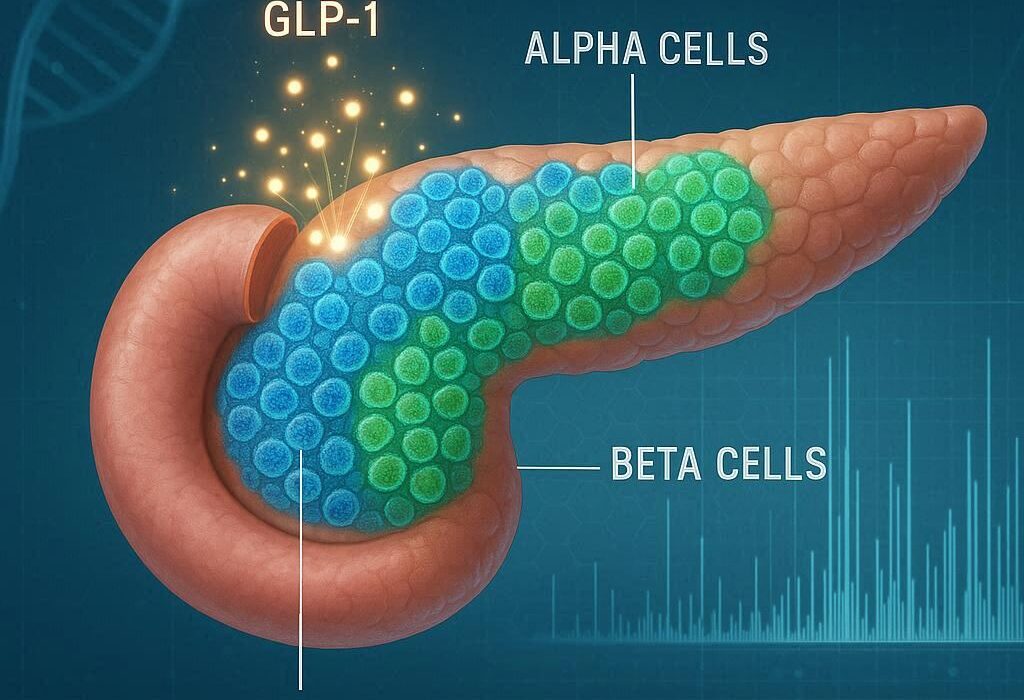
Both PMS and PMDD are rooted in the hormonal changes that occur during the menstrual cycle, particularly after ovulation. Estrogen and progesterone levels fluctuate naturally, but not everyone’s body responds to those shifts the same way. For reasons still being unraveled by science, women with PMDD appear to have an abnormal sensitivity to these normal hormonal changes.
It’s not about having too much or too little hormone—it’s about how the brain reacts to them. Research suggests that women with PMDD may have a heightened response in certain brain systems, particularly those involving serotonin, the neurotransmitter often linked to mood regulation. The result? Even small hormonal shifts can trigger dramatic mood changes.
This helps explain why PMDD is not simply “worse PMS.” It’s not just a matter of exaggerated symptoms—it’s a distinct biological response to hormonal changes, one that affects the central nervous system and can lead to profound emotional instability.
Mental Health Meets Menstrual Health
One of the more insidious aspects of PMDD is how easily it can be misdiagnosed. Women who seek help for PMDD symptoms are sometimes told they have depression, anxiety, bipolar disorder, or borderline personality disorder. These diagnoses can stick, especially if the doctor doesn’t ask about menstrual patterns or fails to recognize the cyclical nature of the symptoms.
This overlap with psychiatric conditions isn’t surprising—after all, PMDD often presents as a mental health crisis. Suicidal thoughts, panic attacks, irrational anger, and crushing sadness can all be part of the picture. But the cyclical timing is key. Unlike chronic mood disorders, PMDD symptoms appear only during the luteal phase and disappear within a few days of menstruation beginning. The rest of the month, the woman may feel perfectly fine—happy, stable, productive, content.
This back-and-forth can be incredibly confusing and distressing for women who don’t understand what’s happening to them. It’s not uncommon for them to doubt their own sanity, especially when the medical community is slow to connect the dots. That’s why education and awareness are crucial—not just for patients, but for doctors, therapists, and anyone involved in women’s health.
A Different Kind of Suffering
To understand how PMDD differs from PMS, it’s helpful to listen to the women who experience it. They describe waking up and knowing something is off—feeling a sudden shift in their emotional landscape. A sense of dread creeps in, even when nothing is wrong. Everyday tasks start to feel impossible. Small annoyances ignite disproportionate rage. A passing comment from a coworker might spiral into feelings of worthlessness. The world takes on a dark hue, and they can’t figure out why.
Some women describe it as feeling possessed, as though a foreign force has taken over their mind. Others liken it to living two separate lives—one functional, and one fractured. They anticipate the arrival of the “PMDD self” each month and dread its inevitable return.
PMS, on the other hand, may involve irritability, sadness, and discomfort, but rarely does it reach this level of psychological intensity. While PMS might make you snap at your partner or cry during a sad commercial, PMDD can make you question whether life is worth living. The distinction isn’t just quantitative—it’s qualitative. The kind of suffering involved in PMDD is of a different order altogether.
When the Body Betrays the Brain
PMDD is, at its core, a disorder of mood regulation. But it’s also a deeply physical experience. Many women with PMDD report physical symptoms such as joint or muscle pain, breast tenderness, fatigue, bloating, headaches, and sleep disturbances. But it’s the emotional symptoms—especially the dramatic mood swings, depression, and anger—that cause the most turmoil.
The sense of betrayal is real. How can your own body do this to you? Why would your brain suddenly revolt every few weeks? These questions torment many PMDD sufferers, especially when their symptoms are dismissed or downplayed by those around them. “It’s just your period,” they’re told. “All women deal with this.”
Except, they don’t. Not like this. And minimizing PMDD only deepens the isolation and shame.
The Long Road to Diagnosis
Despite affecting up to 5–8% of menstruating women, PMDD often goes undiagnosed for years. Many women spend a decade or more bouncing between doctors, therapists, and prescriptions before someone finally connects their symptoms to their menstrual cycle. The process of diagnosis requires careful tracking of symptoms over at least two consecutive cycles, ideally with a tool like the Daily Record of Severity of Problems (DRSP), which helps distinguish PMDD from other mood disorders.
This tracking process is both empowering and validating. For many women, it’s the first time they’re able to see the pattern clearly: how their mood changes like clockwork each month, how the fog lifts after their period, how the pattern repeats with maddening consistency. It’s not all in their head—it’s in their hormones, their neurobiology, their cycle.
Getting a diagnosis can be a turning point. It brings clarity, relief, and the possibility of targeted treatment. But the road to that moment is often long, lonely, and riddled with misunderstanding.
Treatment That Looks Beyond the Surface
There is no one-size-fits-all treatment for PMDD, but there are a variety of options that can help manage symptoms. One of the most commonly prescribed treatments is selective serotonin reuptake inhibitors (SSRIs), a class of antidepressants that can be particularly effective for PMDD—even when taken only during the luteal phase. This suggests that serotonin plays a significant role in the disorder and underscores its neurological basis.
Hormonal treatments are another avenue. Birth control pills that suppress ovulation can stabilize hormonal fluctuations and reduce PMDD symptoms in some women. In more severe cases, medications that shut down the menstrual cycle entirely—such as gonadotropin-releasing hormone (GnRH) agonists—can be used. These induce a temporary menopause, which is not a light decision but can bring dramatic relief.
Lifestyle changes can also play a supportive role. Regular exercise, stress management techniques, dietary adjustments, and adequate sleep all help regulate mood and improve overall well-being. Cognitive-behavioral therapy (CBT) is another evidence-based approach that helps women cope with the emotional rollercoaster and develop tools for managing symptoms.
In extreme cases where all other treatments fail, some women opt for surgery to remove the ovaries—a procedure known as oophorectomy. This is a drastic and irreversible step, but for some, it’s the only way to reclaim their quality of life.
The Cultural Blind Spot Around PMDD
Despite the severity of the condition, PMDD remains shrouded in misunderstanding and stigma. Part of the problem is cultural: menstruation is still a taboo subject in many societies, often treated with discomfort, secrecy, or shame. As a result, conditions related to the menstrual cycle are under-researched, underfunded, and underdiagnosed.
When women do speak up about severe premenstrual symptoms, they’re often dismissed as overly emotional or attention-seeking. This silencing has serious consequences. It delays diagnosis, impedes treatment, and perpetuates a culture in which women’s suffering is normalized—or worse, ridiculed.
PMDD is not a punchline. It’s a legitimate medical disorder that can have a profound impact on mental health, personal relationships, and quality of life. Recognizing it as such is a necessary step toward better care and deeper empathy.
Living With PMDD: Stories of Resilience
Despite the challenges, many women living with PMDD find ways to navigate their condition with strength, insight, and resilience. They become fierce advocates for their own health, educating themselves about their bodies and pushing for the care they need. They form online communities, share resources, and offer support to others who are just beginning to recognize their symptoms.
Some choose to embrace a slower rhythm during the luteal phase, building rest into their routines and communicating openly with loved ones. Others rely on a combination of medication, therapy, and self-care rituals to maintain balance. Every journey is different, but the common thread is this: PMDD does not define them. It’s a part of their story—but not the whole story.
There is strength in naming what you’re going through. There is power in tracking your symptoms, seeking treatment, and speaking out. And there is healing in being believed.
The Future of PMDD Awareness
As awareness of PMDD continues to grow, so too does the hope for better treatments, earlier diagnosis, and more compassionate care. Research is beginning to uncover the genetic, neurological, and hormonal underpinnings of the disorder. Advocacy groups are pushing for PMDD to be recognized in medical training and public health initiatives. And women everywhere are finding their voice, challenging the silence, and demanding to be heard.
The path ahead isn’t easy. But it is illuminated by knowledge, solidarity, and the refusal to accept unnecessary suffering. PMDD may be a formidable opponent, but it is not invincible. With the right tools, support, and understanding, women can—and do—reclaim their lives from its grip.
Closing the Gap Between PMS and PMDD
To the untrained eye, PMS and PMDD might look like different points on the same spectrum. But the difference is more than just degree—it’s kind. PMS is a common, manageable part of many women’s lives. PMDD is a serious, life-altering condition that deserves clinical attention and compassionate support.
Recognizing that difference is not just about semantics—it’s about survival. It’s about seeing the women who feel invisible, hearing the voices that have been ignored, and creating a world in which no one has to suffer in silence.
PMDD is real. It’s painful. But it’s also treatable. And perhaps most importantly, it’s finally being seen for what it is—not a weakness, not a drama, but a disorder worth understanding, treating, and healing.